Research Article Open Access
Kala-Azar Policy and Programmes in Nepal: An Assessment
Shiva R Adhikari*
Patan Multiple Campus, Tribhuvan University, Lalitpur, Nepal
- *Corresponding Author:
- Shiva R Adhikari
Patan Multiple Campus
Tribhuvan University
Lalitpur, Nepal
Tel: + 977-1-5526394
E-mail: sssadhikari@yahoo.com
Received Date: June 18, 2013; Accepted Date: July 16, 2013; Published Date: July 18, 2013
Citation: Adhikari SR (2013) Kala-Azar Policy and Programmes in Nepal: An Assessment. J Bioterr Biodef 4:124. doi: 10.4172/2157-2526.1000124
Copyright: © 2013 Adhikari SR. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Bioterrorism & Biodefense
Abstract
Background: Kala-azar (KA; visceral leishmanasis) is a debilitating and devastating disease, which targets the poor. KA first emerged in Nepal in 1980 and Government of Nepal (GON) has acknowledged the disastrous effects of the disease on domestic economic growth and community development through the explicit identification of KA as a health problem. Objective: The paper has twofold objectives: to describe the policies and plans with regard to KA in Nepal and to assess their overall effectiveness. Methods: The assessment is primarily based on secondary information. The data were collected from various policies and plans, reports, records in government offices, and published and unpublished documents among others. Data collected from various sources were triangulated and analyzed to produce mid-term assessment of elimination KA.
Assessment and conclusions: The existing KA policies and plans of the GON have rightly targeted the major areas of intervention of KA treatment, prevention and control – such as surveillance and early detection, provision of free drugs for KA treatment, demand side financing, insecticide sprays, health education and information among others. Outcomes of the intervention are improving, but in slow rate. Coordination among the KA affected countries is found rather weak. The existing policy is not sufficient to reduce the imported KA cases.
Keywords
Kala-azar; Elimination; Effectiveness; Policy and plans; Nepal
Introduction
Nepal, a predominantly rural economy characterized by low human development and the presence of endemic poverty, has made the health sector a priority for sustained economic development1[1,2], especially as the nature of the economy puts a premium on healthy labour input. Unfortunately, detriments to health abound, including infectious diseases, maternal and peri-natal disorders and nutritional deficiencies, which combined constitute 68% of the total burden of disease and 50% of total mortality; these figures are significantly higher as compared to neighbouring countries India and China [3,4]. Furthermore, communicable diseases such as Malaria and Kala-azar (KA; visceral leishmanasis) have been re-emerging as significant health problems in Nepal after their first occurrences in the 1980s [5].
KA that affected 100,000 people per year and 147 million people were at risk [6] has been considered as a major public health problem in three endemic countries of South Asia: Bangladesh, India and Nepal. The disease contributes almost 1306 DALYs (disability adjusted life years) loss per year [7] in these countries. They have been set up top priority to eliminate KA from these countries with high level political commitments by 20152. The five elements of strategy for elimination of KA in these countries include: access to early diagnosis and treatment particularly of the most vulnerable groups; strengthening disease and vector surveillance; integrated vector management; social mobilization and networking; and research [6].
Elimination of an infectious disease is a unique goal3. A number of studies confirmed [8,9] that elimination of KA is technically and economically feasible; however, it requires sufficient resources to produce desired outcomes. There are several challenges for elimination of KA, for example, KA is called one of the most neglected diseases [9,10]. It does not mean that this is not a serious disease so this is neglected by the people. This is one of the most serious diseases, if not treated, it is fatal. This is neglected because the investment made to fight it appears negligible compared to with the massive amounts expended [11] in other diseases, such as malaria and HIV/AIDS.
It was more than five years of implementing elimination of KA intervention in South Asia. The five years is important time period for the intervention because South Asian countries are familiar to design the five year development plans such as the 11th development plan of India [12], the 10th development plan of Nepal [4] and the sixth five year plan of Bangladesh [13]. On the other hand, this is the time for midterm evaluation of elimination intervention of KA. Each country should evaluate the implementation strategies of elimination of KA, so that the evidences can suggest the direction of implementation mechanism to improve effectiveness of intervention and to achieve targeted outcomes.
The paper has twofold objectives: to describe the policies and plans with regard to elimination of KA in Nepal and to assess overall effectiveness of the intervention by utilizing available secondary information. This grave detriment to Nepal’s economic growth has been acknowledged by the Government of Nepal (GON), as reflected in their past and present policies, plans and strategies.
The communicable disease KA4 which threatens almost one quarter of Nepal’s population [5] is both devastating and impoverishing by targeting those in poverty [8-11]5. The GON has acknowledged the necessity of maintaining a healthy population as a means of poverty alleviation [4] and, in this regard, has initiated measures for the control of KA and abatement of its disastrous effects on affected households (HH)6 after KA cases started to emerge in 1980 [14-16]7.
Materials and Methods
The paper adopts descriptive method to assess the outputs and outcome of KA related policy and programmes of Nepal. The analysis is based on the review of the past and present policies and plans of Nepal, as embodied in the development plans of Nepal, health sector policies, and activities conducted at different points of time. Methodological triangulation was employed to improve the accuracy of the information obtained. This is done through the use of various approaches, comparison of policy and its priority written in different documents and its priority, assessment of documents with different perspectives, etc. The comparisons of national and regional polices were conducted in order to increase convergent validity.
Past Policy and Plans
The GON was already embarking on its Sixth Development Plan (1980-1985) [17] when KA cases first began to appear in Nepal8. Unfortunately, the health sector policies and programmes were then being guided by the 15 year health perspective plan (1975-90) [18] and naturally, the perspective plan was unaware of KA incidence and its devastating impact on HH. Despite the appearance of KA in 1980 and the 604 cases of KA and 48 deaths in the subsequent five years, there were no specific programmes and activities to mitigate the disastrous effects of KA. For example, in the Seventh Development Plan (1985-90) [19], the GON simply adopted some general health objectives without outlining specific programmes for addressing the problem of KA [17]9.
In the 1990s, there was a change in the political regime, with the existing party-less Panchyat system being replaced by a system of multiparty democracy. The uncertainty resulting from this regime shift resulted in a gap of two years in the formulation of the Eighth plan (1992-97) [20], the preparation of which was guided by the recently promulgated National Health Policy (NHP) [21], whose major objective was to guide health sector development through strengthening the primary health care system at the local level10. Guided by the NHP, the Eighth Plan, which had embraced liberal market approach in its overall framework, set an objective of extending basic primary health services and curative services to rural areas [20]. This plan explicitly acknowledged KA as a health problem for the first time at the planning level. The Eighth Plan had likewise set targets for control of KA through insecticide spray, entomological surveys and provision of curative services to patients.
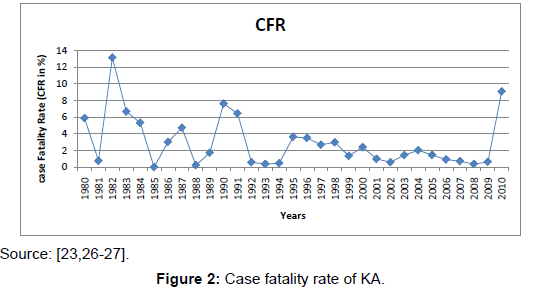
The subsequent Ninth Plan (1997-2002) [22] and the Tenth Plan (2002-2007) [4] acknowledged health care as a human rights issue and aimed to achieve perceivable changes in the health status through preventive, promotive, curative and rehabilitative health care services [22]. Targets were set at two levels: one for a plan period of five years and the other as a perspective plan for 20 years. By the start of the Ninth plan, the health system had been able to contain KA Case Fatality Rate (CFR), but the incidence of KA was still rising. As a continuation of the previous plan, the Ninth Plan included a component programme for the control of vector borne diseases including KA. Epidemiological surveillance—particularly the Early Warning and Reporting System (EWARS)—had been the additional ingredient in the Ninth plan, along with the formulation of a national guideline for vector borne diseases, which was also being prepared in 1997. During the period of the Tenth plan, the GON has committed to the regional strategy (with India and Bangladesh) to eliminate KA, with the target of achieving the disease elimination by 2015. The Elimination of Kala-azar divided in it into three phases: Preparatory Phase: 2005-2008; Attack Phase: 2008-2015 and Consolidation Phase: 2015 onwards. The programmes of the intervention included: early detection and timely appropriate treatment in KA endemic districts; indoor residual spraying two times in a year in highly affected KA areas; providing treatment and diagnostic services (using rK-39 diagnostic tools) and drugs (SAG, Miletefosine and Amphotericin B) at free of cost at the public hospitals; and proving transportation allowance for KA patients who received treatments from the public hospitals.
Due to political instability11, the five governments with leadership of different parties were come into power within last five year period. During this period, two ‘three years interim Plans’ for 2007 to 2010 and 2011 to 2013 were formulated respectively. These plans primarily focused on the continuation of previous strategies and programmes.
Present policy and plans
The present health sector policy of the GON is a continuation of those aforementioned activities. For example, the Second Long Term Health Plan (SLTHP; 1997-2017) [3] has identified KA as a disease with a high burden of disability adjusted life years (DALYs) lost – this has led to KA being included in the “Essential Health Care Services (EHCS)” in the SLTHP12. Further, in recognition that access has a central role in achieving equity in health, the SLTHP has highlighted the importance of ensuring universal access to health services in an equitable manner and has aimed to address access from all dimensions, including geographical/physical, economic, socio/cultural, and organizational access. In this context, the provision of free treatment to KA patients is considered a measure introduced to ensure economic access to the poor.
In accordance with the SLTHP, the Tenth Plan and successive periodic plans of GON adopted the “burden of disease” as a basis for prioritizing its programmes and has included KA control in the first priority “P1” Programme of the health sector. The objective of KA control activities has been to reduce incidence of KA to less than 1 case per 10,000 populations at district level by 2015, a continuation of the previous plan objectives except for a few physical targets [23]. For example, the national target, goals and strategies set by GON were: to reduce KA cases by 10% per annum; reduce mortality due to KA; strengthen quick identification and management of KA patients; improve follow-up of patients to increase the rate of complete recovery; and control sand-fly proliferation through integrated vector control measures13.
Furthermore, the aforementioned National Guidelines for vector borne diseases were revised to address new situations and make use of technological advances in medical sciences. This new guideline reiterated the goal of controlling KA adopted such as: Information and Education Campaigns (IEC), community participation, community surveillance, developing reliable diagnostic facilities, and integrated vector control measures. The guideline also identified several new areas for operational research, which included: KA case management at the peripheral level, evaluating treatment non-responsiveness of first line drugs, evaluation of an oral anti-KA drug, integrated vector control measures, and a few other behavioural/community measures to improve effectiveness in KA control in the future.
GON along with other India and Bangladesh has adopted the following strategies in the implementation of the KA elimination program in Nepal: a) improve program management; b) early Diagnosis and Complete Treatment (introducing new technology); c) Integrated Vector Management; d) Effective Disease Surveillance and Vector Surveillance; e) social mobilization and partnerships; and f) clinical, Implementation and Operational Research. Case detection and Treatment, indoor residual spraying in priority selected KA affected areas, proving transportation allowance to the patients and continuation of treatment through Miltefosine and Amphotericine B are major activities to implement the strategies.
Assessment
Achievements in Nepal
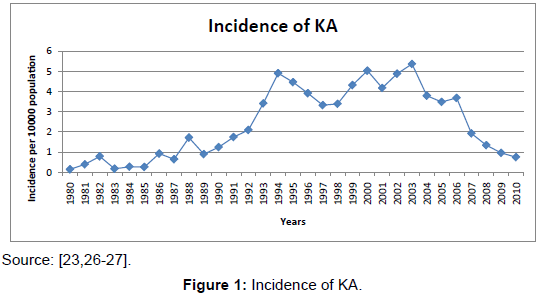
Nepal now has more than three decades of experience on prevention and treatment of KA. The past and present health policies and plans related to KA treatment have become more clearly enunciated and have tried to address the major dimensions of access to KA information, prevention and treatment. Furthermore, the provision of a surveillance mechanism at the community and rural health facility level has been devised to improve geographical access. However, despite these efforts by GON, the data in regard to KA cases, incidence and CFR over the period of three decades has been mixed. After implementation of elimination of KA, the incidence of KA has been falling down as shown in the following figures (Figure 1).
Indoor residual spraying in two cycles was conducted in KA endemic districts with 100% achievements against the set targets. Recently, the incidence of KA has decreased from 1.34 per 10,000 areas at risk population in 2008 to 0.96 in 2009 and to 0.75 in 2010. Out of the 12 districts, five districts have an incidence of more than 1, while 7 districts have an incidence of less than 1 case per 10,000 areas at risk population [23,26,27] (Figure 2).
The results suggest two opposite trends: first, the average KA incidence has been increasing, but at a decreasing rate, until 2003 cases per ten thousand populations; after implementation of elimination of KA, it has a decreasing trend; and second, the CFR showed a fluctuating trend. Generally, the results suggest that the percentage of patients receiving treatment and deaths averted has increased, leading to reduced CFR, while on the prevention side, there was strengthening of the effectiveness of KA detection, which is reflected in decreasing incidence of the disease.
The results showed some success in the journey of elimination of KA in Nepal; however, these figures probably even hide the magnitude of the problem as they reflect grossly underestimated hospital records that do not cover cases of morbidity or mortality of patients who had no access to hospital treatments - this makes an accurate estimation of prevalence difficult. These figures excluded the number of KA cases who came from outside Nepal14. The reported data suggested that more than 20% total KA cases came from India to obtain KA services from public health providers in Nepal [23].
Achievements in the regions
Elimination of KA is a public good and joint programme. The effectiveness of the intervention of a country can create the spillover effects to another neighbour country. It would therefore be helpful for Nepal to explore the outcomes of elimination of KA intervention of India and Bangladesh.
Available data suggested that KA cases in Bangladesh have remained steady at around 5000 yearly and reported deaths have declined to just one in 2010. The data seemed to show that there was a trend of decline in the KA incidence, but this did not prove to be consistent. Only 13 subdistricts (Upazilla) out of 102 reported more than 1/10 000 population; however, some of the sub-districts such as Fulbaria, Godagari and Mymensingh reported significantly KA incidences: 15.6/1000, 27/10 000 and 11/10 000 population respectively [28].
India has different story about the incidence of KA. The number of reported KA cases and deaths declined steadily only for two years after a peak in 2007 (44 533 cases and 18 deaths); however, since then numbers have gone up again. State of Bihar reported 22 756 cases which was more 70% cases of India and 18 deaths in 2010. The results suggested that the programme is not in “elimination mode” in India [28].
Recently Bhutan has reported KA total 22 cases from different 10 districts; however, Bhutan is not the part of the elimination programme. Bhutan aims to join the elimination programme because the country has not developed the national strategy for KA, treatment guidelines and training of health workers. Diagnosis was often late and under reporting is suspected due to a lack of awareness of KA in the country [28].
Discussions and Conclusions
The GON has acknowledged the devastating effects of KA, as reflected in their incorporation of KA-specific programs and targets in their policies and guidelines. Recently, the evidences on the effectiveness of these policies, plans and programs have been realized.
In 2003, KA cases peaked; since then a gradual decline has been observed. The elimination programme was launched in 2006, including IRS and free care in hospitals with food provided, and transportation costs reimbursed to patients. A sharp decline in incidence in endemic districts has since been observed, and in 9 of 12 districts the elimination target (<1/10 000 population) has been reached [23]. The results are further confirmed by the reported incidence of other vector born diseases such as malaria. Comparison of incidences of KA and malaria is logical because endemic areas of these diseases are same and the interventions are concurrently implemented in Nepal since last more than three decades.
Malaria burden in Nepal is on the decline as there has been a reduction of about 40% confirmed cases during the last five years. The experts have concluded that transmission of malaria in Nepal is low and that the program has moved forward from control to pre-elimination stage [23] (Table 1).
| Indicators | 2006 | 2007 | 2008 | 2009 | 2010 |
| Annual Blood Slide Examination Rate(ABER) per100 | 0.70 | 0.01 | 0.75 | 0.68 | 0.66 |
| Annual Parasite Incidence(API) per1,000 | 0.28 | 0.23 | 0.18 | 0.15 | 0.16 |
| Proportion P.falciparum (PF %) | 0.25 | 0.17 | 22.18 | 20.48 | 15.71 |
| Clinical Malaria Incidence(CMI)/1000 | 3.3 | 4.2 | 5.72 | 5.41 | 4.1 |
Source: [23].
Table 1: Malaria related indicators.
No doubt, KA is under-reported; data are obtained by passive surveillance only and most cases live in very remote areas. However, incidence of KA declined after introduction of KA elimination intervention. KA is declared endemic in 12 districts, all bordering India. The burden KA in India remained high. Nearly 50% of the problem of KA is in the districts located on international borders [29].
Current strategies are not sufficient and are not been very clear cut, casting doubt on whether the enunciated policies such as: surveillance and early detection, insecticide sprays, health education and information etc were put into practice. For example, regular exchange of information at the local level across borders did not happen. There is an institutional networking at the national level and among the research institutions; however, no institution relations or net working at the local level have been made. There are some other issues, the most probable of which is the formulation of domestic KA policy and plans without adequate follow-up and monitoring mechanism [30-32]. For example, in spite of policy enunciation for surveillance and early detection, the GON programmes regarding KA have largely relied on methods of passive detection, in which the KA patients themselves have to approach the public hospitals for diagnosis and treatment; this in contrast to an active detection, whereby the public health system itself is vigilant in detecting and treating cases. As a result, only those patients who have access to the health system can benefit from the existing provisions of free diagnosis and treatment for KA at public hospitals. The existing system of passive detection is likely to create a gap between those actually infected with KA and those with access to KA treatment. Since KA infected human population is the “human reservoir”15 for future KA transmission, untreated KA patients are potential agents for transmission and spread of KA. This suggests a need for re-focusing policy towards community outreach programs to detect and treat KA cases, which is also consistent with the present trend for decentralization. Similarly, insecticide spraying in endemic areas, another very important component of KA prevention, has not been put into practice and the quality of such sprays has been questioned [8,33]. The component of health education and information has also been ineffective. For instance, most of the KA patients approached the informal health service providers involving significant wastage of resources before reaching the public hospitals which are the only institutions for KA treatment in Nepal [8,33]16.
Elimination of KA is a national as well as regional public good. Negative externality of KA is found local to regional level, for example, leaving one infected individual behind will distribute the infection again. Delay in identification may enable the infection spread. A strong regional information network is required in order to fill an important gap in knowledge in implementation plan of KA elimination strategies. It will allow for a better understanding of the epidemiology of KA South Asia Region and contributes to the formulation of recommendations for a successful execution of the elimination programme. KA is a newly emerging disease in some countries, such as Bhutan, Sri Lanka. These countries should be brought into the part of elimination programmes.
Country level information network is also equally important. Updated epidemiological information is essential for measuring the output of the elimination programmes; but management related indicators need to measure the implementation status of elimination programmes. In order to measure the success of the elimination programme, process indicators need to be defined that, when regularly measured, will provide information on whether it is on track to reach the goal of elimination.
In conclusion, it is felt that the past and present KA policy and plans have been both well formulated and clearly enunciated, and it appears from the above evidences that the problem lies in the effective implementation of those KA programs. In other words, the GON should move away from the simple enunciation of KA policies and plans and towards their sincere implementation through adequate mechanisms of follow up and monitoring.
1The per-capita income of Nepal in 2011 was US $735 [1] and adult literacy rates were 61.23% for female and 83.36% for male. The country is struggling to overcome low health status such as a life expectancy of 70 years for female and 66 years for male [2].
2The Health Ministers from these countries have signed a Memorandum of Understanding on 18 May 2005 for the elimination of KA through inter-country cooperation.
3The KA endemic countries have defined elimination of KA as to reduce the annual incidence to less than one case per 10 000 population by 2015 at the district or sub-district levels in the endemic countries.
4KA is a disease caused by the bite of sandfly, a vector that feeds primarily on domestic cattle but sometimes feeds on human blood. People who keep cattle and share common spaces are likely to be infected by KA.
5Poverty is a cause as well as an important consequence of KA and this vicious cycle of poverty and disease makes KA one of the most intractable diseases in poor communities [8,16].
6A HH consists of persons living together and sharing the same kitchen for the last six months.
7At that time, an incidence of 1.5 per 100,000 populations and a case fatality rate (CFR) of 5.88% were reported.
8KA may have appeared earlier, but there was no recorded evidence of KA before 1980, which may be attributed to poor surveillance and awareness at that time.
9The primary objective of the Seventh Plan was to promote the physical, mental and community health of the general public and to provide basic health services to the maximum number of people, with the goal of reducing the death rate. The plan also aimed to increase longevity through promotional, preventive and curative health services, population control and extending maternity and child services.
10Thus, NHP adopted the policy of establishing at least one health unit for each of the Village Development Committees (VDCs), establishing a Primary Health Centre in each of the electoral constituencies and making available the services of Female Community Health Volunteers (FCHV) at the grass root level. It also adopted the policy of having local bodies share the responsibility for the management of health facilities. The provisions made in these policies reveal that the Nepalese policy makers expected that, if properly implemented, these mechanisms would ensure rural communities’ access to primary health care services at the local level, a phenomenon the government had not been able to bring about through earlier efforts.
11The period of domestic insurgency ended in 2007 with the Comprehensive Peace Agreement and Nepal started the process of writing own Constitution, having elected a Constituent Assembly. Unfortunately, the process is still ongoing with the term of the Constituent Assembly having expired and exercise being made to from an election government for another Constituent Assembly.
12The EHCS have been defined as priority public health measures targeted at addressing the most essential health needs of the population that are also cost effective. In addition, EHCS are those health services that would be made available at the district level and below in a manner that ensures the needy and underprivileged population are not deprived of the essential health care services because of the inability to pay [3].
13To secure effective KA control, respective responsibilities for referrals and record maintenance has been assigned from community level such as the FCHVs and Subhealth posts up to the zonal hospitals. To facilitate early detection, EWARS has been set up in the more endemic areas. With the purpose of more decentralized health care services, Primary Health Care Centers (PHCCs) have been provided with K-39 dipsticks and SAG (Sodium Antimony Glutamate, a first line drug) for identified KA patients which were previously limited to district and zonal hospitals. The district hospitals on the other hand are provided with facilities to conduct K-39 dipstick and bone-marrow aspiration and administration of both first line and second line drugs to patient referred from Sub- Health Posts (SHP), health posts (HP) and PHCs. The K-39 dipstick and first and second line treatments of KA are provided free of cost to the patients in the public health facilities. The supplies of these drugs are provided by the central government. A provision of doctors as well as trained lab assistants have been instituted to ensure case detection and administration of first line drugs in the PHCs of KA affected areas for. In addition to KA treatment, the government has adopted the policy of KA prevention through health education, environmental measures and insecticide sprays in the KA affected areas [24-26].
14Nepal has open border with India. There are free flow of labour, goods and capital between the countries. Primary endemic areas of KA are found in Bihar State of India. KA is confined in those districts which are adjoining with Bihar state of India. Some of patients have been coming to obtain KA care from Nepalese public health providers where they can get KA services at free of cost. Some of the Nepalese patients are visiting to Indian health care providers.
15KA found in Nepal is considered to be a non-zoonotic infection with man as the sole reservoir [5].
16In a study involving 61 KA households, only 18% of the KA patients started treatment seeking from the formal sector service providers such as health posts, PHCs, clinics, nursing homes run by registered doctors while 82% approached the informal sector (traditional healers, quacks, local drug stores etc).
References
- Ministry of Finance (MOHP) (2012) Economic Survey 2010/011 Ministry of Finance, Government of Nepal, Kathmandu, Nepal.
- United Nations Development Programme (UNDP) (2009) Nepal Human Development Report 2009: State Transformation and Human Development, United Nations Development Programme, Kathmandu, Nepal.
- Ministry of Health and Population (MOHP) (1999) Second Long Term Health Plan (1997-2017), Ministry of Health, Government of Nepal, Kathmandu, Nepal.
- National Planning commission (NPC) (2003) The Tenth Plan (2002-2007), National Planning Commission, Government of Nepal, Kathmandu, Nepal.
- Bista MB, Vaidya RG, Thakur GD, Pokharel RK (2004) The Annual Internal Assessment of Malaria and Kala-azar Control Activities 2002, Department of Health Services, Epidemiology and Disease Control Division, Ministry of Health and Population, Government of Nepal, Kathmandu, Nepal.
- World Health Organization/ South East Asia Regional Office (WHO/SEARO) (2005) Regional Strategic Framework for Elimination of Kala-azar from the South-East Asia Region (2005-2015). WHO Project No: IND CRD 714, World Health Organization/ South East Asia Regional Office, New Delhi, India.
- Cattand P, Desjeux P, Guzmán MG, Jannin J, Kroeger A, et al. (2006) “Tropical Diseases Lacking Adequate Control Measures: Dengue, Leishmaniasis, and African Trypanosomiasis”. Disease Control Priorities in Developing Countries. Second edition, Oxford University Press and The World Bank.
- Adhikari SR, Supakankunti S (2010) A cost benefit analysis of elimination of kala-azar in Indian subcontinent: an example of Nepal. J Vector Borne Dis 47: 127-139.
- Bhattacharya SK, Sur D, Sinha PK, Karbwang J (2006) Elimination of leishmaniasis (kala-azar) from the Indian subcontinent is technically feasible & operationally achievable. Indian J Med Res 123: 195-196.
- Yamey G, Torreele E (2002) The world's most neglected diseases. BMJ 325: 176-177.
- Ahluwalia IB, Bern C, Costa C, Akter T, Chowdhury R, et al. (2003) Visceral Leishmaniasis: Consequences of a Neglected Disease in a Bangladeshi Community. Am J Trop Med Hyg 69: 624-628.
- Remme JHF, Feenstra P, Lever PR, Médici A, Morel C, et al. (2006) Tropical Diseases Targeted for Elimination: Chagas Disease, Lymphatic Filariasis, Onchocerciasis, and Leprosy. Disease Control Priorities in Developing Countries, second edition, Oxford University Press and The World Bank.
- Planning Commission of India (PCI) (2007) Eleventh Plan (2007–2012) Planning commission of India, Government of India, New Delhi, India.
- Ministry of Planning Commission (MOP) (2011) Sixth Five year Plan (2011–15) Ministry of Planning commission, Government of Bangladesh, Dhaka, Bangladesh.
- Chelala C (2004) The poor man’s disease: The history and the present reality of a dastardly disease that hits the poorest in the poorest regions of South-Asia, Himal South Asian, March – April.
- Sharma BP, Maskay NM, Adhikari SR, Andrews JR, Joshi AB, et al. (2004) Socio-economic determinants of Kala-azar in Nepal. Journal of Nepal Health Research Council 2: 35-42.
- National Planning Commission (NPC) (1980) The Sixth Plan (1980-85), National Planning Commission, Government of Nepal, Kathmandu, Nepal.
- Ministry of health (MOH) (1975) The first long term health Plan (1975-90), Ministry of Health, Government of Nepal, Kathmandu, Nepal.
- National Planning Commission (NPC) (1985) The Sixth Plan (1985-90), National Planning Commission, Government of Nepal, Kathmandu, Nepal.
- National Planning Commission (NPC) (1992) The Eightth Plan (1992-97), National Planning Commission, Government of Nepal, Kathmandu, Nepal.
- Ministry of Health and Population (MOHP) (1991), National Health Plan Ministry of Health and Population, Kathmandu, Nepal.
- National Planning Commission (NPC) (1997) The Ninth Plan (1997-02), National Planning Commission, Government of Nepal, Kathmandu, Nepal.
- Ministry of health and population (MOHP) (2012) Annual report Department of health services. Ministry of health and population, Government of Nepal.
- Adhikari SR, Maskay NM, Sharma BP (2009) Paying for hospital-based care of Kala-azar in Nepal: assessing catastrophic, impoverishment and economic consequences. Health Policy Plan 24: 129-139.
- Adhikari SR, Maskay NM (2004) Health sector policy in the first decade of Nepal's multiparty democracy. Does clear enunciation of health priorities matter? Health Policy 68: 103-112.
- Ministry of health and population (MOHP) (2008) The Annual Internal Assessment of Malaria and Kala-azar Control Activities 2004 2005 and 2006. 2007, Epidemiology and Disease Control Division, Department of Health Services, Ministry of Health, Government of Nepal, Nepal.
- Ministry of health and population (MOHP) (2010) The Annual Internal Assessment of Malaria and Kala-azar Control Activities. Epidemiology and Disease Control Division, Department of Health Services, Ministry of Health, Government of Nepal.
- World Health Organization South East Asia regional office (WHO/SEARO) (2012) Leishmaniasis in the WHO SEA Region Epidemiological information on disease burden due to kala-azar in Bangladesh, India and Nepal. Report of an informal consultation Paro, Bhutan, 8-10 March 2011, World Health Organization, South East Asia regional office.
- Gupta A, Nagar M, Mishra SS, Lahariya C (2013) Visceral Leishmaniasis (Kala Azar) Elimination from Indian Sub-continent by 2015. Int J Trop Dis Health 3: 73-81.
- Pattanayak S (2001) Kala-azar: a potentially eradicable disease as a public health challenge. Indian J Public Health 45: 41-42.
- Thakur CP (2000) Socio-economics of visceral leishmaniasis in Bihar (India). Trans R Soc Trop Med Hyg 94: 156-157.
- Adhikari SR (2011) Underlying factors of healer shopping behaviour of Visceral Leishmaniasis Patient in Nepal. J Bioterr Biodef S6: 001.
- Pokharel S, Joshi AB (2003) In detecting visceral leishmaniasis (Kala azar) cases through existing control program Cost-Effective and early in Nepal. Journal of Nepal Health Research Council 1: 9-16.
Relevant Topics
- Anthrax Bioterrorism
- Bio surveilliance
- Biodefense
- Biohazards
- Biological Preparedness
- Biological Warfare
- Biological weapons
- Biorisk
- Bioterrorism
- Bioterrorism Agents
- Biothreat Agents
- Disease surveillance
- Emerging infectious disease
- Epidemiology of Breast Cancer
- Information Security
- Mass Prophylaxis
- Nuclear Terrorism
- Probabilistic risk assessment
- United States biological defense program
- Vaccines
Recommended Journals
Article Tools
Article Usage
- Total views: 14986
- [From(publication date):
December-2013 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 10540
- PDF downloads : 4446