Case Report Open Access
Implementation of the Best Practice in Occupational Therapy “Assess Patients within 24 to 48 Hours of Admission” for a Stroke
Girard A1, Rochette A2,3*, Isabel N4, Laplante F5 and Lebeau A61Marie-Clarac Hospital, Canada
2Occupational Therapy Program, School of Rehabilitation, Faculty of Medicine, Université de Montréal, Canada
3Centre for Interdisciplinary Research in Rehabilitation of Greater Montreal (CRIR), Canada
4Maisonneuve-Rosemont Hospital, Canada
5University of Montreal Hospital Centre - Notre-Dame hospital, Canada
6Villa Medica Rehabilitation Center, Canada
- Corresponding Author:
- Annie Rochette
School of Rehabilitation
Université de Montréal
C.P. 6128, Succursale
Centre-Ville, Montréal (Québec)
H3C 3J7, Canada
Tel: (514) – 343 – 2192
Fax: (514) – 343 – 2105
E-mail: annie.rochette@umontreal.ca
Received Date: February 11, 2012; Accepted Date: March 15, 2012; Published Date: March 17, 2012
Citation: Girard A, Rochette A, Isabel N, Laplante F, Lebeau A (2012) Implementation of the Best Practice in Occupational Therapy “Assess Patients within 24 to 48 Hours of Admission” for a Stroke. J Community Med Health Edu 2:130. doi:10.4172/jcmhe.1000130
Copyright: © 2012 Girard A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Keywords
Knowledge translation; Acute stroke; Occupational therapy
Introduction
In neurology, new knowledge derived from research has been emerging at an astonishing rate, thus compelling health professionals, such as occupational therapists to regularly integrate the former in their practice. In order to facilitate the transfer of that new knowledge, various strategies are put forward, such as the production of systematic reviews and best-practice guides. The recommendations on stroke management published in the Canadian Stroke Strategy in 2006 and updated in 2008 are examples [1]. In spite of that type of initiative, a gap between the knowledge available for the practice of stroke occupational therapy and its use remains nonetheless [2-5]. Furthermore, that gap was observed by the occupational therapy services in two Quebec hospital environments where they noted response time for acute stroke clientele which did not comply with the recommendations issued in the Canadian Stroke Strategy. According to these recommendations, occupational therapists should begin their assessments and interventions in less than 24 to 48 hours post admission.
With a view to guiding the integration process of one of the best occupational therapy practices for a clientele having experienced an acute stroke, the Knowledge to Action Process [6], was chosen as the main conceptual framework. It showcases an approach which takes into account the stages required for a practice change among health professionals. Two cycles are brought together in that process, namely that of knowledge creation and that of action cycle. The former, through the funnel principle, aims at obtaining knowledge that is increasingly relevant for health professionals through three distinct stages, whereas the second contains seven dynamic stages through which knowledge is integrated or applied to practices. Thus, the objective is to experience the application of the first four stages of the action cycle of the model of the Knowledge to Action Process in order to promote an early response (< 24 to 48 hours post admission) in occupational therapy for a stroke clientele in acute care.
Methodology
Sample
Occupational therapists working with an acute-care stroke clientele in two hospitals (designated “Environment 1” and “Environment 2” in this article) from the city of Montreal are the population targeted by this project. As for ethical considerations, occupational therapists initiated the project themselves thus rendering them collaborators instead of participants. Verbal consent was obtained in order to proceed with the recording of the last meeting.
Study design
The first four stages of the action cycle of the model from Graham et al. [6], were used in this study in order to structure the knowledge translation approach. This study was also inspired by the philosophy of a participative approach by involving occupational therapists, the main knowledge users at each of the stages. It is indeed in that perspective that we will designate them as “collaborating occupational therapists.” According to Cargo and Mercer [7], this approach represents all the schools of thought (e.g. active participative research, participative research based on the community, etc.) sharing the same philosophy of promoting the commitment of knowledge users and beneficiaries in the research process. Prompting their participation thus aims at promoting the acceptance and belonging of knowledge brought to their practices.
The first stage (problem and knowledge identification) was carried out during a first meeting with collaborating occupational therapists during which were discussed their concerns in relation to one of the recommendations in occupational therapy and the knowledge which could support them. Further to that meeting, the researcher identified the knowledge (mainly in practice guides) allowing a response to occupational therapists’ needs. The second stage (knowledge adaptation) consisted in adapting knowledge to the practice context of occupational therapy in acute care. Collaborating occupational therapists were then invited to contribute to that reflection by commenting in writing on the information collected by the researcher, thus permitting a first knowledge acquisition approach on their part. The third stage (obstacle assessment) aimed at discussing the obstacles and facilitators encountered in the application of knowledge. In order to do so, the collaborating occupational therapists distributed the preliminary result of the knowledge translation tool to colleagues of the occupational therapy department who work with a stroke clientele to experience it for a period of approximately four weeks. Then, collaborating occupational therapists were invited to take part in a discussion led by the main researcher. It’s also during that last meeting that the fourth stage took place through the discussion of interventions or changes in their practice having taken place or which could eventually enable an improvement to knowledge use.
Data analysis
The content of the first meeting (stage 1) was kept using notes recorded in a diary. Then, at stage 2, participants issued an email to the researcher with an attached electronic document containing their comments. The content of the discussion was also recorded by means of notes in the diary in addition to being recorded on an audio track in order to facilitate the retention of the information contained during the meeting.
Knowledge adaptation was carried out using the Disability Creation Process model [8]. That model enabled organizing the recommendations arising from selected practice guides. As it pertains to the content of the meetings and comments, it was analyzed throughout the conduct of the stages, in real time, through the recording of notes in a diary.
Results
Participants
Three collaborating occupational therapists from two hospital environments participated in this project as representatives for their team. The collaborating occupational therapist from environment 1 works in a general neurology department. She consulted seven other colleagues from the department inter-program medicine and geriatrics part of whose clientele is admitted following a stroke. One of the two collaborating occupational therapists from environment 2 works exclusively with a stroke clientele while the other ensures the coordination of occupational therapy services in neurology and works with the general physical medicine clientele.
Stage 1: Problem and knowledge identification
Collaborating occupational therapists identified a gap between their practices and one of the recommendations issued in the 2008 Canadian Strategy, namely “to assess patients within 24 to 48 hours of admission” for a stroke. Further to exchanges with collaborating occupational therapists, the production of an action prioritization aid (assessments and interventions) based on best practices [9-11], was the targeted strategy in order to reduce that gap. Indeed, one of the concerns from collaborating occupational therapists was to be able to act efficiently with the acute care clientele in order to permit them to better manage their time.
Stage 2: Knowledge adaptation to the local context
Adaptation is a necessary process since the best-practice guides are not always designed in order to describe with great precision the interventions specific to each of the disciplines at a given moment of the care continuum. During that second stage, a chart enabled the gathering of all the best practices to then initiate a reflection with collaborating occupational therapists on the interventions which mainly apply to occupational therapists in their environment and those deemed priorities within the targeted response time (24 to 48 hours) with relation to the severity level of the stroke (mild, moderate, severe). Table 1 outlines an example of the classification carried out.
| Personal care | Role of the occupational therapist | Mild stroke | Moderate stroke | Severe stroke | Priority within 24 to 48 hours |
|---|---|---|---|---|---|
| Global personal care (E)* Evaluation of the performance and independence for clients having difficulty to carry out personal care (including personal care, excretory hygiene, clothing, health care) (A)* |
|||||
| (I)* In the event of difficulty to carry out that activity, offer specific training (training specific to the task and the use of technical help) (B)* | |||||
| (I)* The family and healthcare personnel should be notified of the techniques and equipment (technical help) required to optimize the performance in that activity (GPP)* |
Table 1: Excerpt from the recommendation classification chart for an early stroke response.
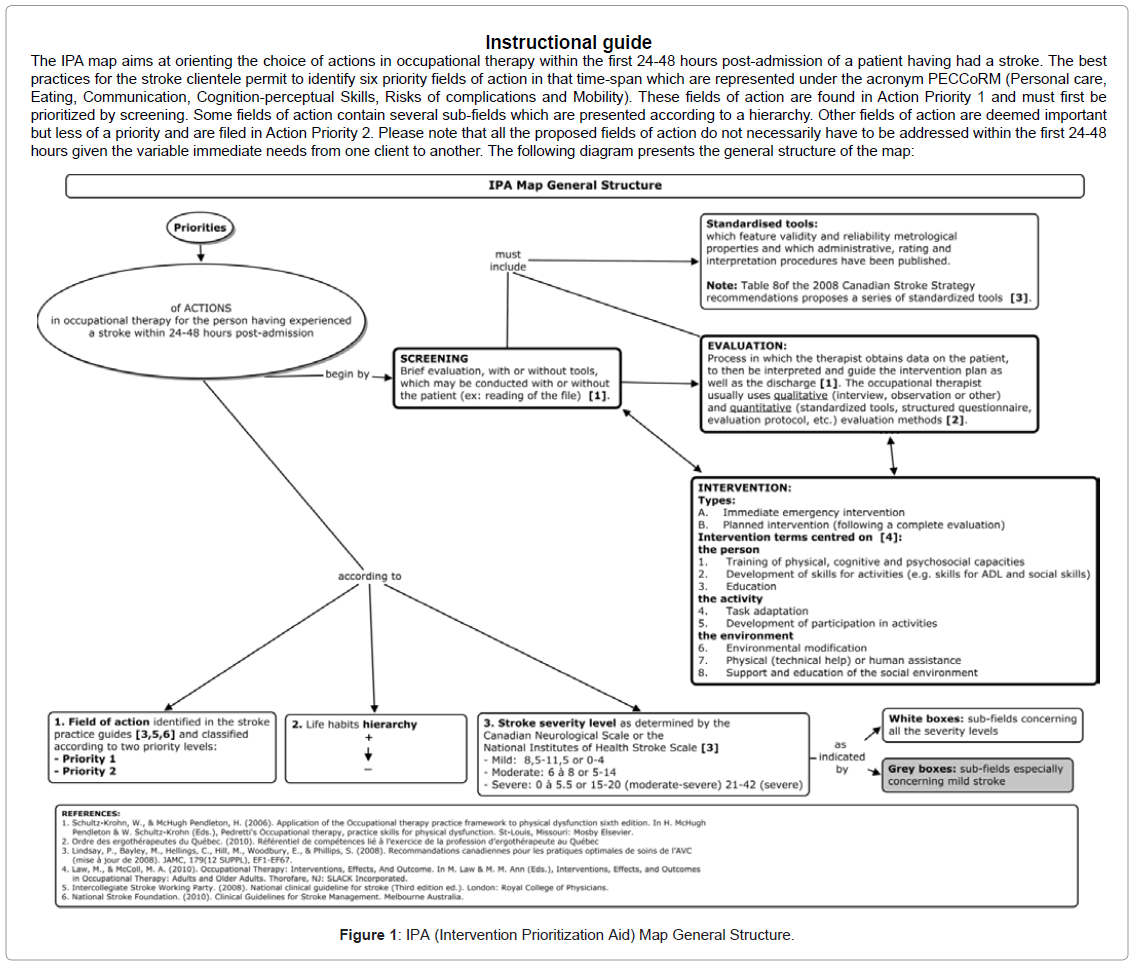
The reflection concerning priority actions was investigated further by the researcher who, using evidence-based data, established intervention priorities in compliance with the best practices. Most of the knowledge was ultimately illustrated in a concept map called IPA (Intervention Prioritization Aid) in order to facilitate knowledge translation (Figure 1).
Three aspects were considered in order to establish action priorities in occupational therapy for the person having experienced a stroke: the fields of action recommended by practice guides, lifestyle hierarchy and the stroke severity level.
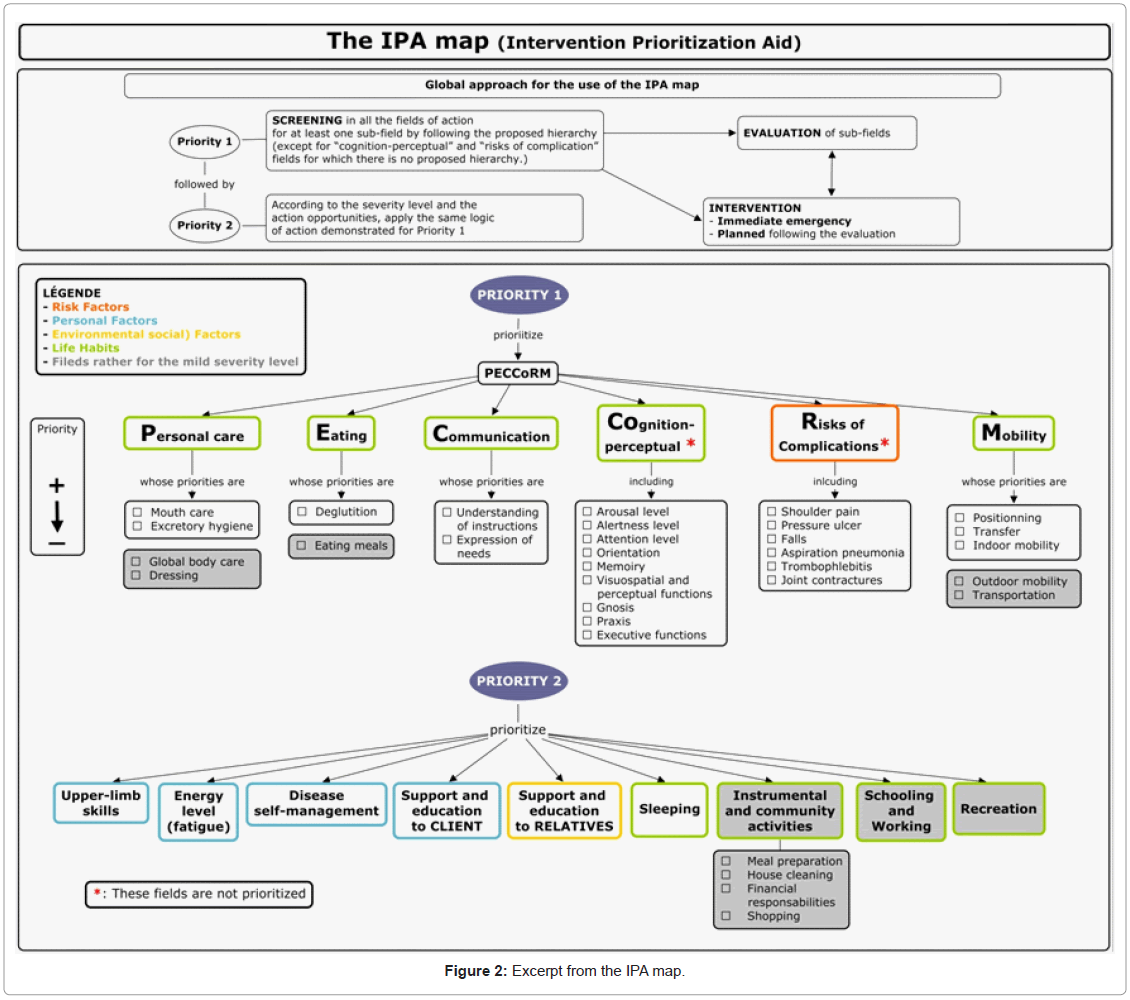
According to the literature, the important aspects to consider within 24-48 hours are gathered according to six fields of action represented under the acronym PECCoRM that is: Personal Care, Eating, Communication, Cognition-perceptual Skills, Risks of Complications and Mobility (Figure 2). Furthermore, the following themes emerge in the preparation of the discharge and in anticipation of early rehabilitation: sleeping, fatigue, support and education of relatives, self-sufficient management of the disease, upper limb skills, instrumental and community activities, education and work.
In order to further specify the elements to prioritize within a field of action, one must be reminded of the logic that survival activities and roles must be promoted prior to those linked to personal development which leads us to, for instance, prioritize the habit of eating to that of carrying out maintenance of the house. This justifies that the IPA map identified a priority level 1 (required for survival). Each field of action is detailed by a series of themes which possess a hierarchy, since one is a prerequisite for the other or is easier to carry out. For instance, for the field of mobility, good positioning in bed or armchair is a prerequisite to the transfer, indoor mobility, outdoor mobility and the use of a means of transportation. As it pertains to the various elements of the fields of action linked to cognition-perceptual skills and to risks of complication, they have not been prioritized.
The severity level of the stroke is based upon the person’s capacities during the acute stage and is divided into three levels: mild, moderate and severe. Since the functioning of a person having experienced a stroke differs according to the level of severity, the action priorities and the occupational therapists evaluation approach will thus differ from one person to another. For instance, for a person having had a mild stroke, the personal care will be evaluated by a quick screening whereas for a person having had a moderate or severe stroke, an evaluation using situation simulations will probably be required. Consequently, the occupational therapists priorities for a mild stroke will not necessarily be the same as for a moderate or severe stroke since, for the former, it is highly probable that the person already is independent for activities of daily living (ADL), whereas a person falling within the two other levels could need assistance. Incidentally, the occupational therapists evaluation for a mild stroke level will be further based upon the return home, in comparison with the evaluation for a moderate stroke, which will be focused on the rehabilitation potential, and the evaluation for a severe stroke, which will probably be further focused on the prevention of complications in a first phase. Hence, the IPA map proposes action priorities which must be considered based upon the occupational therapists clinical judgment with respect to needs specific to the person based upon the severity level and affliction type.
Stage 3: Evaluating the obstacles and facilitators in relation to the use of knowledge
The meeting with the collaborating occupational therapists permitted to identify the obstacles and facilitators encountered for knowledge application. First of all, the lack of time and high workload represent important organizational obstacles to early action with persons who have had a stroke. The service request process in occupational therapy was also identified as obstacles. Indeed, the admitted clientele is only known to occupational therapists once they receive the service request, which creates a delay between the client’s admission and case management. The fact that occupational therapists are not present on weekends and holidays also constitutes an obstacle to the quick case management in occupational therapy of clients admitted during those days. Other organizational obstacles were raised by the collaborating occupational therapist of Environment 1. Indeed, in the context of a general neurology unit, the general prioritization policies are applicable to all the clienteles and not only the stroke clientele. Consequently, there is no legitimacy in prioritizing a client who is admitted for a stroke rather than a client admitted for other health problems. Furthermore, in certain sectors, the clients with a stroke are sometimes transferred quickly which has the impact of decreasing the range of early actions for the latter and causing financial losses. As it pertains to the IPA map, even though it facilitates intervention prioritization, the former does not by itself allow a sufficient increase in the clients’ case management speed. Indeed, according to the collaborating occupational therapists, a more directional guide on evaluations and concrete interventions would have facilitated compliance with the recommendation. All the occupational therapists also raised the fact that Priority 2, which targets more the mild stroke clientele, seemed to them less adapted to their practice context. Indeed, according to them, during the first post-stroke days, the hospital reality sometimes makes the evaluation of complex activities more difficult, such as financial management and meal preparation, since the client must often undergo various examinations (cerebral scan, cardiac ultrasound, doppler, etc.) and is sometimes still located in the emergency room, an inappropriate environment for this type of evaluation. Moreover, the latter became aware that the little interest for this priority also comes from the fact that few clients having had a mild stroke were referred to them.
Collaborating occupational therapists identified certain facilitators in the improvement of their practices concerning the early action with their stroke clientele. First of all, the presence of persons coming from a university environment had the effect of energizing and guiding the necessary reflections to the practice change. Secondly, the IPA map reassured the collaborating occupational therapists in some of their practices while reminding them of the sometimes more neglected aspects of the action with the person having had a stroke (e.g. mouth care, continence).
Stage 4: Choosing, adapting and implementing interventions
The collaborating occupational therapists from the two hospital environments implemented interventions adapted to their context. Environment 1 occupational therapist developed a screening form (checklist type) designed from certain fields of action from the IPA map. This checklist allows to quickly make a necessary observations in order to identify the elements thus promoting client autonomy at the beginning of their stay in the emergency ward. It also targets the risks of complications which could adversely affect client recovery. Simultaneously, communication aid and important information transmission tools were developed in order to provide the healthcare personnel, client and family with precise guidelines depending on screening results. Therefore, that environment chose the intervention of creating tools permitting the access and quick transfer of knowledge, and that, in a screening context for complication risks and autonomystimulation for the stroke clientele within 24 to 48 hours post reception of the request.
With respect to Environment 2, two collaborating occupational therapists had begun a reflection on the strategies to improve their practice prior to the beginning of this project and this was resumed and fine-tuned during the conduct of the latter. Considering the low level of evidence of the recommendation to evaluate within 24 to 48 hours post admission (Level C), the reflection, faced with obstacles, was rather focused towards the definition of a realistic and acceptable delay considering the context and type of practice valued by occupational therapists. Their reflection also dealt with the strategies permitting early mobilization during their evaluations and through recommendations. Their objective is thus to produce a reference document which can guide the efficient preliminary evaluation of stroke clients within 72 hours post reception of the request while focusing on early mobilization.
The final meeting with the collaborating occupational therapists thus gave opportunity to share the various strategies implemented to favour knowledge application. Several questionings on the strategies of any of them emerged from that discussion. Consequently, it was possible to expand the collaborating occupational therapists’ perspective on the various approaches which could be used in order to ensure early action with the stroke clientele.
Discussion
The objective was to experience the application of the first four stages of the action cycle of the Knowledge to action process model from Graham et al. [6], in order to promote early action (< 24 to 48 hours post admission) in occupational therapy with stroke clientele. The objective was reached, since, on one hand, the four targeted stages of the model [6], were implemented and, on the other, several positive aspects in the practice of collaborating occupational therapists emerged in this project. Indeed, this project promoted knowledge translation, but also its application through the collaborating occupational therapists’ reflection on solutions adapted to their context and the sharing of the latter among the environments. Therefore, it allowed them to initiate a necessary change of practice for an early action with the stroke clientele.
Different interventions for each of the environments
During this project, different strategies were chosen by collaborating occupational therapists in order to facilitate knowledge application depending on obstacles encountered. Cabana et al. [12], developed a classification of obstacles to compliance with practice guides which was then developed further by Legare et al. [13]. The collaborating occupational therapists all identified external obstacles of the environmental type (lack of time and organizational limitations). This type of obstacles, according to the classification from Cabana et al. [12], tends to have an impact on the health professional’s capacity to adopt behaviour consistent with the practice guides. However, these obstacles were not to the same extent or did not occur the same way from one environment to another which influenced the knowledge application interventions implemented afterwards. Environment 1 targeted actions related to screening whereas environment 2 focused its actions on the client’s evaluation and mobilization. However, the two environments were faced with the same organizational feature, that is, the service request process which limited their objectives for the case management delays of admitted stroke clientele. Furthermore, environment 2 featured another obstacle in its lack of agreement with the recommendation of assessing within 24 to 48 hours. Environment 2 therapists perceived that it was more beneficial for the client and resource management to carry out a complete evaluation within 72 hours post reception of the request rather than acting earlier in a minimal manner without offering early mobilization interventions to clients. Thus, according to the classification [12], this may have influenced the attitude of collaborating occupational therapists from that environment towards the recommendation and motivated the strategies chosen by them.
Therefore, considering the various obstacles encountered the knowledge application interventions differed from one environment to another as it pertains to the chosen occupational therapy intervention process and the delay to carry it out. The intervention process of the two environments corresponded to that proposed in the IPA map. One advocated a change from screening to an immediate emergency intervention, if needed whereas the other targeted screening, then evaluation and immediate emergency interventions, also if needed. Moreover, although the Canadian Stroke Strategy recommends evaluating within 24 to 48 hours post admission, a guide in the United Kingdom proposes a delay of four business days for an evaluation note to be added in the client’s medical chart [9]. The two intervention strategies proposed by the two environments are thus in agreement with the literature and their differences reflect the conclusions brought forward by Ploeg et al. [14] and Wensing et al. [15], with respect to the importance of choosing knowledge application strategies according to the context of the environment and the obstacles encountered. Nevertheless, in order to give themselves every opportunity to reduce case management delays, establishments should manage some organizational obstacles. Their method of reference, for instance, could be modified by promoting systematic reference in occupational therapy for some clients such as those admitted for a stroke.
The intervention within 24-48 hours post admission with a mild-stroke clientele
The IPA map developed was designed considering the three levels of stroke severity. However, during this project, the collaborating occupational therapists noticed that the mild-stroke clientele was rarely referred to them. Consequently, some areas of Action Priority 2, which further target that severity level, seemed less relevant to them within 24 to 48 hours post admission. According to Duncan et al. [16], the persons having had a mild stroke are affected in all the dimensions of health (measured by the MOS 36-item short-form health survey or the SF-36) except as it pertains to pain. Also, the impact on their daily lives is significant, considerably affecting the level of participation of those persons within six months post-stroke [17]. With respect to the difficulties encountered by persons having had a mild stroke, it might be desirable for the latter to be referred more for occupational therapy prior to their return home. Especially since rehabilitation specialists, who, according to the Canadian Stroke Strategy [11], should be involved in the planning of the stroke clientele’s discharge [18], confirm the importance of expanding the case management perspective in acutecare occupational therapy by considering also more complex fields of activity such as participation at work, among the family and the community [18]. Considering the organizational obstacles raised by the collaborating occupational therapists for the evaluation of complex activities, that type of evaluation should undoubtedly be adapted to be a possibility in such a context by focusing, for instance, on screening and an efficient reference system towards other services. Incidentally, it should be noted that the IPA map was designed in order to present the action possibilities within 24-48 hours following admission and consequently, the fields of action presented do not have to be addressed in depth as a whole within that delay. It is through the quick screening influenced by the practice context and the client’s needs on which the occupational therapists actions will center. Thus, in an ideal world in which the mild-stroke clientele was referred to occupational therapists, Intervention Priority 2 should undoubtedly be considered for a client whose discharge is expected in a short time.
Model and approaches for knowledge application with occupational therapists
The “Knowledge to Action Process” [6], is the model which guided knowledge application during this project. The purpose of that model is to promote the use of knowledge by providing a framework that integrates the key stages of knowledge creation and application in the perspective of planned action theories. Even though that model acts as a guide through the stages of knowledge action, it nonetheless constitutes a long process which requires a lot of time. Hence, can occupational therapists be expected to use that model in order to improve their practices? That model was adapted by Metzler and Metz [19], for occupational therapists in order to further focus on the client, an approach that is highly present in that profession. If that adaptation enables a micro knowledge application and is better integrated in a daily practice, it nonetheless requires a great mobilization of resources. That is why a health professional should not be alone in the knowledge application process [20].
Considering that knowledge application affects several factors, including health professionals, managers, researchers and students, the latter should all collaborate together according to their competence level in order to contribute to that process. In the current project, the presence of external collaborators coming from the university environment was a facilitator in the knowledge application process for both hospital environments. That collaboration is integrated in a participative research approach from which this project was inspired in its methodology. That research approach has the advantage of producing knowledge which is adapted to health professionals’ needs, but also of facilitating knowledge appropriation [7]. Furthermore, Tolson et al. [21], in a study with nurses (n = 75) and older clients (n = 21), demonstrated the merits of this research type to promote knowledge application. The latter study also used a community of practices approach in order to develop the meaning of knowledge sharing among nurses. In our project, the collaboration among occupational therapists working with the same clientele in different hospital centres and having a common goal features similarities with those found in community of practices. This type of approach was also used successfully by Kilbride et al. [22] and Huckson and Davies [23], in order to promote knowledge application for health professionals working with a stroke clientele (n = 40 team members of the stroke unit) and for those working in a context of emergency care (n = 47 emergency care team). Considering the positive contribution of community of practices, the current project’s methodology could have been further based on its principles by being associated with an existing community of practices thus allowing for the expansion of the reflection process to more than two environments; particularly as this approach is currently used in Montreal with health professionals working with a stroke clientele in a project by Poissant et al. [24]. Finally, Wenger and Snyder [25], conclude on the importance of the managers’ presence in order to support practice communities in their approach and faced with encountered organizational obstacles. In this project, the managers were not directly involved even though they were informed of its evolution. Considering their influence on organizational obstacles and their role, according to the Social and health Ministry in participating in the development of a knowledge translation plan, it is possible to think that their direct collaboration would have been desirable [26].
Strengths and limitations
This project enabled the promotion of early action in occupational therapy with a stroke clientele by using an approach based on the model of the Knowledge to Action Process [6]. The approach was also influenced by an approach inspired by participative research thus permitting to obtain significant results for knowledge users. In spite of that, this project features a few limitations. A first limitation relates to the choice of knowledge, since the latter was not selected using an instrument. The use of an instrument such as the “Appraisal of Guidelines for Research and Evaluation (AGREE) Instrument” for the choice of practice guides would undoubtedly have been desirable [27]. However, that type of evaluation constitutes a long process which could not have been initiated within the framework of this project. In their study, Hurdowar et al. [28], took it upon them to conduct the exercise of qualifying practice guides for the stroke clientele, but could not be used in this project because the year of publication for the guides varied from 2000 to 2004. A second limitation deals with knowledge adaptation. Although the model specifies that it must be adapted to the local context, the project induced two hospital environments to collaborate making this stage arduous. Thus, the IPA map which resulted from that stage was designed in a conceptual form for practice in occupational therapy in an acute care context while giving room for clinical judgment. The adaptation of knowledge to the local context was carried out more during Intervention Stage 4 of the model, carried out by the collaborating occupational therapists in order to implement strategies in response to their context and obstacles noted. Finally, the last stages of model could not be carried out within the framework of this project which limits the long-term significance of the knowledge application process.
Conclusion
The aim which was to experiment with the application of the first four stages of the action cycle of the Knowledge to Action Process model [6], in order to promote early action in occupational therapy with the stroke clientele was achieved. This project enabled the redefining of action priorities in occupational therapy in the context of the stroke clientele within 24 to 48 hours post admission using the IPA map. The use of the Knowledge to Action Process and the collaboration of two different hospital environments with the university community emphasized the importance of adapting the practice guides to specific practice contexts and promoting collaboration among the various parties affected by knowledge application. If collaboration is highlighted as an essential element in the success of knowledge application, processes must also be provided in order to ensure effective communication among the various parties. In this study, a concept map was used in order to communicate the synthesis of knowledge. That strategy could be optimized in order for the map to be an actual central tool making possible the collaboration of all parties and evolving as knowledge is created.
Acknowledgements
Second author was supported by a junior career award from the Fond de recherche du Québec - santé (FRQ-S).
Declaration of Interest
The authors report no conflicts of interest.
References
- Lindsay P, Bayley M, Hellings C, Hill M, Woodbury E, et al. (2008) Recommandations canadiennes pour les pratiques optimales de soins de l’AVC. JAMC 179: SF1-SF29.
- Dumoulin C, Korner-Bitensky N, Tannenbaum C (2007) Urinary incontinence after stroke: identification, assessment, and intervention by rehabilitation professionals in Canada. Stroke 38: 2745-2751.
- Hammond R, Lennon S, Walker MF, Hoffman A, Irwin P, et al. (2005) Changing occupational therapy and physiotherapy practice through guidelines and audit in the United Kingdom. Clin Rehabil 19: 365-371.
- Menon-Nair A, Korner-Bitensky N, Ogourtsova T (2007) Occupational therapists' identification, assessment, and treatment of unilateral spatial neglect during stroke rehabilitation in Canada. Stroke 38: 2556-2562.
- Rochette A, Korner-Bitensky N, Desrosiers J (2007) Actual vs best practice for families post-stroke according to three rehabilitation disciplines. J Rehabil med 39 : 513-519.
- Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, et al. (2006) Lost in knowledge translation: time for a map? J Contin Educ Health Prof 26: 13-24.
- Cargo M, Mercer SL (2008) The value and challenges of participatory research: strengthening its practice. Annu Rev Public Health 29: 325-350.
- Fougeyrollas P (1995) Documenting environmental factors for preventing the handicap creation process: Quebec contributions relating to ICIDH and social participation of people with functional differences. Disabil Rehabil 17: 145-153.
- College of Occupational Therapists Specialist Section: Neurological practice (2008) Occupational therapy standards for stroke. London: Royal College of Physicians.
- Intercollegiate Stroke Working Party (2008) National clinical guideline for stroke. London: Royal College of Physicians: 175 p.
- Lindsay MP, Gubitz G, Bayley M, Hill MD, Singh S, et al. (2010) Recommandations canadiennes pour les pratiques optimales de soins de l’AVC (mise à jour de 2010). Ottawa, Ontario Canada: Réseau canadien contre les accidents cérébrovasculaires: 243.
- Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, et al. (1999) Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA 282: 1458-1465.
- Legare F, O'Connor AM, Graham ID, Saucier D, Cote L, et al. (2006) Primary health care professionals' views on barriers and facilitators to the implementation of the Ottawa Decision Support Framework in practice. Patient Educ Couns 63: 380-390.
- Ploeg J, Davies B, Edwards N, Gifford W, Miller PE (2007) Factors influencing best-practice guideline implementation: lessons learned from administrators, nursing staff, and project leaders. Worldviews Evid Based Nurs 4: 210-219.
- Wensing M, Bosch M, Grol R (2010) Developing and selecting interventions for translating knowledge to action. CMAJ 182: E85-E88.
- Duncan PW, Samsa GP, Weinberger M, Goldstein LB, Bonito A, et al. (1997) Health status of individuals with mild stroke. Stroke 28: 740-745.
- Rochette A, Desrosiers J, Bravo G, St-Cyr-Tribble D, Bourget A (2007) Changes in participation after a mild stroke: quantitative and qualitative perspectives. Top Stroke Rehabil 14: 59-68.
- Wolf TJ, Baum C, Connor LT (2009) Changing Face of Stroke: Implications for Occupational Therapy Practice. Am J Occup Ther 63: 621–625.
- Metzler MJ, Metz GA (2010) Translating knowledge to practice: an occupational therapy perspective. Aust Occup Ther J 57: 373-379.
- Rochette A, Korner-Bitensky N, Thomas A (2009) Changing clinicians' habits: is this the hidden challenge to increasing best practices? Disabil Rehabil 31: 1790-1794.
- Tolson D, Irene S, Booth J, Kelly TB, James L (2006) Constructing a new approach to developing evidence-based practice with nurses and older people. Worldviews Evid Based Nurs 3: 62-72.
- Kilbride C, Perry L, Flatley M, Turner E, Meyer J (2011) Developing theory and practice: creation of a Community of Practice through Action Research produced excellence in stroke care. J Interprof Care 25: 91-97.
- Huckson S, Davies J (2007) Closing evidence to practice gaps in emergency care: the Australian experience. Acad Emerg Med 14: 1058-1063.
- Poissant L, Ahmed S, Riopelle RJ, Rochette A, Lefebvre H, et al. (2010) Synergizing expectation and execution for stroke communities of practice innovations. Implement Sci 5: 44.
- Wenger EC, Snyder MS (2000) Communities of Practice: The Organizational Frontier. Harvard Business Review: 139-145.
- Ministère de la santé et des services sociaux. Guide: Profils de responsabilités de gestion, Fonctions types du personnel d'encadrement. Québec2006.
- AGREE Collaboration (2003) Development and validation of an international appraisal instrument for assessing the quality of clinical practice guidelines: the AGREE project. Qual Saf Health Care 12: 18-23.
- Hurdowar A, Graham ID, Bayley M, Harrison M, Wood-Dauphinee S, et al. (2007) Quality of stroke rehabilitation clinical practice guidelines. J Eval Clin Pract 13: 657-664.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 17109
- [From(publication date):
March-2012 - Dec 04, 2025] - Breakdown by view type
- HTML page views : 12265
- PDF downloads : 4844