Case Report Open Access
Isolated Intracranial Rosai-Dorfman Disease Mimicking Convexity Meningioma: A Case Report
Tetsuro Sameshima1*, Akio Morita1, Rokuya Tanikawa2, Toshiyuki Tsuboi2 and Ryuhei Kitai3
1Department of Neurosurgery, NTT Medical Center Tokyo, Tokyo, Japan
2Department of Neurosurgery, Abashiri Neurosurgical Hospital, Abashiri, Hokkaido, Japan
3Division of Neurosurgery, Department of Sensory & Locomotor Medicine, Faculty of Medical Science, University of Fukui, Fukui, Japan
- *Corresponding Author:
- Dr. Tetsuro Sameshima
Department of Neurosurgery
NTT Medical Center Tokyo
5-9-22, Higashi-Gotanda, Shinagawa-ku
Tokyo 141-8625, Japan
Tel: +81-3-3448-6111
Fax: +81-3-3448-6136
E-mail: tetsurosameshima@gmail.com
Received date: May 25, 2012; Accepted date: July 23, 2012; Published date: July 25, 2012
Citation: Sameshima T, Morita A, Tanikawa R, Tsuboi T, Kitai R (2012) Isolated Intracranial Rosai-Dorfman Disease Mimicking Convexity Meningioma: A Case Report. J Clin Exp Pathol 2:118. doi:10.4172/2161-0681.1000118
Copyright: © 2012 Sameshima T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Clinical & Experimental Pathology
Abstract
Abstract
Intracranial Rosai-Dorfman disease without systemic involvement is extremely rare. A 59-year-old woman
presented with headaches. Magnetic resonance imaging revealed an enhancing posterior fossa convexity lesion
with the dural tail sign. The preoperative diagnosis was meningioma. The histopathological examination revealed
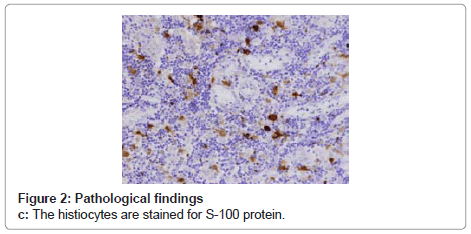
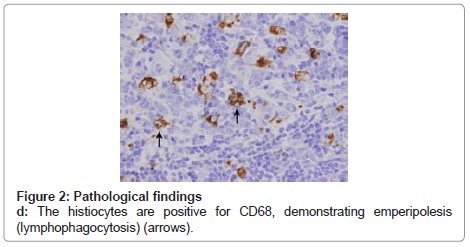
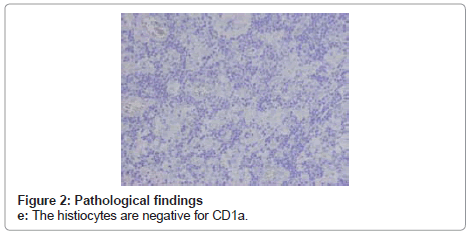
reactivity for S-100 and CD68 and non-reactivity for CD1a with emperipolesis (lymphophagocytosis) characteristic of
Rosai-Dorfman disease.
Keywords
Rosai-Dorfman disease; Meningioma; Emperipolesis
Introduction
Rosai-Dorfman Disease (RDD) is a benign histioproliferative disease of unknown etiology, first described by Rosaiand Dorfman [1], which causes bilateral painless enlarged cervical lymph nodes, fever, leukocytosis, Elevated erythrocyte Sedimentation Rate (ESR), and hypergammaglobulinemia. Extranodal involvement is believed to occur in approximately 25% to 43% of cases [2-4], but isolated intracranial RDD with no systemic involvement is extremely rare [4-16]. It is usually tightly attached to the dura mater and resembles meningioma in both clinical and surgical findings [2,3,6-10,13,15,17-19]. Meningioma usually occurs in middle-aged and older women, whereas RDD is more often seen in children and young adults and has a definite male predominance [4,7,8,17,12]. Histological and immunohistochemical confirmation is essential for definitive diagnosis. In addition to emperipolesis (lymphophagocytosis), reactivity for S-100 protein and CD68, but non reactivity for CD1aimmunostaining are characteristic features of this histioproliferative disease [9,11,15].
Case Report
A 59-year-old female presented with a 7-month history of headaches. Magnetic Resonance Imaging (MRI) at another hospital indicated a neoplastic lesion in the posterior fossa, so the woman was referred to this hospital. There were no neurological deficits, and a physical examination disclosed no extra cranial lesions. Laboratory examination of the blood revealed no abnormalities.
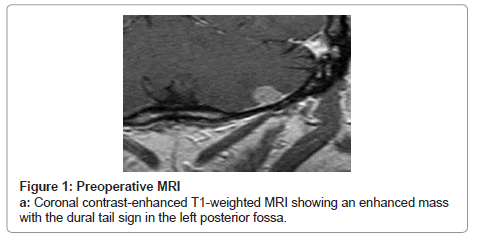
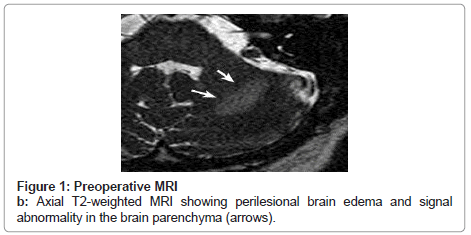
MRI showed a round-shaped mass in the left posterior fossa convexity that showed isointensity on T1-weighted imaging and low intensity on T2-weighted imaging. This was homogeneously enhanced with Gadolinium Diethylenetriaminepenta-Acetic Acid (Gd-DTPA) with the dural tail sign (Figure 1a). T2-weighted imaging revealed perilesional edema and a high signal abnormality in the brain parenchyma (Figure 1b).
The preoperative diagnosis was convexity meningioma. The patient underwent a suboccipital craniotomy, and a total excision of the lesion with the dural attachment was performed. The mass was whitish-gray, vascular, and elastic. It was arising from the cerebellar convexity dura, and loosely adherent to the pia mater.
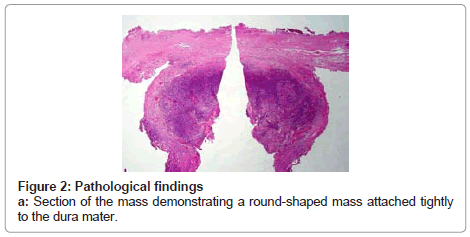
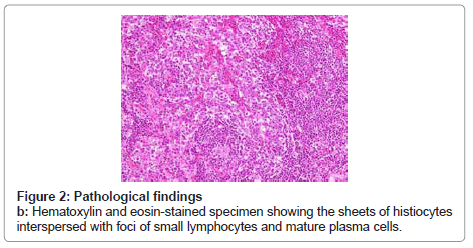
On histological examination, a round-shaped mass was tightly attached to the dura mater (Figure 2a), and there were sheets of histiocytes interspersed with foci of small lymphocytes and mature plasma cells (Figure 2b). Immunohistochemical staining showed that the histiocytes were reactive for S-100 protein (Figure 2c) and CD68 (Figure 2d), and were nonreactive for CD1a (Figure 2e). The histiocytic cells occasionally showed emperipolesis (lymphophagocytosis) (arrows) (Figure 2d). Four years after surgery, the patient is in good health without recurrence.
Discussion
RDD, also known as Sinus Histiocytosis with Massive Lymphadenopathy (SHML) [11,20], is a benign histioproliferative disease with systemic symptoms and lymphadenopathy that was first described by Rosai and Dorfman in 1969 [1]. It usually causes bilateral painless enlarged cervical lymph nodes, fever, leukocytosis, elevated ESR, and hypergammaglobulinemia. Lesions occur mainly in the systemic lymph nodes, but extranodal involvement has been reported in the skin, nasal cavity, soft tissue, orbit, bone, salivary glands, and central nerves [11]. Isolated intracranial RDD is extremely rare, with approximately 40 previously reported cases in the literature [2-6,9,11-13,15-19,21-24].
The most common findings of intracranial RDD on imaging usually suggest a dural based, extra-axial, enhancing mass, and most are resected as meningioma [2,3,6-10,13,15,17-19]. In most cases, however, rather than forming the well-demarcated, lobulated, rounded mass typical of benign meningioma, RDD infiltrates the brain, as shown by the continuous enhancement of the meningeal mass extending to the brain parenchyma, and on imaging it more closely resembles en plaque or malignant meningioma [21,22]. A further characteristic is that, although the lesion is small, brain edema and signal abnormalities on T2-weighted MR images are pronounced in RDD. This may explain why patients commonly experience headaches and seizures despite its small size. However, in cases such as this, when the tumor forms a rounded mass, differentiation from meningioma on preoperative MRI imaging is more difficult [9,13].
Microscopic examination of RDD typically reveals a polymorphous infiltrate of histiocytes, lymphocytes, and plasma cells in a fibrous stroma. The large histiocytes typically exhibit emperipolesis (lymphophagocytosis), which means that the lymphocytes are within the histiocytes. Emperipolesis is not unique to RDD and has been seen in other conditions, but it appears to be a prerequisite for the diagnosis. On immunehistochemical examination, these large histiocytes are reactive for S-100 protein and CD68, and are nonreactive for CD1a, a reliable maker 5 RDD, also known as Sinus Histiocytosis with Massive Lymphadenopathy (SHML) [17,11], is a benign histioproliferative disease with systemic symptoms and lymphadenopathy that was first described by Rosai and Dorfman in 1969 [1]. It usually causes bilateral painless enlarged cervical lymph nodes, fever, leukocytosis, elevated ESR, and hypergammaglobulinemia. Lesions occur mainly in the systemic lymph nodes, but extranodal involvement has been reported in the skin, nasal cavity, soft tissue, orbit, bone, salivary glands, and central nerves [11]. Isolated intracranial RDD is extremely rare, with approximately 40 previously reported cases in the literature [2-9,11,13,15,16-19,22].
The most common findings of intracranial RDD on imaging usually suggest a dural based, extra-axial, enhancing mass, and most are resected as meningioma [2,3,6-10,13,17-19]. In most cases, however, rather than forming the well-demarcated, lobulated, rounded mass typical of benign meningioma, RDD infiltrates the brain, as shown by the continuous enhancement of the meningeal mass extending to the brain parenchyma, and on imaging it more closely resembles en plaque or malignant meningioma [21,22]. A further characteristic is that, although the lesion is small, brain edema and signal abnormalities on T2-weighted MR images are pronounced in RDD. This may explain why patients commonly experience headaches and seizures despite its small size. However, in cases such as this, when the tumor forms a rounded mass, differentiation from meningioma on preoperative MRI imaging is more difficult [9,13].
Microscopic examination of RDD typically reveals a polymorphous infiltrate of histiocytes, lymphocytes, and plasma cells in a fibrous stroma. The large histiocytes typically exhibit emperipolesis (lymphophagocytosis), which means that the lymphocytes are within the histiocytes. Emperipolesis is not unique to RDD and has been seen in other conditions, but it appears to be a prerequisite for the diagnosis. On immunohistochemical examination, these large histiocytes are reactive for S-100 protein and CD68, and are nonreactive for CD1a, a reliable maker of Langerhans histiocytosis [9,11,15].
The origin and pathogenesis of RDD remain unknown, and an ideal treatment has yet to be identified. However, RDD is basically regarded as a benign histioproliferative disease, and the prognosis of RDD with CNS involvement is not poor. Complete surgical resection is generally regarded as being the most effective [8]. However, there have been reports of patients who required adjuvant radiation and chemotherapy for residual tumor or recurrent lesions [3,22], and more experience is necessary to elucidate the long-term prognosis.
References
- Rosai J, Dorfman RF (1969) Sinus histiocytosis with massive lymphadenopathy. A newly recognized benign clinicopathological entity. Arch Pathol 87: 63-70.
- Kim M, Provias J, Bernstein M (1995) Rosai-Dorfman disease mimicking multiple meningioma: case report. Neurosurgery 36: 1185-1187.
- Sharma MS, Padua MD, Jha AN (2005) Rosai-Dorfman disease mimicking a sphenoid wing meningioma. Neurol India 53: 110-111.
- Shaver EG, Rebsamen SL, Yachnis AT, Sutton LN (1993) Isolated extranodal intracranial sinus histiocytosis in a 5-year-old boy. Case report. J Neurosurg 79: 769-773.
- Andriko JA, Morrison A, Colegial CH, Davis BJ, Jones RV (2001) Rosai-Dorfman disease isolated to the central nervous system: a report of 11 cases. Mod Pathol 14: 172-178.
- Ghosal N, Murthy G, Visvanathan K, Sridhar M, Hegde AS (2007) Isolated intracranial Rosai Dorfman disease masquerading as meningioma: a case report. Indian J Pathol Microbiol 50: 382-384.
- Griffiths SJ, Tang W, Parameswaran R, Kelsey A, West CG (2004) Isolated intracranial Rosai-Dorfman disease mimicking meningioma in a child. Br J Neurosurg 18: 293-297.
- Kitai R, Llena J, Hirano A, Ido K, Sato K, et al. (2001) Meningeal Rosai-Dorfman disease: report of three cases and literature review. Brain Tumor Pathol 18: 49-54.
- Kitai R, Sato K, Kubota T, Kabuto M, Kawano H, et al. (1996) Meningeal sinus histiocytosis mimicking lymphoplasmacyte-rich meningioma. Case report. J Neurosurg 84: 1051-1054.
- Konishi E, Ibayashi N, Yamamoto S, Scheithauer BW (2003) Isolated intracranial Rosai-Dorfman disease (sinus histiocytosis with massive lymphadenopathy). AJNR Am J Neuroradiol 24: 515-518.
- Di Rocco F, Garnett MR, Puget S, Pueyerredon F, Roujeau T, et al. (2007) Cerebral localization of Rosai-Dorfman disease in a child. Case report. J Neurosurg 107: 147-151.
- Scumpia AJ, Frederic JA, Cohen AJ, Bania M, Hameed A, et al. (2009) Isolated intracranial Rosai-Dorfman disease with orbital extension. J Clin Neurosci 16: 1108-1109.
- Wu M, Anderson AE, Kahn LB (2001) A report of intracranial Rosai-Dorfman disease with literature review. Ann Diagn Pathol 5: 96-102.
- Gupta DK, Suri A, Mahapatra AK, Mehta VS, Garg A, et al. (2006) Intracranial Rosai-Dorfman disease in a child mimicking bilateral giant petroclival meningiomas: a case report and review of literature. Childs Nerv Syst 22: 1194-1200.
- Simos M, Dimitrios P, Philip T (1998) A new clinical entity mimicking meningioma diagnosed pathologically as rosai-dorfman disease. Skull Base Surg 8: 87-92.
- Udono H, Fukuyama K, Okamoto H, Tabuchi K (1999) Rosai-Dorfman disease presenting multiple intracranial lesions with unique findings on magnetic resonance imaging. Case report. J Neurosurg 91: 335-339.
- Horneff G, Jürgens H, Hort W, Karitzky D, Göbel U (1996) Sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease): response to methotrexate and mercaptopurine. Med Pediatr Oncol 27: 187-192.
- Franco-Paredes C, Martin K (2002) Extranodal Rosai-Dorfman disease involving the meninges. South Med J 95: 1101-1102.
- Jurić G, Jakić-Razumović J, Rotim K, Zarković K (2003) Extranodal sinus histiocytosis (Rosai-Dorfman disease) of the brain parenchyma. Acta Neurochir (Wien) 145: 145-149.
- Kattner KA, Stroink AR, Roth TC, Lee JM (2000) Rosai-Dorfman disease mimicking parasagittal meningioma: case presentation and review of literature. Surg Neurol 53: 452-457.
- Petzold A, Thom M, Powell M, Plant GT (2001) Relapsing intracranial Rosai-Dorfman disease. J Neurol Neurosurg Psychiatry 71: 538-541.
- Hadjipanayis CG, Bejjani G, Wiley C, Hasegawa T, Maddock M, et al. (2003) Intracranial Rosai-Dorfman disease treated with microsurgical resection and stereotactic radiosurgery. Case report. J Neurosurg 98: 165-168.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 14997
- [From(publication date):
July-2012 - Nov 22, 2025] - Breakdown by view type
- HTML page views : 10287
- PDF downloads : 4710