Research Article Open Access
Mucosal Leishmaniasis - Clinical and Epidemiological Aspects of 234 Cases Treated in a Tertiary Reference Center in the Brazilian Amazon
Jorge Augusto de Oliveira Guerra1,2*, Maria das Graças Vale Barbosa1,3, Marcilene Gomes Paes1, Renato Teles de Sousa3, Pricila Gama da Silva3, Maria José Silva3, Alexandre Ribera Macião3, Rafael Siqueira de Carvalho3, Leila Inês de Aguiar Raposo da Câmara Coelho1,3 and Luiz Carlos de Lima Ferreira1,2,31Tropical Medicine Foundation of Amazonas, Manaus, Amazonas, Brazil
2University of the State of Amazonas, Manaus, Amazonas, Brazil
3Federal University of Amazonas, Manaus, Amazonas, Brazil
- *Corresponding Author:
- Dr. Jorge Augusto de Oliveira Guerra
Tropical Medicine Foundation of Amazonas
Manaus, Amazonas, Brazil
E-mail: jguerra291@gmail. com
Received date: November 09, 2011; Accepted date: December 08, 2011; Published date: December 10, 2011
Citation: de Oliveira Guerra JA, das Graças Vale Barbosa M, Paes MG, de Sousa RT, da Silva PG, et al. (2011) Mucosal Leishmaniasis – Clinical and Epidemiological Aspects of 234 Cases Treated in a Tertiary Reference Center in the Brazilian Amazon. J Community Med Health Edu 1:110. doi:10.4172/2161-0711.1000110
Copyright: © 2011 de Oliveira Guerra JA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Presented here is a retrospective study including patients of the Brazilian Amazon region who were diagnosed with mucosal leishmaniasis (ML) and treated in a tertiary referral center between July 1992 to December 2008. In total, 234 patients fulfilled the inclusion criteria. There was a clear predominance of males, comprising 193 (82.5%) cases, and the mean age was 48 years. No fewer than 186 (79.5%) patients had undertaken activities that are considered to place one at risk of acquiring American Tegumentary Leishmaniasis (ATL) – agriculture, animal raising, or mineral extraction. Furthermore, 193 (82.5%) presented with a prior history of cutaneous leishmaniasis (CL); the average time between the onset of CL and the first symptoms of ML in 138 cases was 16.3 years. Finally, 156 cases (66.7%) were located in municipalities that lie on the south bank of the Amazon River, suggesting that Leishmania (Viannia) braziliensis was the likely etiological agent in these cases.
Keywords
Leishmaniasis; Mucocutaneous; Leishmania braziliensis; Amazon region
Introduction
Across the American continent (Western Hemisphere), eleven different Leishmania species are responsible for the forms of American Tegumentary Leishmaniasis (ATL) that are clinically recognizable, and present distinct epidemiological and demographic patterns [1].
In Brazil, 37.9% of ATL cases originate in the Northern region [2]. Marsden et al. [3] reported that the prevalence of mucosal leishmaniasis (ML) in Brazil lies between 3 and 5%. In the state of Amazonas, ML prevalence is around 1.5%, less than in the rest of the country [4].
The dispersion of ATL throughout Brazil from the Amazonian region is believed to have taken place during the “rubber boom” between 1880 and 1912. The war effort of the 1940s reactivated rubber production in the Amazon and new waves of northeasterners arrived into the region [5]. The increase in incidence of leishmaniasis occurred for various reasons: the human population’s geographic expansion, the construction of roads and the creation of new agricultural centers. This brought into play other important factors such as the movement of people to endemic regions as part of colonization projects, the movement of laborers, miners and their companies, and military exercises in jungle areas [6-9].
Within the Amazon region ATL is primarily a zoonosis, with a transmission cycle that occurs within sand flies and wild animals. In the majority of cases, humans are infected due to environmental alterations, when they may place themselves within the transmission cycle through penetration of the ecosystem [2,10,11].
The accurate diagnosis of ML is challenging within the Amazon region. The majority of cases present with only clinical and/or epidemiological criteria. This is occasionally supported by additional laboratory criteria such as a Montenegro skin test (MST – delayed hyper-sensitivity to leishmanial antigens), histopathological characteristics, or detection of parasites via direct exam.
The factors relating specifically to the occurrence of ML in the Brazilian Amazon are yet to be clarified, although it has been asserted that there is a relationship between the cutaneous lesion and mucosal disease, principally in individuals who engage in agricultural activities in areas of pristine rainforest, particularly the collection of latex and Brazil nuts [4,11].
Acquisition of data on the clinical, epidemiological, and laboratory factors related to mucosal disease in the region is important in order to improve disease control and diagnosis of ATL in the Manaus metropolitan area [4]. The majority of cases of ML treated in Manaus originated in distant regions, and the etiological agents of these cases have only recently been described for the Amazon Region [12]. The Amazon Tropical Medicine Foundation (FMT-HVD), which treats approximately 50% of ATL cases in the state, registers around 1,000 new cases each year [2,9], of which 15 to 20 are ML.
The purpose of this paper is to discuss the appearance of ML in relation to previous cutaneous lesions and how they were managed, considering aspects of the disease such as geographic origin, source of patient livelihood, socio-cultural practices and traditions and environmental factors, in patients diagnosed with ATL/ML and treated at the FMT-HVD.
Materials and Methods
A retrospective study was conducted including patients of the Amazon region who were diagnosed with ML at FMT-HVD between July 1992 and December 2008. The inclusion criteria were: patients submitted/referred for treatment of ML as recommended under official guidelines of the Brazilian Government [13] with a clinical history and physical examination suggestive of mucosal disease and/or a prior history of CL, and/or originating in the Brazilian Amazon region. The cases were confirmed by a positive complementary exam [14].
Patients were classified according to a set of employment activities defined by Cassano et al. [15] in agriculture, animal raising and mineral extraction. In the category of risk exposure, the activities considered to be at-risk were: those working directly in the rainforest environment, those involved in vegetal extraction (principally rubber tappers or “seringueiros”, and others whose primary occupation was the harvest of natural products, such as Brazil-nut collectors and woodcutters), farmers, and inhabitants of endemic areas (both indigenous and nonindigenous populations) during the period of cutaneous lesions.
A case of CL was defined as an ulcerated lesion on the skin associated with the presence of amastigote forms on microscopy, or which took more than three months to heal, and/or the presence of an atrophic scar suggestive of ATL [13].
All the information contained in documents relating to the cases of ML treated in the aforementioned period was evaluated. To determine the statistical significance of the data, we used the Minitab® 15.1.30.0. Program and for all the analyses a significant p value was set at ≤0.05. This study was developed according to international ethical standards for biomedical research involving human subjects and was approved by the Medical Ethics Commission of the FMT-HVD, protocol number - 1809/2006-FMTAM.
Results
Two hundred and thirty-four patients who fulfilled the requirements for inclusion in the study were selected. The results of this study represent nearly 74% of the total cases seen in FMT-HVD. Among them, there was a clear predominance of males, comprising 193 (82.5%) cases (p-value = 0.000). The mean age was 48 years (ranging from 8 to 87 years), with the greatest frequency (106 cases, or 45.3%) between 41 and 60 years of age (Table 1).
| Characteristic or finding | Value |
|---|---|
| Gender | |
| male | 193 (82.5%) |
| female | 41 (17,5%) |
| Age-group/ years (median = 48 ) | |
| 1 to 20 | 10 (4.3%) |
| 21 to 40 | 68 (29%) |
| 41 to 60 | 106 (45.3%) |
| > 60 | 50 (21.4%) |
| High risk activities for acquiring ATL | |
| Extraction of natural resources | 187 (80%) |
| House / stay in areas of transmission | 41 (17.5%) |
| Professional Activities in the area of â??â??transmission | 6 (2.5%) |
| Previous history of CL | 193 (82.5%) |
| Presence of cutaneous scar | 193 (82.5%) |
| Inadequate treatment of CL | 112 (63.6%) |
| Average time between CL and ML | 16.7 (30 days to 74 years) |
| Duration of disease, years (median) | 7.9 (30 days to 50 years) |
Table 1: Clinical and epidemiological characteristics of 234 patients with mucosal
leishmaniasis treated in a Tertiary Referral Center in the Amazon
With regards to lifestyle, 187 (80%) patients engaged in the extraction of natural resources: 74 (39.8%) patients were agricultural workers, 112 (60.2%) worked in extraction of natural resources (97 rubber tappers, six fishermen, four woodcutters and five mineralworker ´s) and 48 (21.5%) patients either lived or performed other activities in the transmission areas.
Of the total, 193 (82.5%) had a prior history of CL (of which eight had the concomitant form – mucocutaneous leishmaniasis or MCL), and 41 (17.5%) had no prior history of CL. The average time between the onset of CL and the first symptoms of ML in 163 cases was 16.7 years, ranging from 30 days to 74 years (Table 1). The average duration of the mucosal disease in 227 patients was 7.9 years.
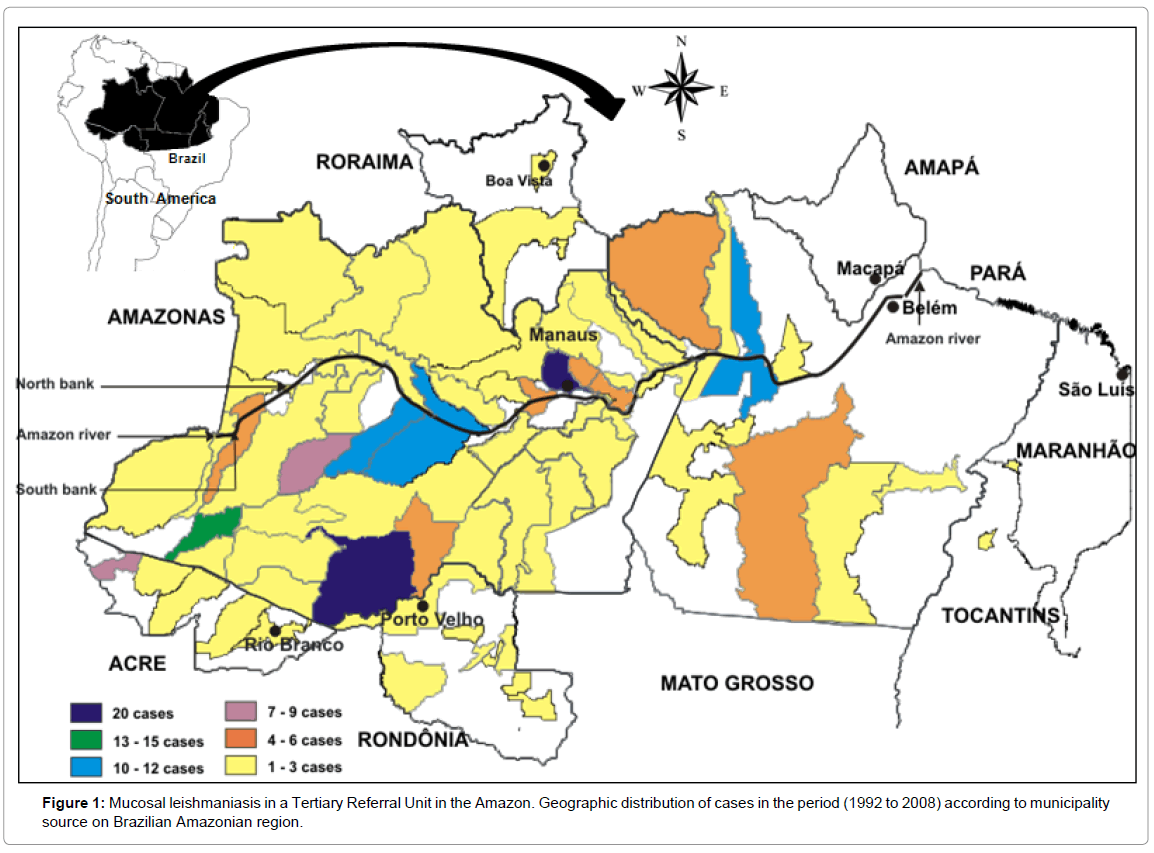
With regards to geographic location, 156 (66.7%) cases originated in the state of Amazonas, 45 (19.2%) in Pará, 15 (6.4%) in Acre, 11 (4.7%) in Rondônia, and the remainder from other Brazilian states of the Amazon region. One hundred and fifty-six cases (66.7%) were located in municipalities that lie on the right side or south bank of the Amazon River (Figure 1). When considering occupation and location along the Amazon River, there was statistical significance (P = 0.008) between the activity performed and the provenance of the right side or south bank of the Amazon River (Figure 1).
Discussion
Mucosal leishmaniasis represents a considerable public health problem in Latin America. Recent data have shown an increase in its incidence in several Brazilian states along with new areas [16] being affected each year. The debate surrounding the occurrence of ML and its diverse facets has been discussed by various authors [16-18]. The way of life of the population in the Amazon region, in direct contact with an otherwise pristine environment, particularly increases its exposure to the different vectors of ATL. This results in infections, symptomatic or asymptomatic, which lead to ML. Various activities have been associated with the risk of contracting ATL [19-21]. This study confirms that activities related to vegetal extraction, mainly those related to rubber tapping, appear to represent an increasing risk factor. This finding agrees with Marzochi and Marzochi [22] who refer to the predominant areas of L. (V.) braziliensis, namely the large rubber tapping region of the Amazon, which are confined almost exclusively to the tributaries on the right side or southern bank of the Amazon River; in this study 66.7% of cases analyzed originated from this region.
Unlike the outbreaks of CL linked to the unplanned settlements close to areas considered to be pristine rainforest [2], ML in the Amazon region appears to be more closely related to occupational activities of the patients in forest regions, principally those linked to vegetal extraction, in agreement with previous studies [3,4,23].
Most of the activities carried out by our patients put them into a situation considered to be at-risk for primary infection (CL) or development of mucosal disease (ML) years later. In the rest of Brazil, ML is predominantly caused by L. (V.) braziliensis [14,16,17,24] whereas in the Amazon region both L. (V.) braziliensis and L. (V.) guyanensis are found to cause cutaneous and mucosal disease [12]. Human infections are observed in people who undertake activities related to forest extraction, such as deforestation, road construction, oil drilling, and scientific expeditions [10].
In most endemic areas, 1–10% of CL infections results in mucosal leishmaniasis approximately 1-5 years after the cutaneous lesions have healed [3]. In this study, the median gap between the occurrence of CL and ML was 16.7 years.
In the cases described here, the predominance of subjects over 40 years of age, as indicated by the average age of 47.7 years, has also been observed in other studies involving ML [19]. In the cutaneous forms of the disease the predominant age group is between 20 and 40 years [18].
Various studies have demonstrated the predominance of males acquiring ATL, including ML [10,11,18]. Environmental factors predispose men to the vectors within forested areas or in other areas of transmission and in this study 82.5% of patients were male.
In a study carried out in Peru, Lucas et al. [25] observed that, of 351 people isolated with Leishmania, 279 had L. (V.) braziliensis, with 69% of these patients being carriers of MCL. Therefore, the Peruvian reality shows that a greater number of cases come from areas with difficult access, mainly due to the forest or a lack of roads. This fact represents an obstacle to the diagnosis and adequate treatment of many people with leishmaniasis.
These findings are corroborated by several authors [3,19,20], who suggest that a contributing factor to the development of the mucosal disease could be inadequate or irregular treatment of the primary cutaneous lesions. These findings are similar to those in this study which show that, of the 192 patients who had CL, 112 (63.5%) had a history of inadequate treatment of their cutaneous lesions. Furthermore, it demonstrates that multiple or extensive cutaneous lesions of long duration are more frequently associated with mucosal complications, determining ML [19], principally as a result of inadequate treatment or irregular dosages of the medication for primary cutaneous lesions [3,17]. Although the evolution is usually slow. In the Brazilian Amazon the mucosal disease tends to occur in similar circumstances [10,20,24].
The complexity and severity of the mucosal disease, its chronic character, its tendency to relapse, the difficulty in obtaining a correct diagnosis, and the limited access to treatment are some of the characteristics that hinder the understanding of the clinical and epidemiological aspects of these cases, reflecting the challenges facing these populations and their healthcare services. Therein lies the importance of this study.
We can state, based on this research, that mucocutaneous leishmaniasis is also a great challenge for the public health of the populations that inhabit the Amazon and which manifests itself in the very livelihood of these populations, who maintain a high degree of intimacy with the rainforest, from which they derive their sustenance [23]. This gives rise to, in the majority of cases, the formation of a cutaneous lesion which is not adequately treated because of the lack of knowledge of its complications, which itself is the result of a lack of access to a valid diagnosis and appropriate treatment, eventually manifesting itself, often years later, as the mucosal disease.
In sum, we emphasize that the findings of this study ought to be complemented by others involving populations with similar characteristics, due to the magnitude of this problem in the Amazonian population.
References
- Desjeux P (2004) Leishmaniasis: current situation and new perspectives. Comp Immunol Microbiol Infect Dis 27: 305-318.
- Guerra JA, Ribeiro JA, Coelho LI, Barbosa MG, et al. (2006) Epidemiology of tegumentary leishmaniasis in São João, Manaus, Amazonas, Brazil.Cad Saude Publica 22: 2319-2327.
- Marsden PD (1986) Mucosal leishmaniasis (“espundia” Escomel, 1911). Trans R Soc Trop Med Hyg 80: 859-876.
- Paes MG, Barros MLB, Toledo LM (1998) Considerações sobre a produção da leishmaniose tegumentar americana no Estado do Amazonas. Espaço & Doença: um olhar sobre o Amazonas: 105-113.
- Altamirano-Enciso AJ, Marzochi MC, Moreira JS, Schubach AO, Marzochi KB (2003) On the origin and spread of cutaneous and mucosal leishmaniasis, based on pre-and post colombian historical source. Hist Cienc Saude Manguinhos 10: 852-882.
- Barros MLB, Paes MG, Talhari S (1982) Leishmaniose cutaneo-mucosa na Amazônia – Estudo dos casos diagnosticados em Manaus no período de 1976 a 1980. An Bras Dermatol 57: 153-154.
- Talhari S, Arias JÁ, Cunha MGS, Naiff RD, Freitas RA et al. (1988) Leishmaniose no Estado do Amazonas - Aspectos Epidemiológicos Clínicos e Terapêuticos. An Bras Dermatol 63: 433-438.
- Handman E (2001) Leishmaniasis: current status of vaccine development. Clin Microbiol Rev 14: 229-243.
- Oliveira Guerra JA, Talhari S, Paes MG, Garrido M, Talhari JM (2003) Clinical and diagnostic aspects of American tegumentary leishmaniosis in soldiers simultaneously exposed to the infection in the Amazon Region. Rev Soc Bras Med Trop 36: 587-590.
- Lainson R (1983) The American leishmaniases: some observations on their ecology and epidemiology. Trans R Soc Trop Med Hyg 77: 569-596.
- Lainson R (1985) Our present knowledge of the ecology and control of leishmaniasis in the Amazon Region of Brazil. Rev Soc Bras Med Trop 18: 47- 56.
- Guerra JA, Prestes SR, Silveira H, Coelho LI, Gama P, et al. (2011) Mucosal Leishmaniasis caused by Leishmania (Viannia) braziliensis and Leishmania (Viannia) guyanensis in the Brazilian Amazon. PLoS Negl Trop Dis 5: e980.
- MS/Brasil (2008) Manual de controle da leishmaniose tegumentar americana. In: Saúde FNd, editor. Brasilia: FNS 62.
- Castellucci L, Cheng LH, Araújo C, Guimarães LH, Lessa H, et al. (2005) Familial aggregation of mucosal leishmaniasis in northeast Brazil. Am J Trop Med Hyg 73: 69-73.
- Cassano C, de Medeiros Frias LA, Valente JG (2000) Classification by occupation of AIDS cases in Brazil- 1995. Cad Saude Publica 16: 53-64.
- Amato VS, Tuon FF, Bacha HA, Neto VA, Nicodemo AC (2008) Mucosal leishmaniasis . Current scenario and prospects for treatment. Acta Trop Jan 105: 1-9.
- Amato VS, Tuon FF, Siqueira AM, Nicodemo AC, Neto VA (2007) Treatment of mucosal leishmaniasis in Latin America: systematic review. Am J Trop Med Hyg. Aug 77: 266-274.
- Marsden PD, Llanos-Cuentas A, Lago EL, Cuba-Cuba AC, Barreto AC, et al. (1984) Human mucocutaneous leishmaniasis in Três Braços, Bahia, Brazil. An area of Leishmania braziliensis braziliensis transmission. III. Mucosal disease: presentation and initial evolution. Rev Soc Bras Med Trop 17: 179-186.
- Machado-Coelho GL, Caiaffa WT, Genaro O, Magalhães PA, Mayrink W (2005) Risk factors for mucosal manifestation of American cutaneous leishmaniasis. Trans R Soc Trop Med Hyg 99: 55-61.
- Silveira FT, Lainson R, Corbett CE (2004) Clinical and immunopathological spectrum of American cutaneous leishmaniasis with special reference to the disease in Amazonian Brazil: a review. Mem Inst Oswaldo Cruz 99: 239-251.
- Guerra JA, Barbosa MG, Loureiro AC, Coelho CP, Rosa GG et al. (2007) Cad Saude Publica 23: 2215- 2223.
- Marzochi MC, Marzochi KB (1994) Tegumentary and visceral leishmaniases in Brazil: emerging anthropozoonosis and possibilities for their control. Cad Saude Pub American tegumentary leishmaniasis in children: epidemiological aspects of cases treated in Manaus, Amazonas, Brazil.lica 10: 359-375.
- Futemma C (2006) Uso e acesso aos recursos florestais: os caboclos do baixo Amazonas e seus atributos sócio-culturais. In: Adams C MR, Neves W, editor. Sociedades Caboclas Amazônicas - Modernidade e Invisibilidade: FAPESP. http://www.scielo.br/pdf/asoc/v11n2/v11n2a16.pdf
- Reithinger R, Dujardin JC, Louzir H, Pirmez C, Alexander B, et al. (2007) Cutaneous leishmaniasis. Lancet Infect Dis 7: 581-596.
- Lucas CM, Franke ED, Cachay MI, Tejada A, Cruz ME, et al. (1998) Geographic distribution and clinical description of leishmaniasis cases in Peru. Am J Trop Med Hyg Aug 59:312-317.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 14187
- [From(publication date):
December-2011 - Apr 01, 2025] - Breakdown by view type
- HTML page views : 9618
- PDF downloads : 4569