Research Article Open Access
Management of Patients with Ulcerative Colitis after Proctocolectomy:Pouchitis is a Real Danger
Tamás Molnár*, Klaudia Farkas, Ferenc Nagy, Zoltán Szepes and Tibor Wittmann
First Department of Medicine, University of Szeged, Szeged, Hungary
- *Corresponding Author:
- Tamás Molnár
First Department of Medicine
University of Szeged, H-6720
Korányi fasor 8, Szeged, Hungary
Tel: +36-62-545186
Fax: +36-62-545185
E-mail: mot@in1st.szote.u-szeged.hu
Received date: September 12, 2011; Accepted date: November 14, 2011; Published date: November 16, 2011
Citation: Molnár T, Farkas K, Nagy F, Szepes Z, Wittmann T (2011) Management of Patients with Ulcerative Colitis after Proctocolectomy: Pouchitis is a Real Danger. J Gastrointest Dig Syst 1:102. doi:10.4172/2161-069X.1000102
Copyright: © 2011 Molnár T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Pouchitis develops in about 50% of the patients with ulcerative colitis (UC) undergoing colectomy.
Aim: The aim of this study was to evaluate the frequency of pouchitis, to determine risk factors and to assess the efficacy of infliximab in refractory pouchitis.
Patients and Methods: 76% of the 46 UC patients requiring colectomy underwent ileal pouch-anal anastomosis (IPAA) procedure. Demographic, clinical and therapeutic parameters were compared between patients who did and did not develop pouchitis and between those with pouchitis responding or being refractory to the conservative therapy.
Results: 40% of the patients developed pouchitis. Six patients received infliximab therapy. Extraintestinal manifestation and non smoking was characteristic for refractory pouchitis.
Discussion: Pouchitis developed in 40% of our patients undergoing IPAA. The development of pouchitis seems to be predisposed by frequent preoperative hospitalization. The earlier onset of pouchitis seems to be a prognostic factor for the unsuccessful conservative treatment and the need for biological therapy.
Keywords
Ulcerative colitis; Ileal pouch-anal anastomosis; Pouchitis; Infliximab
Introduction
Approximately 30% of patients with relapsing, extensive ulcerative colitis (UC) require surgery [1]. Total proctocolectomy with ileal pouchanal anastomosis (IPAA) represents the most common and potentially curative surgical procedure for intractable UC since 1978, although up to 50% of the patients undergoing surgery will develop pouchitis [2]. Ethiopathogenesis of pouchitis is still unclear. It is thought to be a third and distinctly different form of inflammatory bowel diseases (IBD). Since patients with UC are more likely to get pouchitis than those with familial adenomatous polyposis, genetic predisposition and the autoimmune phenomena are susceptible in the development of the disease [3]. Various infections (cytomegalovirus, Candida, Clostridium difficile), ischemia, autoimmune disorders, collagen deposition and the regular use of nonsteroidal anti-inflammatory drugs are known causative agents in the development of pouchitis [4], whereas the idiopathic form of the disease is thought be the result of an abnormal mucosal immune response to altered microflora of the pouch [5].
Pouchitis usually responds to conventional antibiotic therapy. Refractory pouchitis develops in 5-19% of the cases and may lead to pouch failure and excision. A recently published paper by Ferrante et al. [6] on the efficacy of infliximab in refractory pouchitis showed clinical response at week 10 in 82% of the patients with refractory luminal inflammation and sustained clinical response were achieved in 56% of the patients after a median follow-up of 20 months.
The aim of this study was to evaluate the frequency of pouchitis in our UC patients who had undergone colectomy and to determine risk factors that predict refractory pouchitis. In this study we also assessed retrospectively the efficacy of infliximab in refractory pouchitis.
Patients and methods
The outcome of 46 UC patients (29 females, 17 males; average age at the diagnosis: 30 years [12-60]) undergoing colectomy due to severe disease refractory to rescue therapy in 63%, chronic activity in 35% and intramucosal carcinoma in 1 patient was assessed retrospectively. The mean disease duration was 10 years at the time of surgery. The average follow-up period from colectomy was 3.3 (0-10) years. 35 (76%) patients underwent IPAA procedure, 10 patients needed definitive ileostomy and in one case ileorectal anastomosis was requested by the patient. Clinical and demographic characteristics of patients undergoing IPAA are detailed in (Table 1).
| Patients undergoing IPAA (n=35) | |
|---|---|
| Female/male Median age at the diagnosis (years) Median duration between diagnosis and surgery (years) Indication for surgery
Average number of surgical interventions Presence of pouchitis |
22/13 (63/37%) 29.7 (12-60) 8.2 (0.1-24) 34 (97%) 1 (3%) 27 (77%) 8 (23%) 6 (17%) 29 (83%) 9 (26%) 2.6 (2-6) 14 (40%) |
Table 1: Characteristics of patients undergoing IPAA procedure.
Data of patients developing pouchitis were analyzed in detail. Pouchitis was defined as Pouchitis Disease Activity Index (PDAI) > 7 points [7]. The patients with and without pouchitis were asked to complete questionnaires regarding to the quality of life before and after colectomy. The alteration of body weight, the disease duration at the surgery, the number of in and outpatient visits, surgical interventions because of postoperative complications, and the number of medication used before and after IPAA operation was compared between patients who did and did not develop pouchitis using two-sample t-test and one-way analysis of variance. P<0.05 was considered statistically significant. Ethical approvals for the study have been obtained from the Ethical Committee of the University of Szeged.
Demographic, clinical and therapeutic parameters were also compared between patients with pouchitis responding or being refractory to the conservative therapy. Infliximab at a dose of 5 mg/ kg was administered at week 0, 2, 6 and in every 8 weeks in case of refractory pouchitis. Clinical response to infliximab was evaluated by the frequency of diarrhoea, blood loss, and abdominal pain, and by the assessment of endoscopic and histological findings of the pouch.
Results
40% of the patients (9 females, 5 males; average age at the diagnosis: 28.6 years [14-48]) who had undergone IPAA developed pouchitis. No difference was detected in the alteration of the body weight, the disease duration and the number of the surgical interventions between IPAA patients with and without pouchitis. The need for hospitalizations before colectomy was significantly more common in patients with vs. without pouchitis (p=0.02). The number of outpatient admissions both before (p=0.02) and after (p=0.05) IPAA procedure, and the number of medications after surgery (p<0.001) was significantly higher in patients suffering from pouchitis. Patients with pouchitis assessed their quality of life significantly worse than those who did not develop inflammation (p=0.005).
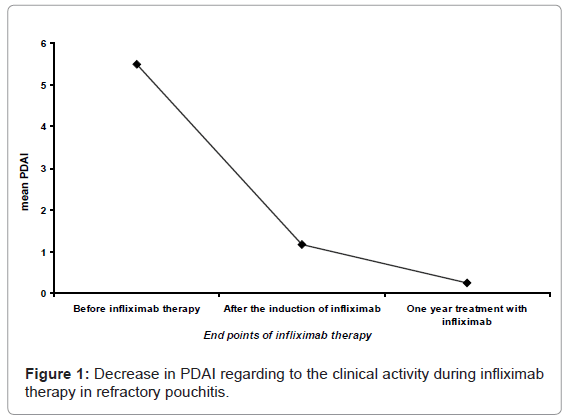
Six patients with refractory pouchitis (3 males, and 3 females; average age at the diagnosis: 25.2 years, average disease duration: 7.8 years, mean PDAI: 17 [18-14]) failed to respond to conservative treatment and received infliximab therapy. The average number of infliximab infusions was 12.5/patient (8-20 infusions). Infliximab was effective in all case, complete remission was achieved after a median follow up of 19.8 months. Figure 1 shows the alteration of PDAI regarding to only the clinical parametersin patients treated with infliximab. None of the patients needed permanent ileostomy.
The average time between the occurrences of pouchitis in the refractory and non refractory groups were 3.28 (0.8-6.8) and 1.69 (0.02-3.9) years, respectively. Extraintestinal manifestation was present in 5 of the 6 patients (83.3%) with refractory pouchitis, whereas smoking was characteristic for 3 of the 8 patients responding to the conventional therapy of pouchitis. None of the patients with refractory disease smoked. Table 2 summarizes the predictors of the development of refractory pouchitis.
| Non refractory pouchitis | Refractory pouchitis | |
|---|---|---|
| Frequency after IPAA | 23% | 17% |
| Smoking | 37.5% | 0% (p=0.04) |
| Extraintestinal manifestation | 12.5% | 83.3% (p=0.007) |
| Time elapsed between IPAA and the occurrence of pouchitis (years) | 3.28 (0.8-6.8) | 1.69 (0.02-3.9) (p=0.1) |
Table 2: Predictors of the development of refractory pouchitis.
Discussion
Pouchitis is an idiopathic chronic inflammatory disease that may occur in the ileal pouch after restorative proctocolectomy with IPAA and seems to be the most frequent in the first 2-3 years after closure of the ileostomy. Finding routinely available risk factors predicting to the development of pouchitis is becoming more and more important for the selection of the appropriate treatment. Genetic polymorphisms, extraintestinal manifestations, the presence of serum perinuclear antineutrophil cytoplasmic antibodies, backwash ileitis, thrombocytosis, non-smoking behaviour, extensive UC and the use of NSAIDs are some of the previously identified risk factors for pouchitis [8]. A retrospective review by Hoda et al. [9] found that patients who did not undergo diverting ileostomy at the time of the IPAA and those with postoperative complications were more likely to develop chronic pouchitis, whereas primary sclerosing cholangitis and extraintestinal manifestations – known predictors for acute pouchitis – did not trend toward a higher likelihood of developing chronic pouchitis.
Pouchitis is usually well-controlled with antibiotic therapy. Results of eleven randomized controlled trials on the management of pouchitis were reviewed in the recently published Cochrane Database [10]. Ciprofloxacin proved to be more effective at inducing remission than metronidazole, whereas budesonid enemas showed similar efficiency with metronidazole. For the maintenance of remission and the prevention of chronic pouchitis, VSL#3 probiotic proved to be more effective than placebo. Chronic pouchitis which requires maintenance suppressive therapy and common leads to pouch failure has been reported in approximately 9% to 20% of all surgeries [11]. Refractory pouchitis may significantly influence the patients’ quality of life. Experience with the treatment of chronic relapsing or refractory pouchitis is limited. Infliximab has been successfully used in the induction and maintenance of remission both in Crohn’s disease (CD) and in UC [12-14]. The fact that tumor necrosis factor (TNF)-α expression was significantly higher in the mucosal biopsies of the inflamed pouch compared to the normal, noninflamed one suggest that infliximab may also be efficacious in treating refractory pouchitis. Children with refractory pouchitis were treated with infliximab in combination with an immunomodulator drug after failure to respond to antibiotics, aminosalicylates and immunomodulators resulting in significant improvement clinically, endoscopically, and histologically [15]. The results of a study by Viscido et al. [16] indicated that infliximab in combination with azathioprine may also be recommended for the treatment of refractory pouchitis complicated by fistulae.
Pouchitis developed in 40% of our patients undergone IPAA during the follow up period. 17% of the patients with pouchitis required biological therapy. The development of pouchitis seems to be predisposed by frequent hospital admissions before colectomy. Severe, refractory pouchitis was significantly more common in non-smokers and in patients with extraintestinal manifestations. Although significant differences could not be detected, the earlier onset of pouchitis seems to be a prognostic factor for the unsuccessful conservative treatment and the need for biological therapy. Our data suggest that infliximab may be at least as effective in refractory pouchitis as in severe UC, although further randomized controlled studies are needed to confirm these results.
References
- Truelove SC, Jewell DP (1974) Intensive intravenous regimen for severe attacks of ulcerative colitis. Lancet 1: 1067-1070.
- Fazio VW, Ziv Y, Church JM Oakley JR, Lavery IC, et al. (1995) Ileal pouchanal anastomosis: complications and function in 1005 patients. Ann Surg 222: 120-127.
- Cheifetz A, Itzkowitz S (2004) The diagnosis and treatment of pouchitis in inflammatory bowel disease. J Clin Gastroenterol 38: S44-S50.
- Navaneethan U, Shen B (2010) Secondary pouchitis: Those with identifiable ethiopathogenetic or triggering factors. Am J Gastroenterol 105: 51-64.
- Coffey JC, Rowan F, Burke J, Dochery NG, Kirwan WO, et al. (2009) Pathogenesis of and unifying hypothesis for idiopathic pouchitis. Am J Gastroenterol 104: 1013-1023.
- Ferrante M, D'Haens G, Dewit O, Baert F, Holvoet J, et al. (2010) Efficacy of infliximab in refractory pouchitis and Crohn's disease-related complications of the pouch: a Belgian case series. Inflamm Bowel Dis 16: 243-249.
- Sandborn WJ, Tremaine WJ, Batts KP, Pemberton JH, Phillips SF (1994) Pouchitis after ileal pouch-anal anastomosis: a Pouchitis Disease Activity Index. Mayo Clin Proc 69: 409-415.
- Yamamoto-Furusho JK (2007) Pouchitis. World J Gastroenterol 13: 5598- 5604.
- Hoda KM, Collins JF, Knigge KL, Deveney KE (2008) Predictors of pouchitis after ileal pouch-anal anastomosis: a retrospective review. Dis Colon Rectum 51: 554-560.
- Holubar SD, Cima RR, Sandborn WJ, Pardi DS (2010) Treatment and prevention of pouchitis after ileal pouch-anal anastomosis for chronic ulcerative colitis. Cochrane Database Syst Rev 16: CD001176.
- Stahlberg D, Gullberg K, Liljeqvist L, Hellers G, Löfberg R (1996) Pouchitis following pelvic pouch operation for ulcerative colitis. Incidence, cumulative risk, and risk factors. Dis Colon Rectum 39: 1012-1018.
- Hanauer SB, Feagan BG, Lichtenstein GR, Mayer LF, Schreiber S, et al. (2002) Maintenance infliximab for Crohn's disease: the ACCENT I randomized trial. Lancet 359: 1541-1549.
- Present DH, Rutgeerts P, Targan S, Hanauer SB, Mayer L, et al. (1999) Infliximab for the treatment of fistulas in patients with Crohn's disease. N Engl J Med 340: 1398-1405.
- Rutgeerts P, Sandborn WJ, Feagan BG, Reinisch W, Olson A, et al. (2005) Infliximab for induction and maintenance therapy for ulcerative colitis. N Engl J Med 353: 2462-2476.
- Kooros K, Katz AJ (2004) Infliximab therapy in pediatric Crohn's pouchitis. Inflamm Bowel Dis 10: 417-420.
- Viscido A, Kohn A, Papi C, Caprilli R (2004) Management of refractory fistulizing pouchitis with infliximab. Eur Rev Med Pharmacol Sci 8: 239-246.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 15171
- [From(publication date):
December-2011 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 10493
- PDF downloads : 4678