Investigation of Death Cases by Pesticides Poisonning in a Rural Community, Bignona, Senegal
Received: 25-Jul-2011 / Accepted Date: 20-Oct-2011 / Published Date: 25-Oct-2011 DOI: 10.4172/2161-1165.1000105
Abstract
This study gives the report of an epidemiological investigation of twenty nine deaths among fifty cases (global lethality rate was 58%) in a rural community which use widely pesticides and insecticides for agricultural purposes. A case control study with an environmental description has been realized. Serologic tests were performed to eliminate arboviruses aetiology. A qualitative investigation was undertaken, to evaluate the perception, the beliefs, and the population attitudes toward the infection and the inventory of the different pesticides used in the sites of study. In Africa, there are many incidents of domestic or professional poisoning with a fatal ending for which, few data are available, toxicological analysis are still a challenge.
Keywords: Poisoning organophosphate; Organochloride; Senegal
158502Introduction
Pesticide poisoning raises public health concerns around the world. As a matter of fact, 150,000 metric tons of pesticides are sold each year [1]. Pesticides use has dramatic consequences both in developed and developing countries. For example, a study of licensed pesticide applicators in Iowa and North Carolina was conducted. This study indicates positive exposure–response trends among pesticide applicators exposed to chlorpyrifos for mortality from external causes. Among external cause of death, mortality from suicide (codes X60–X84) and non-motor-vehicle accidents (codes W00–X59) were increased with lifetime exposure-days, with more than 2-fold relative risks in the highest category, although the suicide finding was restricted to Iowa applicators [2]. Another study in Sri Lanka shows that pesticide poisoning is the main cause of death, it represents 32.7% of all hospital deaths [3]. Despite the fatal side effects associated with the use of pesticides, they are widely employed. Pesticides and insecticides used for agricultural purposed are not the only source of poisoning. In fact, the ingestion of the most commonly used mosquito repellent, N,N - diethyl - m – toluamide (DEET) rapidly caused convulsions, severe hypotension, respiratory depression, coma and death [4]. Too often, farmers like Senegalese farmers have found themselves obligated to use pesticides to survive. Although dangerous, their choice is understandable because Senegalese farmers face a great deal of financial pressure and natural disasters. Senegal is one of the ten North and West African countries affected by locust invasions [5]. Locust is only one of the different potential pests capable of destroying entire crops. Agriculture is critical for the local population, 74.1% of a case population consisted of farmers [6]. Agriculture is often their only source of income. Unfortunately, the insects have been devastating the crops and pastures of a population entirely dependent on subsistence farming [5]. Farmers utilize pesticide to increase their harvests and profits. Given that pesticides are hazardous, they are detrimental to the population, water reserves and animals. Water resource contamination may persist for a long time after the last use of pesticides [7]. Pesticide poisoning can occur in various instances. Contamination can take place at work for the farmers, or at home. Residues of malathion, diazinon, or chlorpyrifos were found in 93% of homes, even though these compounds were identified as pesticides used in or around only 6% of homes [8]. The farmers’ households are at a relatively high risk for pesticide poisoning. Pesticide Action Network Africa investigated 11 villages in Senegal; the focus was on poisoning incidents related to consumption of groundnut treated with insecticide. In June 2004 treated groundnuts were used to prepare sauce in one household and all five family members who ate were poisoned, three of them fatally [9]. Between 1995 and 2004, various grouped deaths that occurred in the same communities have been reported in different areas in the Southern part of Senegal. In total 231 cases were signaled - lethality rate of 41.6%.This phenomenon have even affected the capital, Dakar along with other major cities [7]. Even though these fatal cases are rarely found in the literature, pesticide poisonings are always mentioned.
The mysterious death continued, on October 14th 2005 a total of 32 cases were reported in two villages of the sanitary district of Bignona. There were 13 deaths – a lethality rate of 41%. The chief regional doctor of Ziguinchor sent this alarming report to the Ministry of Health and Medical prevention. The chief doctor informed the Ministry of a disease characterized by neurological signs, syndrome of intracranial hypertension, cerebello-vestibular syndrome, convulsive seizures and an evolution that can often be fatal. The patients usually present these symptoms, dizziness, headaches, vomiting, diplopia, coordination troubles, language troubles, tremors, seizures and some of them die from convulsion or coma. The present study has two objectives: 1) to describe the epidemiological findings of the outbreak investigation that was conducted; 2) to present the recommendations which were addressed to the Health Authorities.
Materials and Methods
Studied population
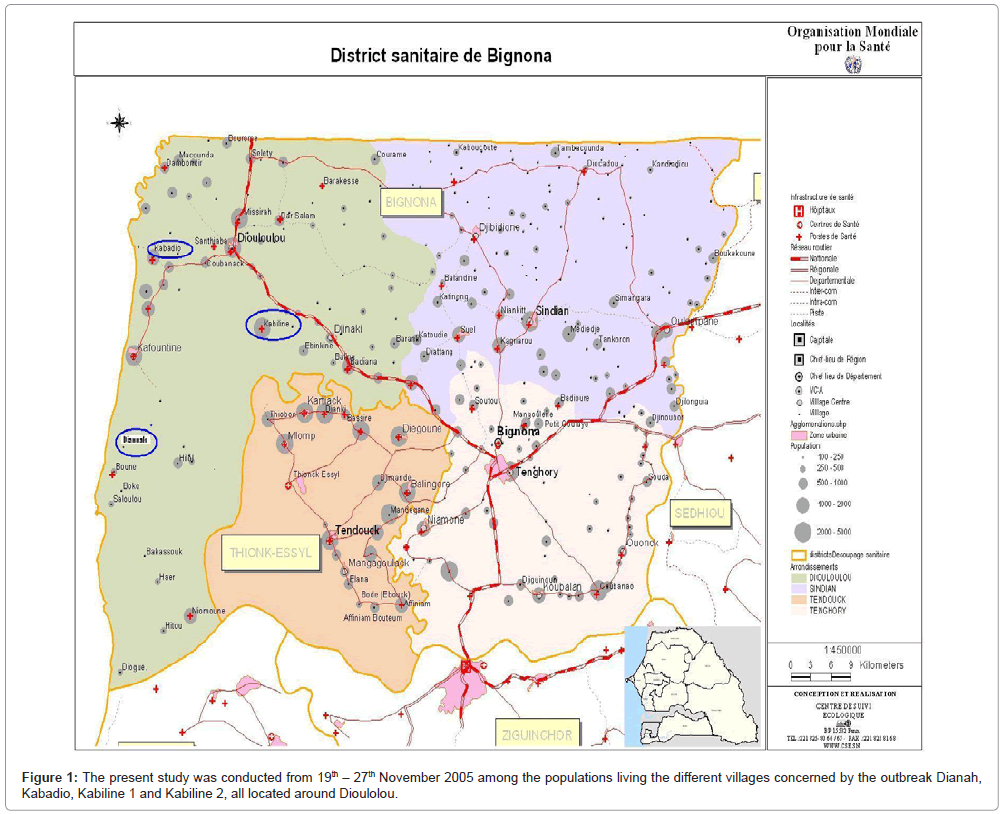
This present study was conducted from 19th – 27th November 2005 among the populations living the different villages concerned by the outbreak Dianah, Kabadio, Kabiline 1 and Kabiline 2, all located around Dioulolou (Figure 1). So, several individuals were interviewed: 1) the convalescents; 2) The healed sick individuals, 3) the parents of cases/ witnesses; 4) The witnesses of sick individuals (in the same family and in the neighborhood); 5) Healthcare personal; 6) The representatives of the related departments (agriculture); 7) The community leaders (village chief, imam, president of the rural community).
Two types of studies were conducted in the targeted sites:
• A quantitative investigation was performed in order to better describe the epidemiology of this infection. So, an exhaustive study of the cases that were reported to the health posts was accomplished, followed by an investigation case-control. A search of the documents in the register of consultation at the health post allowed the identification of patients who had the disease. All the cases paired by sex, age and marital status were interviewed and clinically examined. The Pasteur Institute of Dakar performed the laboratory analyses. Serologic tests to detect IgM for arboviruses (yellow fever, dengue 2, west Nile, Rift Valley Fever, Chikungunya virus, and the Crimea Congo), as described previously [10,11].
• A qualitative investigation was undertaken to evaluate the perception, the beliefs, and the population attitudes toward the infection and the inventory of the different pesticides used in the sites of study.
Results and Discussion
In total, 97 individual were interviewed among which 50 cases and 47 control. Out of 97 people, 54 blood samples were taken, 15 from the cases and 39 from the control. The missing blood samples were explained by the deaths that occurred before the mission and by the absences when we took the blood samples.
Characteristics of the socio demographic cases
At the study sites, we reported 50 cases with an average age of 25.6 years old (±18) and extreme from 3 to 84 years old. Twenty six cases (52%) were between 16-49 years old. This is the age group of workers that seemed the most affected by the disease. Regarding the cases employment, 70.2% declared being farmers, and in the small number fisher, breeder and storekeeper. About the education level; only about 23.4% went to a French school. Individuals of feminine sex were the most affected by the disease. As a matter of fact, 52% of the cases were women and 48% were men.
Disease description
The epidemic zone is composed of the villages of Diannah, Kabiline and Kabadio. Out of all the cases reported by the health care personal of the health posts of these villages since August 2005 (50 cases among which 29 death), the attack rate was 6 for 1000 at Diannah the highest and it was 3 for 1000 at Kabiline and at Kabadio. The lethality rate was 58.5% at Kabadio; the highest followed by Diannah 51.7% and Kabiline 57.1%. The first cases were noticed in the beginning of August and the peak is observed in October. The average period of evolution before death was 15 days for the village of Diannah, 10 days for Kabadio and 7 days for Kabiline with a maximum of 43 days and a minimum of 2 days at Diannah. The global lethality rate was 58%. When the investigation started 5 people were (10%) convalescents and 16 (32%) were healed. The evolution of the clinical prognostic seemed more favorable since the introduction of corticoids (Synacthene-retard) in the therapeutic care routine. In fact, we noticed a significant decrease of the number of deaths. The clinical signs encompassed mainly digestion impairments, vomiting and abdominal pain. Although less frequent, some patients presented central nervous system clinical signs, dizziness, headaches, coordination troubles, elocution troubles, tremor, seldom agitation, seizure and coma.
The virology results
The arboviruses search (yellow fever, Rift valley fever, Dengue, Chigungunya, Crimee Congo, West Nile) among cases and controls was negative.
The results of the complete blood count
In total, 97 people were interviewed, among which 50 cases and 47 controls. Among the investigated people, 54 were taken blood samples, 15 cases and 39 controls.
The erythrocytes: The average of all blood sample taking was 6.6 millions ± 2.2 erythrocytes. These values are included in the international range, which is from 4 to 10 millions. Thus, these values were normal for both groups: cases and controls.
The results were the same for the white blood cells. The values were normal for both groups. However, the hemoglobin count was slightly below the international norms. As a matter of fact, the average value was below 12.4 g/dl ± 1 and the international norms fluctuate between 13.5 and 17.5 g/dl. Nonetheless, there was not a significant statistical difference between both groups.
The toxicology results
The results of the activity of the enzyme cholinesterase in fmol/mn/ millions of erythrocytes/mm3 of blood or in SI unit were as follow:
The lowest value was 2 SI for one case and the highest was 73 UI for a witness. The average value for the cases was 21.56 ± 14.83 and for the controls the average value was 27.82 ± 17.49. We noted an important decrease of the activity of the enzyme cholinesterase for the cases. However, the difference was not statistically significant. Nevertheless, the low number of blood samples collected from cases (fifteen) could explain this result.
The values of the activity of the enzyme cholinesterase were lower for the samples taken in Diannah and for the hospitalized people from Kabiline. However, at Kabadio, its activity was greatly increased. The samplings done at Kabadio were mostly on witnesses.
The disease and the risk factors
The study of the data showed that the disease occurred the most among the age group 16-29 years old (52%) with feminin predominance, 52% against 48% for men. Among the investigated cases, 70.2% declared being farmers. The population, more precisely the youth were harvesting the crops of rice, corn and peanuts. Moreover, in the villages of Diannah and Kabadio the populations monitor the watermelon crops which require daily pesticides treatments. The women were very present in the crops harvesting activities. In fact, they assured the harvesting of the rice and they helped their husband with the peanuts and corn harvests. In Diannah, we noticed dangerous habits related to the storage of the corn seeds. As a matter of fact, in certain families, the corn seeds were stored in the attic, which has an opening to the room where individuals sleep. The pesticide fenitrothion is most dangerous in this condition because of the progressive intoxication due to the long term exposure and the lack of aeration. Out of five people who slept in this room, two were victims of food poisoning. At Kabiline, the introduction of tobacco crops increased the employment of pesticides to pulverize the fields.
Our investigation team found pesticides made of fenitrothion whether in solution or powder in most of the visited houses belonging to both the cases and controls. These products were stored in rooms where individuals slept. In addition to their use in the watermelon fields and for the seeds storage, the populations utilized them to kill insects in the beddings and rooms. The harvesting takes place during the same period as the rainy season which is characterized by the absence of aeration in the houses due to the humidity. During this season the beddings cannot be exposed to the sun. This observation could explain the fact that the phenomenon occurs each years at the same time. The deadly phenomenon starts in July with a peak between September – October – November. At this period, we noticed intense pesticide utilization.
The investigation was done among the pesticides handlers, the cases and controls families in this area showed that out of 13 types of products found, 5 are not approved by the Senegalese Authorities (among which Dimethoate 300 g/l and 400 g/l in EC, dimethoate (PA) organophosphosphate, endosulfan 35% EC (PA) and organochlorate). So, they are not distributed by the official services of agriculture. Despite the proven risks, the populations affirmed purchasing pesticides in parallel markets especially in Gambia, neighbor country.
Socio cultural consequences of the disease
The populations suspected that the disease has mystical origin so; to feel protected they did plenty of prayers and gave alm to avert fate. Moreover, in the Muslim ethnicity Diola, there was the practice of a rite name the “kabene” and sacrifices were made to avert the bad fate which is characterized by “a windblown by the spirits”. Despite this animist practices in the Muslim and Christian communities, the fatality and resignation was present in both communities.
The hypothesis of pesticide poisoning (organophosphates) either by inhalation or by accidental contamination of the food is based on the following observations:
• The appearance of the disease during the harvesting period of the crops where there is a high pesticides usage especially for the seeds storage,
• The presence in visited houses of pesticides that have not been approved by the official services of agriculture with a tendency of abusive and not appropriated utilization,
• The dominance of the working population involved in agricultural work among the subject of the disease,
• The subjects showed clinical signs that are similar the ones described in the literature in cases of poisoning by chemical products containing organophosphates or carbamate,
• The gathering of the cases at the same location rather than randomly in the different villages. In fact, in most of the visited houses, there is more than one case by household.
• The decrease of the activity of the enzyme cholinesterase in the cases, even though the difference between the cases and controls is not statistically significant.
From October 1st 1995 to January 31st 1996, 46 cases amount which 23 death (lethality rate of 50%) from an infection consisted of clinical manifestations of the central nervous system. These first cases were reported in the neighborhood of Kabrousse Mossor, sanitary district of Oussouye in the region of Ziguinchor. The clinical signs were composed of headache (91%), paralysis (85%), conscious troubles (72%), vomiting (67%), dizziness (46%), vision trouble (43%), dysphagia (33%). The investigation team noticed a decrease of the plasmatic and intraerythrocytic concentrations of cholinesterase in all cases. The team concluded that the cases suffered from pesticide poisoning due to the use of an Organophosphate (OP) utilized by the populations to treat the bedding. A second outbreak happened between May and October 2000 in the sanitary districts of Kolda and Sedhiou. There were 22 deaths out of 113 cases (lethality rate 19.5%) in the village of Diannah, sanitary district of Bignona. This unknown disease was characterized by thoracic pains, dyspnea, edema of inferior limbs and face. The investigation team hypothesized a carbamate and carbofuran poisoning. The carbofuran is contained in the products distributed with peanuts’ seeds. The following fatal event took place between October 2002 and January 2003, 31 cases and 20 deaths (lethality rate 65%). The cases suffered from myalgia, dizziness, vomiting, headache, dyspnea and convulsions. The most lethal outbreak occurred from, July to December 2004. The same symptoms as in Diannah were observed. But this time it happened in the villages of Mlomp and Thionkessyl in the sanitary district of Bignona. In total, 41 cases were reported, among which 31 deaths, for a lethality rate of 75.6%. The inappropriate and abusive usage of pesticides with uncertain origins in agriculture is to be blamed [12]. The two most lethal insecticides are the organophosphates and carbamates.
There are two possible reasons that could explain the high lethality rate due to pesticide poisoning. One reason is that there is the lack of qualified healthcare professional that are able to treat pesticide poisoning patients in rural areas. The other reason is that the diagnosis and the case management of poisoning are a real challenge in the health services [13]. There are different solutions. First, a more efficient formation of physicians to treat and diagnose pesticide poisoning cases is needed. Second, the government could play a critical role by regulating and banning the usage of pesticides that are too lethal. It is to be considered regrettable that the policy of distribution of pesticides in Senegal, which presents without any doubt a risk of poisoning, is not accompanied by better information to the farmers on the danger of these products, and of the necessary precautions to be taken during their use, in particular to wash hands, to use masks and gloves, and to deviate from the wind [6]. The organization of campaign awareness in the rural areas of Senegal could be an effective mean to inform the farmers of the potential risks associated with the usage of pesticides. Moreover, there is a safer and effective alternative to pesticides. A number of research institutions have even been studying the option of “biological warfare” – promoting the use of particular birds and specialized parasites hostile to locusts in an effort to reduce their populations (eighth plague).
In conclusion, the attitude of the population victim of this fatal event was ambiguous. We noted that some individual “refused” to go to the heath post because of superstitious reasons. During a MARP (mystical meeting to avert bad fate) at Kabiline 2, partakers talked about the fact that some ill people who received medical care at the community clinic passed away. Whereas the sick people who refuse to seek medical care survived. We also noticed a self exclusion phenomenon, of desertion the house of the deceased, feelings of fear, horror and anxiety.
Following the investigation, recommendations were formulated: 1) The improvement of the medical care of the cases; 2) Enhancement of the integrated surveillance of the diseases; 3) To strengthen the knowledge, attitudes and practices
These recommendations formulated after our investigation were finally taking into account. In fact, the Ministry of Health and Prevention organized a workshop to elaborate a plan to fight against chemical poisoning in the South of Senegal. The workshop took place from the 13th to 15th of April 2011. The organization of the workshop by the Ministry of Health and Prevention show the Senegalese authorities’ motivations to control and eradicate pesticide poisoning. The participants are the principle actors of the improvement of health in Senegal, among them to cite a few, the representative of the World Health Organization, the chief of Hygiene of Sedhiou and the chief of service of the poisoning center. The main objective of the workshop is the elaboration of a strategy to fight chemical poisoning in the 3 southern regions (Ziguinchor, Sedhiou and Kolda). It was decided to strengthen the surveillance of the borders to limit the usage of unapproved pesticides. The discussions and presentations raised some recommendations to be followed at both the regional and national levels.
References
- Miligi L, Aprea C, Settimi L (2005) Health risk and occupation in agricultural settings in Italy. Int J Occup Environ Health 11: 96-102.
- Lee WJ, Alavanja MC, Hoppin JA, Rusiecki JA, Kamel F, et al. (2007) Mortality among Pesticide Applicators Exposed to Chlorpyrifos in the Agricultural Health Study. its Environ Health Perspect 115: 528-534.
- Van der Hoek W, Konradsen F (2006) Analysis of 8000 hospital admissions for acute poisoning in a rural area of Sri Lanka. Clin Toxicol (Phila) 44: 225-231.
- Briassoulis G, Narlioglou M, Hatzis T (2001) Toxic encephalopathy associated with use of DEET insect repellents: a case analysis of its toxicity in children. Hum Exp Toxicol 20: 8-14.
- The humanitarian news and analysis service (2004) The Eighth Plague West Africa's Locust Invasion.
- Gomes Do Espirito Santo ME, Marrama L, Ndiaye K, Coly M, Faye O (2002) Investigation of deaths in an area of groundnut plantations in Casamance, South of Senegal after exposure to Carbofuran, Thiram and Benomyl. J Expo Anal Environ Epidemiol 12: 381-388.
- Tall A, AB Ly, P Nabeth, A A Sall, FD Sarr, et al. (2010) Epidemiological investigation of death cases by pesticide poisoning. Journal of Agricultural Biotechnology and Sustainable Development 2: 51-55.
- Castorina R, Bradman A, McKone TE, Barr DB, Harnly ME, et al. (2003) Cumulative organophosphate pesticide exposure and risk assessment among pregnant women living in an agricultural community: a case study from the CHAMACOS cohort. Environ Health Perspect 111: 1640-1648.
- Tall A, Diallo M, Faye O, Diab H, Diatta B, et al. (2009) [Crimean-Congo hemorrhagic fever in Senegal]. Med Trop 69: 18.
- Tall A, Sall AA, Faye O, Diatta B, Sylla R, et al. (2009) [Two cases of Crimean- Congo haemorrhagic fever (CCHF) in two tourists in Senegal in 2004]. Bull Soc Pathol Exot 102: 159-161.
- Sy MD (2003) Présentation de trois épidémies par intoxication aux pesticides en Casamance. Médecine d'Afrique Noire 473-474.
- Diop YM, Diouf A, Fall M, Thiam A, Ndiaye B, et al. (1999) Pesticide bioaccumulation: Measurement and levels of organochlorine residues in products of vegetable origin. Dakar Med 44: 153-157.
Citation: Touré K, Coly M, Toure D, Fall M, Sarr MD, et al. (2011) Investigation of Death Cases by Pesticides Poisonning in a Rural Community, Bignona, Senegal. Epidemiol 1:105. DOI: 10.4172/2161-1165.1000105
Copyright: © 2011 Touré K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 16692
- [From(publication date): 10-2011 - Dec 16, 2025]
- Breakdown by view type
- HTML page views: 11813
- PDF downloads: 4879