Research Article Open Access
Long QT Syndrome (LQTS) in Opiate, Cocaine and Alcohol Addiction, with HIV+ / HCV+ Co-Infection in Antiretroviral Therapy (HAART)
D. Demarie2*, G. Marletta1, E. De Vivo1, E. Rivela1 and E. Bignamini11Addiction Department 1, ASL TO2 Torino, Italy
2Cardiology Department, ASL TO2 Torino, Italy
- *Corresponding Author:
- Daniela Demarie, M.D.,
Maria Vittoria Hospital, Via Cibrario 72, Torino, Italy
Tel: 3347659587, 0114393486
Fax: 0114393387
E-mail: d.demarie@aslto2.it
Received June 20, 2011; Accepted July 22, 2011; Published July 26, 2011
Citation: Demarie D, Marletta G, De Vivo E, Rivela E, Bignamini E (2011) Long QT Syndrome (LQTS) in Opiate, Cocaine and Alcohol Addiction, with HIV+ / HCV+ Co-Infection in Antiretroviral Therapy (HAART). J Addict Res Ther 2:114. doi:
Copyright: © 2011 Demarie D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Addiction Research & Therapy
Case Report
We describe a case of 28 years old woman, HIV and HCV coinfected, addicted to cocaine and heroin, and alcohol. The patient was in methadone maintenance therapy with 60 mg / die.
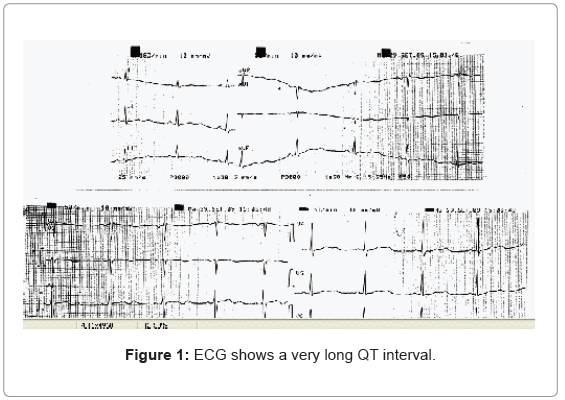
She was referred to cardiology department on September 2009 because of syncope associated with noise tachycardia. Orthostatic hypotension was present associated with presyncope symptoms The ECG showed a very long QT about 0,580” (Figure 1) and ventricular extra systolic beats in couple and triplets. There were not abnormalities of P duration, PR interval and QRS duration both at hospital admission and at 18-months of follow up.
The CD4 level, at hospital admission was 243/μL, the viral load was high and a sub clinical human papillomavirus infection (HPV) was present.
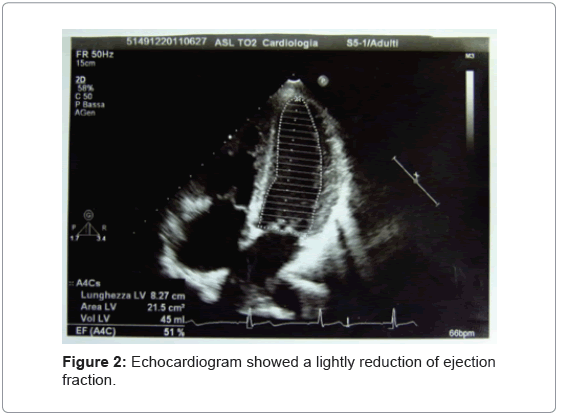
Echocardiogram performed when the patient was admitted to the hospital, (Figure 2) showed a transient reduction of ventricular ejection fraction that completely normalized in following echocardiograms upon beginning ARVT. There were not valvular abnormalities.
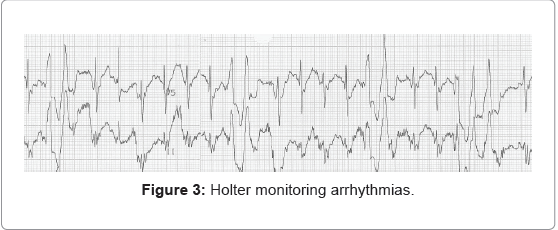
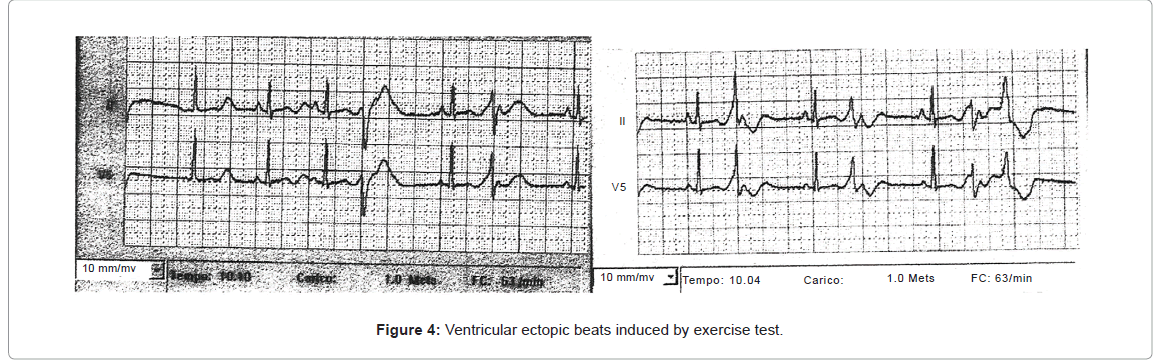
Holter monitoring presented a high number of ventricular arrhythmias, (i.e ventricular couples and triplets and some runs of non sustained ventricular tachycardia) (Figure 3). During the treadmill exercise test the patient was stopped at 4’ of exercise for ventricular bigeminy (Figure 4).
Because of poor compliance of the patient, genetic test to evaluate congenital long QT syndrome was not performed, even if at the Schwartz point system for the diagnosis of congenital LOTS our patient reached four points.
Beta blocker therapy was started with methoprolol 25 mg once a day. It was impossible to increase the dose because the patient had low blood pressure and low heart rate. Methadone treatment was reduced until 40 mg a day.
| Data Nascita: | 06/05/1983 | Eta: 28 Anni | Sesso G | |
|---|---|---|---|---|
| Richiesta: 58001052 | Del 27/06/2011 | Ore: 12:16 | ||
| Esame | Esito | U.M. | Val. Tiferimento | Metodo |
| Analisi Genetica: Discrimnazione allelica. | ||||
| Materiale: Sangue | ||||
| Genotipo CYP 2B6 516 rs3745274 G->T | TT | PCR real-time | ||
| Genotipo GG: enzima ad alata attivita metabolica; Genotipo GT: enzima a media attivita metabolica; Genotipo TT: enzima a bassa attivita metabolic. |
||||
| Genotipo CYP 2B6 983 rs28399499 T->C | TT | PCR real-time | ||
| Genotipo CYP 3A4* IB (rs 2740574): AA. L’enzima con questo polimorfismo dovrebbe Presentare un’attivita metabolic nella norma. |
||||
| Genotipo TT: enzima ad alata attivita metabolica; Genotipo GT: enzima a media attivita metabolica; Genotipo TT: enzima a bassa attivita metabolic. |
||||
strong>Table 1:
In 18 months of follow up, the patient avoided cocaine, heroin and alcohol abuse, but the QT interval remained very long (>500 msec) , P wave, PR and QRS intervals did not change.
ARVT (efavirenz + tenofovir + emcitrabine) was started with normalization of QT interval.
Control exercise test was stopped At 9’ of exercise. The test showed; always a prolongation of QT interval but major ventricular arrhythmias disappeared.
Upon beginning of ARVT, CD4 increased until 409 μL and viral load decreased (< 20 c/mL).
Genetic test about main methadone metabolizing enzymes CYP2B6 and CYP3A4 was performed and showed a very low activity of CYP2B6 (Table 1).
Discussion
Long QT syndrome is more frequent in subjects infected with HIV than in the general population and has been reported to occur in up to 29% of the hospitalized HIV-positive patients. Why long QT syndrome occurs more often in HIV-positive patients is currently unknown. There are multiple possible explanations why long QT syndrome is more prevalent in HIV-infected patients [4]. HIV-positive patients frequently receive medications that prolong the QT interval such as diflucan, clarithromycin, and cotrimoxazole. Furthermore, antiretroviral drugs themselves have been implied to cause prolongation of the QT interval. Whether HIV infection itself might cause heart disease and QT-interval prolongation is controversial. Autonomic dysfunction due to HIV-associated neuropathy [5,6] is also a presumed cause of long QT syndrome in HIV patients and could have been a contributing factor in our patient, who suffered from HIV-associated peripheral neuropathy (i.e. orthostatic hypotension).
In our patient genetic test to value congenital long QT syndrome was not performed, even if at the Schwartz point system for the diagnosis of congenital LOTS. She reached four points [7] because of her poor compliance. She had many causes of acquired long QT syndrome.
As everybody knows a low CD4 cells count and a high VL (viral Load) may be risk factors potentially related to QT prolongation in HIV patients in the outpatient setting [8,9]. A recent and important work shows that low CD4 cell count and a high VL may be risk factors potentially related to QT prolongation in HIV patients in the outpatient setting.
Our case is very atypical because the normalization of QT interval happened when the ARVT was started. For this reason, we looked for a possible explanation in genetic mutation of main metabolizing methadone enzymes [10], and/or possible inter drug interference between efavirenz and methadone [11].
As our Knowledge there are many reports in which efavirenz [12] a non nucleoside reverse transcriptase inhibitor is responsible for acquired long QT syndrome and torsades de pointes. Genetic test to value the function of CYP2B6 and CYP3B4 was performed and showed a very low activity of CYP2B6 with normal function of CYP 3A4. The introduction of efavirenz that was in normal range decreases plasma methadone level. In fact efavirenz is a very effective non-nucleoside reverse transcriptase inhibitor (NNRTI). Efavirenz is metabolized in the liver, and is both a substrate and inducer of the 2B6 and 3A4 isoforms of the cytochrome P450 system. This means efavirenz may interact with other drugs metabolized in the liver like methadone, decreasing its blood concentration [13]. In fact the patient showed withdrawal symptoms when methadone dosage was reduced [14].
Beta blocker therapy effective on ventricular arrhythmias became effective on QT interval upon beginning ARVT.
We consider this case very interesting, because it links scientific and clinical aspects. The results of genetic test, in fact, confirm our study hypothesis. Moreover, it improves our clinical management, showing how is important to personalize therapy, especially in very complex drug interactions.
References
- Kocheril AG, Bokhari SA, Batsford WP, Sinusas AJ (1997) Long QT(c) and torsades de pointes in human immunodeficiency virus disease. Pacing Clin Electrophysiol 20: 2810-2816.
- Sani MU, Okeahialam BN (2005) QTc interval prolongation in patients with HIV and AIDS. J Natl Med Assoc 97: 1657-1661.
- Reinsch N, Buhr C, Krings P, Kaelsch H, Neuhaus K, et al. (2009) German Heart Failure Network. Prevalence and risk factors of prolonged QTc interval in HIVinfected patients: results of the HIV-HEART study. HIV Clin Trials 10: 261-83.
- Freeman R, Roberts MS, Friedman LS, Broadbridge C (1990) Autonomic function and human immunodeficiency virus infection. Neurology 40: 575-580.
- Villa A, Foresti V, Confalonieri F (1995) Autonomic neuropathy and prolongation of QT interval in human immunodeficiency virus infection. Clin Auton Res 5: 48-52.
- Castillo R, Pedalino RP, El-Sherif N, Turitto G (2002) Efavirenz-associated QT prolongation and Torsade de Pointes arrhythmia. Ann Pharmacother 36: 1006-1008.
- Shimabukuro-Vornhagen A, Rybniker J, Zoghi S, Faetkenheuer G, Michels G, et al. (2010) Acquired Long QT Syndrome and Torsade de Pointes Associated with HIV Infection. Case Report Med pii: 278427.
- Qaqa AY, Shaaban H, DeBari VA, Phung S, Slim J, et al. (2010) Viral load and CD4+ cell count as risk factors for prolonged QT interval in HIV-infected subjects: a cohort-nested case-control study in an outpatient population. Cardiology 117: 105-111.
- Lichtenstein KA, Armon C, Buchacz K, Chmiel JS, Buckner K, et al. (2010) Low CD4+ T cell count is a risk factor for cardiovascular disease events in the HIV outpatient study. Clin Infect Dis 51: 435-447.
- Shiran MR, Lennard MS, Iqbal MZ, Lagundoye O, Seivewright N, et al. (2009) Contribution of the activities of CYP3A, CYP2D6, CYP1A2 and other potential covariates to the disposition of methadone in patients undergoing methadone maintenance treatment. Br J Clin Pharmacol 67: 29-37.
- Calvo R, Lukas JC, Rodriguez M, Carlos MA, Suarez E (2002) Pharmacokinetics of methadone in HIV-positive patients receiving the nonnucleoside reverse transcriptase efavirenz. Br J Clin Pharmacol 53: 212-214.
- R Castillo, RP Pedalino, N El-Sherif, G Turitto (2002) Efavirenz-associated QT prolongation and Torsade de Pointes arrhythmia. Ann Pharmacother 36: 1006-1008.
- Calvo R, Lukas JC, Rodriguez M, Carlos MA, Suarez E (2002) Pharmacokinetics of methadone in HIV-positive patients receiving the nonnucleoside reverse transcriptase efavirenz. Br J Clin Pharmacol 53: 212-214.
- Tossonian HK, Raffa JD, Grebely J, Trotter B, Viljoen M, et al. (2007) Methadone dosing strategies in HIV-infected injection drug users enrolled in a directly observed therapy program. J Acquir Immune Defic Syndr 45: 324-327.
Relevant Topics
- Addiction Recovery
- Alcohol Addiction Treatment
- Alcohol Rehabilitation
- Amphetamine Addiction
- Amphetamine-Related Disorders
- Cocaine Addiction
- Cocaine-Related Disorders
- Computer Addiction Research
- Drug Addiction Treatment
- Drug Rehabilitation
- Facts About Alcoholism
- Food Addiction Research
- Heroin Addiction Treatment
- Holistic Addiction Treatment
- Hospital-Addiction Syndrome
- Morphine Addiction
- Munchausen Syndrome
- Neonatal Abstinence Syndrome
- Nutritional Suitability
- Opioid-Related Disorders
- Relapse prevention
- Substance-Related Disorders
Recommended Journals
Article Tools
Article Usage
- Total views: 16220
- [From(publication date):
July-2011 - Nov 29, 2025] - Breakdown by view type
- HTML page views : 11522
- PDF downloads : 4698