Case Report Open Access
Liver Amyloidosis Complicated with Liver Failure: A Case Report and Review of the Literature
Mona AL-Saedi1*, Faisal Batwa1, Ahmed Absi2 , Yaser Dahlan1, Mohamed Satti3, and Abdul Halim Kinsara1
1Department of Medicine, King Khalid National Guard Hospital, King Abdul-Aziz Medical City, Kingdom of Saudi Arabia/Jeddah
2Department of Haematology, King Khalid National Guard Hospital, King Abdul-Aziz Medical City, Kingdom of Saudi Arabia/Jeddah
3Department of Histopathology, King Khalid National Guard Hospital, King Abdul-Aziz Medical City, Kingdom of Saudi Arabia/Jeddah
- *Corresponding Author:
- Mona AL-Saedi
Department of Medicine
King Khalid National Guard Hospital
King Abdul-Aziz Medical City
Kingdom of Saudi Arabia/Jeddah
Tel: +966-050-6364003
Fax: +966-262-40000
E-mail: dr_mona.h@hotmail.com
Received date: October 19, 2012; Accepted date: November 02, 2012; Published date: November 05, 2012
Citation: AL-Saedi M, Batwa F, Absi A, Dahlan Y, Satti M, et al. (2012) Liver Amyloidosis Complicated with Liver Failure: A Case Report and Review of the Literature. J Gastroint Dig Syst S3:002. doi: 10.4172/2161-069X.S3-002
Copyright: © 2012 AL-Saedi M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Introduction: Liver involvement by amyloidosis is not uncommon. The clinical presentation is usually subclinical or with mild elevation of liver enzymes. Liver failure and rupture has rarely been reported. We report a case that presented with new onset ascites and rapidly progressed into liver failure and rupture with fatal outcome. Methods: A 53 years old male patient presented with progressive anasarca over 2 months. His evaluation revealed ascites with high serum-ascites albumin gradient. Liver imaging suggested mild hepatomegaly with nodular liver and splenomegaly with patent hepatic and portal veins. Cardiac workup was unremarkable. Non nephrotic range proteinuria was noted with hypoalbuminemia and mild hyperbilirubinemia. Esophageal varices were seen on gastroscopy. After thorough blood tests, the patient was labelled as cryptogenic cirrhosis and started on diuretics. Result: One week later he developed transient renal failure and confusional state. His serum bilirubin started to increase rapidly .Under evaluation for liver transplant, the patient underwent liver biopsy which showed massive deposits of amyloid with atrophy of hepatocytes. Rectal biopsy was unremarkable. Bone marrow biopsy showed hypercellular marrow with 5-10% abnormal looking plasma cells some appeared in abnormal clusters with thickened blood vessels which were positive for congo red stain. Kappa and lambda immunochemical stains were inconclusive and cytogenetic studies were not performed. Serum protein electrophoresis was normal. Urinary Bence-Jones proteins were negative. Skeletal survey could not be done due to the patient’s critical condition. Five days later the patient developed hypotension with leukocytosis and was transferred to the Intensive Care Unit with the impression of septic shock. Ascetic tap showed frank blood and computed tomography confirmed rupture of the liver. His liver enzymes and bilirubin continued to deteriorate and he developed refractory coagulopathy. A trial of hepatic artery embolization was unsuccessful and the patient succumbed shortly after. Conclusion: Liver amyloidosis can be fatal. It should be considered in any patient who present with features of ascites and hepatomegaly.
Keywords
Liver amyloidosis; Liver rupture; Hepatic artery embolization; Liver transplant
Introduction
Amyloid consists of aggregated fibrils of various proteins such as monoclonal kappa or lambda light chains in primary systemic amyloidosis or protein A in secondary amyloidosis. In most forms of familial amyloidosis the fibrils are composed of variant transthyretin. In amyloidosis associated with haemodialysis, the characteristic protein is beta 2 microglobulin. The amyloid fibrils are deposited extracellularly, destroying the affected tissues with disruption of normal organ function.
The most common clinical presentations of amyloidosis include: Nephrotic syndrome, restrictive cardiomyopathy, peripheral neuropathy and hepatomegaly, with elevated liver enzyme levels. Clinically significant liver involvement in amyloidosis is rare [1].
We report a case of liver amyloidosis proved by liver biopsy presenting with hepatic encephalopathy and died later from liver rupture.
Case Report
A 53 years old male with a history of dyslipidemia and diabetes mellitus on treatment presented to our hospital with a history of progressive abdominal distension over the last two months. This was associated with dyspnea, lower limbs edema and weight loss. No history of fever, jaundice, constipation, abdominal pain or gastrointestinal bleeding. His family history was unremarkable. He denied alcohol intake.
He was admitted recently due to spontaneous bleeding tendency. His hematological work up was un-remarkable and his bleeding was attributed to be aspirin related which was discontinued and he was discharged in a stable condition.
On physical examination he was hemodynamically stable with bilateral basal inspiratory crepitations. Abdomen was distended, not tender, no palpable organomegaly with positive shifting dullness. There was pitting edema of the lower limbs.
On laboratory testing the complete blood count, renal function, liver function tests and alpha-fetoprotein were normal except for serum albumin which was 23 g/l.
The patient was admitted as a case of ascites for investigations. Hepatitis work up was negative. Liver ultrasound showed normal liver echogenicity, no obvious focal hepatic lesion; portal and left, right and middle hepatic veins were patent. Analysis of ascetic fluid showed high Serum Ascites Albumin Gradient (SAAG), culture was negative and cytology was negative for malignancy. Gastroscopy showed small esophageal varices and mild portal hypertensive gastropathy. Echocardiogram was done which revealed ejection fraction 60 %, normal diastolic function; the wall thickness was 11 mm with no speckle seen. Electrocardiogram showed normal sinus rhythm.
Twenty four hours urine collection for protein urea showed nonnephrotic range protein urea with 819 mg protein per twenty four hours.
He was diagnosed as a case of cryptogenic liver cirrhosis and diabetic nephropathy and discharged on low dose diuretics in a stable condition after 18 days of admission.
One week after discharge he presented with decreased level of consciousness, of three days duration. He had no history of fever, abdominal pain, constipation, or gastrointestinal bleeding.
On physical examination, he was conscious but disoriented. His abdomen was distended with positive shifting dullness without tenderness. His repeated blood tests showed mild leukocytosis (14.3 × 109 cell/l) mainly neutrophil and pre-renal azotemia with Creatinine 204 μmol/l (normal 60-115 μmol/L).
Liver function tests showed serum albumin 23 g/l, Total bilirubin (TBIL) 76.8 μmol/l, Alkaline phosphatase (ALP) 640 IU/l (40-150 IU/l), Alanine aminotransferase was (ALT) 78 IU/l (<58 IU/l), Aspartate aminotransferase (AST): 110 IU/l (5-34 IU/l), Gamma Glutamyltransferase (GGT): 227 IU/l (12-64 IU/l), Ammonia level: 153 μmol/l (10-47 μmol/l), PT: 20 seconds, INR: 1.6, APTT: 48 seconds.
Now he was admitted as a case of acute confusion with rapid deterioration of his liver function tests, acute kidney injury induced by diuretics and presumed spontaneous bacterial peritonitis. His diuretics was stopped, he was started on intravenous hydration, and empirical intravenous antibiotic. His conscious level improved within two days. His renal function completely normalized on the 7th day of admission. He was restarted on diuretics with close follow up of his renal function. Ascetic fluid analysis ruled out spontaneous bacterial peritonitis.
During the admission he underwent full work up for liver transplant; repeated hepatitis serology and autoimmune profile were negative. Liver ultrasound showed signs of liver cirrhosis with hepatomegaly 19 cm, mild splenomegaly 15 cm and mild portal hypertension.
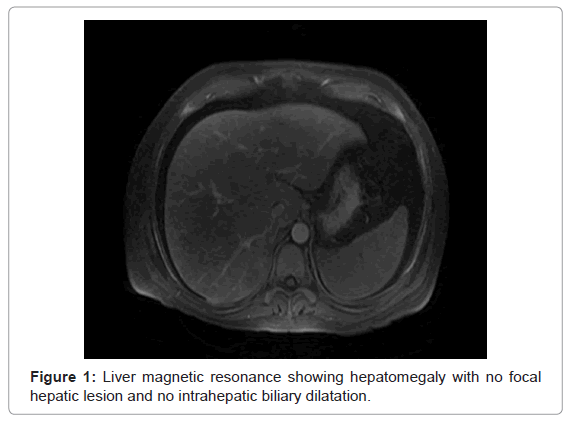
Hepatic vein thrombosis was ruled out by liver magnetic resonance venogram (Figure 1).
On day 12 of admission patient was prepared for liver biopsy to rule out any evidence of infiltrative disease. Patient underwent percutaneous liver biopsy under ultrasound guidance. This was preceded by ascetic fluid drainage.
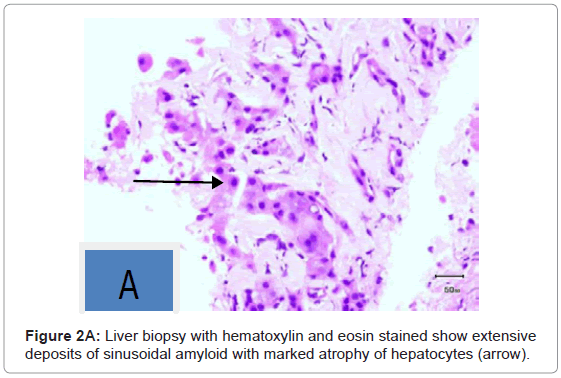
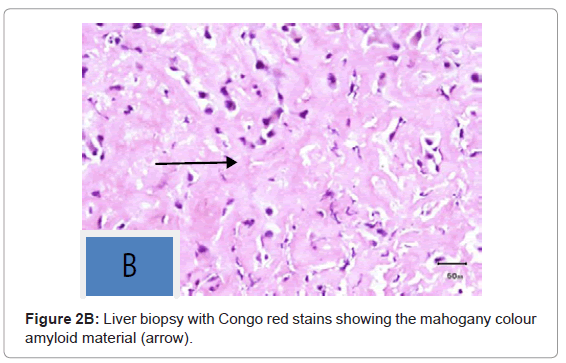
On pathologic examination it showed extensive deposits of sinusoidal amyloid with marked atrophy of hepatocytes (Figures 2A and 2B).
Three days later, he developed hypotension which responded initially to intravenous hydration. Later he was shifted to Intensive Care Unit (ICU) with impression of septic shock. He required inotropic support, and he was started empirically on Caspofungin, Vancomycin and Tazocin. Full septic screen was sent which showed no clear infectious etiology. His hemoglobin remained stable but he again developed renal impairment with creatinine reaching up to 164 μmol/L. His total bilirubin continued to increase up to 258.7 μmol/L (mainly direct 210 μmol/L) while other liver enzymes remained stable. His urine output decreased significantly and he became oligouric requiring dialysis. As a part of amyloidosis workup, he underwent rectal biopsy which was normal. Bone marrow biopsy showed hypercellular marrow with 5-10% abnormal looking plasma cells, some appeared in abnormal clusters with thickened blood vessels which were positive for congo-red stain. Kappa and lambda immunochemical stains were in-conclusive and cytogenetic studies were not performed. Serum protein electrophoresis was normal. Urinary Bence-Jones proteins were negative. Factor X level was 59% (70-120%). Skeletal survey could not be done due to the patient’s critical condition.
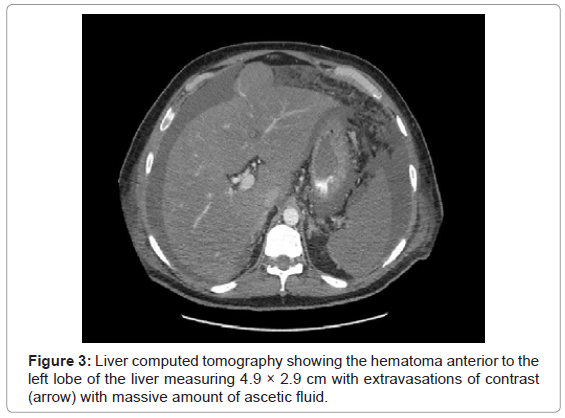
In view of the impression of systemic amyloidosis he was started on Dexamethasone 40 mg intravenous (IV), planned to continue for four days hoping to improve his coagulopathy. Five days after liver biopsy he started to have per-rectal bleeding, oozing from liver biopsy and central line sites. Dexamethasone was stopped and hemoglobin gradually dropped from 13.2 to 7.7 g/dl requiring significant blood and blood products transfusion. Diagnostic ascetic tap revealed hemorrhagic fluid. Liver rupture was confirmed by liver computed tomography scan (Figure 3).
The patient continued to bleed, required more inotropic support and eventually was intubated electively for upper and lower gastrointestinal endoscopies. The latter revealed pharyngeal bleeding with no sign of bleeding in the stomach and duodenum (mostly representing traumatic intubation) with no biopsy was taken from the stomach. There was active bleeding from the rectal biopsy site.
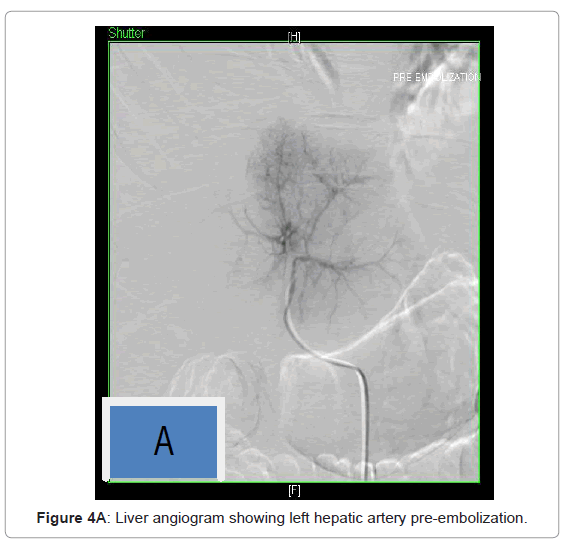
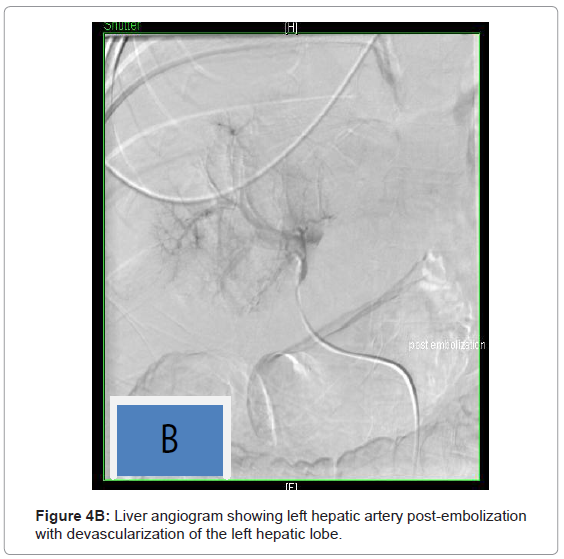
He underwent embolization of left hepatic artery, left branch of right hepatic artery and superior hemorroidal artery which failed to stop his bleeding. At the same time he had pigtail insertion for drainage of ascetic fluid around 6 liters was evacuated from the intraperitoneal hemorrhage. He was deemed not a surgical candidate due to his refractory coagulopathy (Figures 4A and 4B).
Despite significant resuscitative efforts he was still bleeding and required more blood and blood products transfusions. In the last 4 days of his life he received a total of 20 units of packed RBCs, 75 units fresh frozen plasma, 58 units cryoprecipitate, platelets 44 units, and factor VII 53 mg. His blood pressure gradually dropped till it was un-recordable, death was announced early morning of day 8 of ICU admission, secondary to hepatic failure, renal failure and refractory coagulopathy.
Discussion
The most common amyloid syndromes are the result of infiltration of the kidneys, heart, liver and peripheral nervous system. Hepatic infiltration is frequent in amyloidosis, but is rarely of clinical importance. At the Mayo Clinic from 1970 to 1980, 229 patients with primary systemic amyloidosis were examined. Kyle and Greipp [2] reported a 34% incidence of hepatomegaly due to liver involvement in amyloidosis with a modestly raised alkaline phosphatise activity in 16% of the patients. Hyperbilirubinemia was present in only 4% of the cases. Fatigue and weight loss were the most common initial symptoms representing 54% and 42% respectively [2].
A second study at the Mayo Clinic from 1960 to 1986, 80 patients with primary hepatic amyloidosis proved by liver biopsy pre-mortem was reviewed. Hepatomegaly was present in 83% of the patients. The alkaline phosphatase was high in 44% of the patients [3].
Liver biopsy still remains the definitive method of detecting liver involvement in amyloidosis. Three reported cases with clinically unsuspected primary amyloid light chain type of amyloidosis diagnosed by liver biopsy. These cases demonstrate that primary amyloidosis can present with liver enzyme abnormalities that dominate the clinical picture and that liver biopsy may be the initial diagnostic procedure of unsuspected primary amyloidosis [4]. Very rare complications after liver biopsy can occur and include clinically significant intraperitoneal haemorrhage. In 1988 at the Mayo Clinic study only two patients out of 80 had bleeding after liver biopsy [3].
Coagulopathy is frequently seen in patients with primary amyloidosis and several factors may contribute to bleeding complications such as deficiency of factor X, a decrease of vitamin K-dependent clotting factors, increased antithrombin activity fibrinolysis, and intravascular coagulation. Any of these mechanisms or a combination of them may explain the rare cases of hepatic and/or splenic rupture that have been reported in patients with amyloidosis [5].
The mean survival of patients with primary hepatic amyloidosis was 9-12 months. In 1986 Kyle and Greipp [2] established that the major risk factor affecting survival during the first year from diagnosis was the presence of congestive cardiac failure, followed by hepatomegaly, urinary light chains, and underlying myeloma [6].
Hepatic rupture in amyloidosis is extremely ominous, death occurs within hours to days. In review of literature there are thirteen cases of spontaneous hepatic rupture in liver amyloidosis which were managed by different modalities ranging from conservative to liver transplant. Three reported cases in hepatic amyloidosis died shortly after hepatic rupture [7-9]. Another two cases were managed successfully by conservative method [10,11]. Hepatic artery embolization was successful in two patients [12,13], while surgical ligation of the hepatic artery was successful in another patient [14].
A possible therapeutic approach for immunoglobulin light chain amyloidosis is Autologous Stem Cell Transplantation (ASCT). However the toxicity of ASCT limits its feasibility to a minority of patients. Eligibility criteria for ASCT were two or less organs are involved absence of severe cardiac involvement, creatinine 176.8 μmol/L (2 mg/dl) or less, age 65 years or younger and normal respiratory function tests [15]. A case report of a 55-year-old woman with primary immunoglobulin light chain (AL) systemic amyloidosis died due to spontaneous rupture of her liver following treatment with High Dose Melphalan (HDM) 200 mg/m2 in two divided doses, the following week and autologous stem cell transplant (HDM/SCT). Spontaneous rupture of her liver occurred 10 days after treatment with HDM/SCT and was complicated by septic shock. She was not eligible for surgical intervention and died shortly after [16].
The most effective method for treatment of secondary and familial hepatic amyloidosis is liver transplant. In review of literature there are four cases of hepatic amyloidosis complicated by liver rupture, which were treated successfully by liver transplant. First case was a 15-yearold boy case of hereditary autosomal dominant systemic lysosome amyloidosis that had spontaneous hepatic rupture, underwent urgent liver transplant and survived twelve years and later died from mesenteric hemorrhage [17]. His sister, at age of 24-years presented with hepatic rupture confirmed by computed tomography scan. Managed initially by selective embolization and 4 weeks later underwent liver transplant. More than 2 years after presentation, she remained well despite occasional episodes of amyloid-associated gastrointestinal hemorrhage [17].
Third case was a 34-year-old woman presented with abdominal pain and diagnosed to have hepatic rupture underwent orthotopic liver transplantation performed six days post hospitalization. She subsequently made a full recovery and reported well 4.5 years posttransplant without significant morbidity [18]. Fourth case was a 39-yearold female with kappa light chain amyloidosis. She presented with episodes of syncope. Computerized tomography showed acute bleeding from the right lobe of the liver. Despite therapeutic efforts, the patient continued to deteriorate, requiring emergent liver transplantation [19].
In our case the patient presented with rare clinical features of liver amyloidosis. He presented with decompensated liver failure, hepatic confusion, with hepatomegaly and elevated alkaline phosphatase approximately 4 times above the upper limit of normal. The primary indication for a liver biopsy in our case is unexplained hepatomegaly while he had all features of decompensated liver cirrhosis with liver span 19 cm with patent hepatic vein on liver ultrasound. Our patient had liver rupture 5 days after the biopsy which has been reported in patient with amyloidosis. His liver rupture cannot be atrributed to one factor while he had more than one liver amyliodosis ,percutenous liver biopsy and coagulopathy. He had refractory coagulopathy probably secondary to vascular involvement, factor X deficiency, a decrease of vitamin K dependent clotting factors, increased antithrombin III activity and disseminated intravascular coagulopathy. A trial of Dexamethasone intravenously was unsuccessful. Due to his rapid deterioration and his critical condition he did not receive any other chemotherapy. He did not benefit from hepatic artery embolization. The patient was evaluated for liver transplant but unfortunately, was not eligible for surgical intervention, liver transplant or autologous stem cell transplant due to rapid deterioration in his liver function tests and his refractory coagulopathy. He died 9 days after diagnosis secondary to hepato-renal failure and severe continuous bleeding.
Conclusion
Liver involvement in amyloidosis can be fatal. It should be considered in any patient who presents with features of ascites and hepatomegaly. Liver rupture has a poor prognosis and is an extremely rare complication of amyloidosis. Diagnosis is established by ultrasound or computed tomography scan. The mainstay of treatment is surgical, but mortality remains high (Table 1).
| Reported case | Management | Reference |
|---|---|---|
| 1. A 59 year old patient with a subcapsular hematoma of the liver with hepatic rupture secondary to amyloidosis. | Patient died during surgery | [7] |
| 2. A 46 year old patient with hepatic amyloidosis diagnosed premortem by liver biopsy. | Patient died | [8] |
| 3. A 52 year old patient with systemic amyloidosis complicated with multiple myeloma died suddenly of intraperitoneal haemorrhage due to spontaneous rupture of the spleen and liver. | Patient died | [9] |
| 4. A 46 year old patient with recurrent spontaneous hepatic rupture in primary amyloidosis diagnosed after surgical biopsy. | First rupture was treated by surgery while second was treated with cyclic Melphalan and Prednisone. | [10] |
| 5. A patient with amyloidosis complicated by reversible functional asplenia and spontaneous rupture of the liver with subcapsular hematoma. | Hematoma resolved completely with conservative therapy. | [11] |
| 6. A 48 year old patient case of multiple myeloma complicated by secondary systemic amyloidosis complicated by hepatic rupture. | Treated successfully by embolization of right hepatic artery. | [12] |
| 7. A 42 year old patient with primary amyloidosis experienced spontaneous hepatic rupture. | Transcatheter hepatic artery embolization. | [13] |
| 8. A case of primary systemic amyloidosis complicated by spontaneous hepatic rupture. | Treated by surgical ligation of hepatic artery. | [14] |
| 9. A 55-year-old woman with primary immunoglobulin light chain (AL) systemic amyloidosis died due to spontaneous rupture of her liver. | Treatment with high-dose Melphalan (HDM) 200 mg/m2 in two divided doses, the following week and autologous stem cell transplant (HDM/SCT). Spontaneous rupture of her liver occurred 10 days after treatment with HDM/SCT and was complicated by septic shock | [16] |
| 10. A 15-year-old boy case of hereditary autosomal dominant systemic lysosome amyloidosis, who had spontaneous hepatic rupture, underwent urgent liver transplant and survived twelve years and later died from mesenteric hemorrhage. | Liver transplant | [17] |
| 11. A 24-years presented with hepatic rupture confirmed by computed tomography scan. Managed initially by selective embolization and 4 weeks later underwent liver transplant. More than 2 years after presentation, she remained well despite occasional episodes of amyloid. Associated gastrointestinal haemorrhage. | Liver transplant | [17] |
| 12. A 34-year-old woman presented with abdominal pain and diagnosed to have hepatic rupture underwent orthotopic liver transplantation performed six days post hospitalization. She subsequently made a full recovery and reported well 4.5 years post-transplant without significant morbidity | Liver transplant | [18] |
| 13. A 39-year-old female with kappa light chain amyloidosis. She presented with episodes of syncope. Computerized tomography showed acute bleeding from the right lobe of the liver. Despite therapeutic efforts, the patient continued to deteriorate, requiring emergent liver transplantation. | Liver transplant | [19] |
Table 1: Reported cases of hepatic rupture in liver amyloidosis with different modality of management.
References
- Sandberg-Gertzén H, Ericzon BG, Blomberg B (1998) Primary amyloidosis with spontaneous splenic rupture, cholestasis, and liver failure treated with emergency liver transplantation. Am J Gastroenterol 93: 2254-2256.
- Kyle RA, Greipp PR (1983) Amyloidosis (AL). Clinical and Laboratory Features in 229 Cases. Mayo Clin Proc 58: 665-683.
- Gertz MA, Kyle RA (1988) Hepatic amyloidosis (primary [AL], immunoglobulin light chain): the natural history in 80 patients. Am J Med 85: 73-80.
- Haddad MG, Silverman JF, Larkin EW, Dellasega M (1993) Initial Diagnosis of Unsuspected Primary Amyloidosis (AL) by Liver Biopsy. Int J Surg pathol 1: 57-63.
- Kyle RA, Gertz MA (1995) Primary systemic amyloidosis: clinical and laboratory features in 474 cases. Semin Hematol 32: 45-59.
- Peters RA, Koukoulis G, Gimson A, Portmann B, Westaby D, et al. (1994) Primary amyloidosis and severe intrahepatic cholestatic jaundice. Gut 35: 1322-1325.
- Bujanda L, Beguiristain A, Alberdi F, Cosme A, Ruíz de la Hermosa J, et al. (1997) Spontaneous Rupture of The Liver in Amyloidosis. Am J Gastroenterol 92: 1385-1386.
- Ades CJ, Strutton GM, Walker NI, Furnival CM, Whiting G (1989) Spontaneous rupture of the liver associated with amyloidosis. J Clin Gastroenterol 11: 85-87.
- Okazaki K, Moriyasu F, Shiomura T, Yamamoto T, Suzaki T, et al. (1986) Spontaneous rupture of the spleen and liver in amyloidosis--a case report and review of the literature. Gastroenterol Jpn 21: 518-524.
- Kacem C, Helali K, Puisieux F (1998) Recurrent spontaneous hepatic rupture in primary hepatic amyloidosis. Ann Intern Med 129: 339.
- Levy-Lahad E, Steiner-Salz D, Berkman N, Chisin R, Levensart P, et al. (1987) Reversible functional asplenia and subcapsular liver hematoma--two distinctive manifestations of amyloidosis. Klin Wochenschr 65: 1104-1107.
- Mukhopadhya A, Raghuram L, Justus A, Joseph AJ, Eapen CE, et al. (2004) Transcatheter hepatic artery embolization for spontaneous rupture of amyloid liver. Indian J Gastroenterol 23: 26-27.
- Naito KS, Ichiyama T, Kawakami S, Kadoya M, Tabata T, et al. (2008) AL amyloidosis with spontaneous hepatic rupture: successful treatment by transcatheter hepatic artery embolization. Amyloid. 15: 137-139.
- Ooi LL, Lynch SV, Graham DA, Strong RW (1996) Spontaneous liver rupture in amyloidosis. Surgery 120: 117-119.
- Palladini G, Perfetti V, Obici L, Caccialanza R, Semino A, et al. (2004) Association of melphalan and high-dose dexamethasone is effective and well tolerated in patients with AL (primary) amyloidosis who are ineligible for stem cell transplantation. Blood 103: 2936-2938.
- Tam M, Seldin DC, Forbes BM, Connors LH, Skinner M, et al. (2009) Spontaneous rupture of the liver in a patient with systemic AL amyloidosis undergoing treatment with high-dose melphalan and autologous stem cell transplantation: a case report with literature review. Amyloid 16: 103-107.
- Mells GF, Buckels JA, Thorburn D (2006) Emergency Liver Transplantation for Hereditary Lysozyme Amyloidosis. Liver Transpl 12: 1908-1909.
- Loss M, Ng WS, Karim RZ, Strasser SI, Koorey DJ, et al (2006) Hereditary lysozyme amyloidosis: spontaneous hepatic rupture (15 years apart) in mother and daughter. role of emergency liver transplantation. Liver Transpl 12: 1152-1155.
- Croitoru AG, Hytiroglou P, Schwartz ME, Saxena R (2006) Liver transplantation for liver rupture due to light chain deposition disease: a case report. Semin Liver Dis 26: 298-303.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 15614
- [From(publication date):
specialissue-2013 - Nov 15, 2025] - Breakdown by view type
- HTML page views : 10899
- PDF downloads : 4715