Research Article Open Access
Human Factors and Bioagent Transmission following an Indoor Bioterror Attack
Jonathon Taylor, Ka Man Lai* and ZaheerAhmad Nasir
Department of Civil, Environmental and Geomatic Engineering, University College London (UCL), London, UK
- *Corresponding Author:
- Ka Man Lai
Department of Civil
Environmental and Geomatic Engineering
University College London (UCL)
Gower Street, WC1E 6BT, London, UK
E-mail: k.lai@ucl.ac.uk
Received Date: July 02, 2012; Accepted Date: July 25, 2012; Published Date: July 27, 2012
Citation: Taylor J, Lai KM, Nasir ZA (2012) Human Factors and Bioagent Transmission Following an Indoor Bioterror Attack. J Bioterr Biodef 3:116. doi: 10.4172/2157-2526.1000116
Copyright: © 2012 Taylor J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Bioterrorism & Biodefense
Abstract
The spread of bioagent through the population in a building following a bioattack is dependent on the built environment, the characteristics of the agent and the medium in which it is introduced, and the actions of individuals inside the building. While there has been a great deal of research on the spread of contaminants in indoor environments, many studies do not take into account the impact of human factors on bioagent spread and transmission. This paper discusses how bioagents may be spread through an indoor environment following an attack due to the behaviours and characteristics of the building population, in terms of their typical behaviour, as well as any emergency response measures they implement. Modelling methodologies are proposed which can be used to supplement existing air transport and Markovian models in order to take into account the actions and decisions of the building population.
Keywords
Bioterrorism; Indoor environment; Dispersion; Resuspension; Human factors; Transfer rates
Introduction
A bioterrorist attack on a building has the potential to cause illness and fatalities, fear and uncertainty in the building and wider population, and major financial costs from the remediation and displacement from the targeted building. The Anthrax attacks in the U.S. in 2001 lead to the death of five individuals, the infection of another 17, and total costs reported to exceed $1 Billion [1]. Due to the worldwide spread of biotechnology and biological skills, varying standards in laboratory security, bioweapon programs in unstable or rogue nations, and concerted efforts by some terror organisations to research and obtain bioagents, the risk of a bioterror attack in the near future is considered to be high [2].
A great deal of research and analysis has been performed on assessing the resilience of buildings to a bioterror attack. Reviews [3], guidelines [4-9], models [3,10-15], standards [16], and assessment methods [9,17-19], are all available to help determine the resilient of buildings to an attack, and guide decision-making in order to help defend against a bioterror attack. The risk posed by a bioagent to individuals within an attacked building will be dependent on the built form, engineering systems in place, the nature of the bioagent, and the behaviour of individuals within the building. Investigations into reducing the spread of a bioagent within a building have largely focused on modelling techniques that can predict the spread of bioagents in the indoor air (for example, multizone models [20] or Computational Fluid Dynamic (CFD) models [21]) or between individuals within the building (for example, Markovian models [22]), or on engineering systems that can be installed to control and prevent bioagent spread and enable evacuation or isolation of building occupants [3]. There has been less research into how human factors may contribute to the spread of bioagents, regardless of whether they are aware or unaware of the attack.
This paper reviews the potential pathways of bioagent dispersal and infection in a building, and how this may be influenced by the behaviour and other human factors of building occupants. The pathways of bioagent transport are discussed, and a literature review investigates how dispersal and infection through different pathways may be influenced by human factors and behaviours , regardless of whether building occupants are aware of the attack. Finally, modelling methodologies which can integrate human factors into models of bioagent spread are proposed.
Forms of threats
Bioagents can include pathogens (disease-causing agents) and biotoxins (poisonous substances produced by a living organism), and can cause illness and death, psychological turmoil (e.g. fear and anxiety) and economic and social instability to those affected. There are a number of pathogens and toxins that have been considered as possible bioterrorism agents [23]. The pathogenicity of the bioagent, the mode of contaminant delivery, the behaviour of the agent in the indoor environment, and the operating conditions of the building under normal or emergency conditions are all considerations when examining the risk to building occupants.
The risk from bioagents introduced to the indoor environment on surfaces or food will depend on the initial levels of bioagent deposited, the biological decay of the bioagent, and the probability of contact between individuals and the contaminated surface. The biological decay of pathogens can be dependent on the species, the environmental conditions, including the temperature and relative humidity of the indoor environment or the water activity of the media in which the agent is delivered, the surface type, and solar radiation levels [24]. The survival of pathogens can therefore be affected by the conditions of the indoor air, as well as the conditions on the internal building surfaces and the building envelope. The moisture conditions within the building material surfaces and in the indoor air may impact the growth and survival of bioagents on indoor surfaces, as high moisture conditions have been found to be related to the presence of mould, bacteria, protozoa, and viruses in the indoor environment [25]. Potential pathogens used in bioterrorism can exhibit a range of survival times in the environment.
In addition, many pathogens have mechanisms which can allow them to survive in the environment. Fungi and some bacterial species, for example B. anthracis, can form spores, allowing them to survive desiccation and remain viable for years (Table 1). The persistence of Category A agents in the environment was examined by [26], with a range of different survival times depending on the environmental conditions and the supporting media.
| Agents | Persistence in the transmission environment Level 1: Years Level 2: 8-24 hours Level 3: <1 hour |
Bioterrorism dissemination | Infective Dose |
| Inhalation Anthrax | Level 1: Very persistent | -Postal package - air dispersal and transmission - no person to person transmission |
8,000-50,000 spores |
| Plague Yersinia pestis | Level 3: not persistent | -Airborne (aerosol attacks), - 2nd transmission close contact (droplet borne) | 100 – 500 organisms |
| Smallpox | Level 3: not persistent | Airborne (aerosol attacks), close contact (droplet borne, fomites) dissemination of contaminated bedding and clothing | Assumed low (10-100 organisms) |
| Tularaemia | Level 1: Very persistent | airborne inhalation | 10-50 organisms |
| Viral hemorrhagic fevers | Level 2; Persistent | Surfaces, food | 1 – 10 organisms |
| Brucellosis | Level 2; persistent | Surfaces, Aerosols, Food | 10-100 organisms |
| Q-fever Coxiellaburnetii | Level 1; Very persistent | Air, surfaces | 1 – 10 organisms |
| Ricin toxin | Level 1; very persistent | Air, food, or water. | 3-5 mg/kg, LD50 in mice |
Table 1: Persistence, dissemination, and infectious dose of bioagents. [29]
Among the Category A agents, attacks through the airborne pathways are most likely. The risks posed by bioagents released as aerosols will depend on the initial levels of contaminant released, the aerodynamic properties of the contaminant or the media containing the contaminant, the physical and biological decay of the pathogen in the environment, and the movement of the contaminated air throughout the building. Aerodynamic properties that can impact the spread of a bioaerosol include the size, shape, and density of the agent or the media to which the agent is incorporated, while the physical decay of agents in the indoor environment refers to the loss attributable to physical factors such as unrestricted diffusion, surface impaction, and fall-out. Unrestricted diffusion allows the movement of aerosolized particles out of the zone where the pathogen was released into other areas within the building, or the external environment. This dilutes the concentration of the particle in the indoor air, but can also lead to the spread of the pathogen to areas of the building not directly targeted. Surface impaction refers to the attachment of contaminants to surfaces, while fall out refers to the deposition of the contaminant particles on surfaces due to gravity. Physical decay does not necessarily eliminate the threat, but may remove it from the indoor air, although the risk of re-suspension can exist [27]. Moreover, deposition of airborne bioagents on surfaces can potentially increase the dermal exposure level to the bioagents. Bioagents, such as Anthrax can cause health outcomes through dermal, gastrointestinal and respiratory routes [28]. Some bioagents can use the airborne pathways for dispersal and enter the targeted body part after deposition on surfaces and individuals touch these surfaces and pass the agents to the mucosal surfaces of the face, e.g. nose, mouth.
Depending on the type of bioagent used during an attack, an exposed individual may or may not be aware of having been contaminated, or even that an attack has taken place. While biotoxins may result in immediate symptoms, alerting the individual to their exposure, infectious bioagents are unlikely to cause immediate symptoms, and are likely to require an incubation period before symptoms appears. The incubation period for different agents varies, and can depend on the susceptibility of the infected individual. Within the period of incubation, an infected individual may infect other individuals that they encounter. Individuals may also be infected but not symptomatic, and may unknowingly spread infection.
Susceptible hosts are individuals who have an increased likelihood of contracting a disease when exposed to an agent. Those with an increased susceptibility can include the immunosuppressed, the very young, the unvaccinated, the malnourished and pregnant individuals. Because of the varying responses of individuals to an infectious agent, no single dose-response curve is applicable to everyone. The infection caused in an individual by a bioagent can depend on the pathway with which the individual comes into contact with the agent. Many agents are primarily spread through the respiratory pathways, while others are more likely to be transferred by direct contact due to their low survival rates when aerosolised. The pathway of infection can also impact the severity of the disease acquired by the infected individual. For example, B. anthracis is capable of causing both inhalation anthrax through respiratory pathways and cutaneous anthrax through direct contact. Inhalation anthrax is responsible for the vast majority of anthrax deaths, while cutaneous anthrax is rarely fatal.
The biological, physical, and built environment factors that can dictate the risk of infection to building occupants following a bioattack have all been subject to significant research, and in many cases models have been developed to describe their influence. Modelling the movement of contaminants in the indoor air due to the built form and building operation is well established, with a number of engineering models having been developed for this purpose. These models range from the basic zonal model, where each room within a building is considered a node, to complex fluid dynamic models which can predict the movement of contaminants in great detail according to well-defined boundary conditions. However, these models do not take into account the behaviour of individuals within a building, which may impact the spread of the contaminant and the rate of infection. The human interaction with the built environment, whether aware or unaware of an attack having taken place, may inadvertently contribute to the transmission of bioagent and determine if any prepared control measures and investment in biosecurity technology in the infrastructure are worthwhile. The human factors, in terms of their individual susceptibility to infection, their response to the attack and the following situation, their ability to attract and disperse the agent throughout a building, and the actions they take to evade or mitigate contamination may all have an important role which may alter the bioagent risks predicted by engineering models. In addition, understanding the risks to occupants through their own behaviour may help the occupants to reduce the risk of contamination, the authorities to identify potential contaminated or individuals, and security engineers and managers to better decide security measures integrated with human factors such as control, prevention, isolation and decontamination strategy (Table 1) [29].
Human factors
Direct and indirect physical contact pathways: Transmission through direct and indirect contact occurs when an individual touches a contaminated surface or individual. The individual may then cause secondary contamination by touching additional surfaces throughout the building (person-to-surface), or other individuals (personto- person). Surfaces such as tap faucets, door knobs, phones, and keyboards have all been investigated as being reservoirs for infectious microorganisms in hospital environments due to the regularity of human contact [30]. As discussed above, the survival of the bioagents in the environment will also impact the transfer rate between contaminated surfaces and a contacting individual, as some species may not survive long enough to be transferred after a period of time.
The movement of contaminated individuals throughout a building, and the surfaces and individuals that the contaminated individual comes in physical contact with will dictate the spread of the bioagent through direct contact. Understanding the networks of social contacts developed by individuals within the building has been suggested to predict the transmission of infection [31]. Space syntax techniques can be used to understand the typical movements inside a building, while access cards and surveillance video can be used to try and trace the movements of individuals.
Bioagents are not a threat to human health unless they can access the targeted part of the human body at or above the infectious dose. Transfer of an agent from the skin to the nose, mouth, or eyes can cause agents to gain access to the body and cause an infection. Nose-picking and eye rubbing are typical high risk behaviours and contribute to an increase in infection risk. Observations of individuals in an amphitheatre suggests that one out of every three people picked their noses when no one was looking, while the rate was lower in a conference setting when individuals were sat facing each other [32]. The transfer rates from fingertips to lower lips for different bioagents has been examined [33], with the transfer efficiency for the viral PRD-1 bacteriophage (33.90%), the Gram-positive Micrococcus lutues (40.99%), and Gram-negative Serratiarubidea (33.97%) all showing a high transfer fraction. In cases where food or water is the vector, ingesting the contaminated object will be the primary means of infection.
Person-to-surface transfer rates: Infection through contact with contaminated environmental surfaces has been gaining increasing attention as an important pathway in disease transmission [34]. The infection of individuals due to contact with contaminated surfaces poses a threat following a bioattack when the agent has been applied directly to a surface, or following an aerosol attack where the agent has deposited on a surface due to impaction or deposition. In addition, contaminated individuals may spread the bioagent to secondary surfaces through direct contact. The transfer of contaminants between surfaces and the skin of individuals, usually assumed to be through hand contact, has been examined by a number of researchers.
The transfer rates of bacteria from surfaces to fingertips has been shown to be higher from non-porous surfaces than from porous surfaces [33,35,36]. In addition, the type of bacteria [33,36], the time following the inoculation of the surface [35], the moisture levels of porous surfaces [37], and the inoculum size [38] can impact the transfer fraction of bacteria to contacting hands.
Viruses have been found to transfer readily between surfaces and individuals skin upon contact. The fraction of virus transfer between skin and surfaces appears to be dependent on the type of surface, with non-porous surfaces [33] showing higher transfer rates, the virus species, and hand cleanliness (recently washed hands transferred less). The impact of increased contact pressure can also increase the rate of transfer of viruses [39]. Differing microorganism transfer rates from non-porous surfaces to hands suggests that certain surfaces may pose a higher threat than others following a bioterror attack. This is particularly relevant during evacuation, for example, where nonporous metal doorknobs may be necessary to touch in order to exit the building.
Studies into particulate transfer between surfaces and human skin have indicated that the fraction of particles transferred due to direct contact increased when surface roughness decreased and hands were damper. Subsequent presses of a contaminated hand on the same surface showed a reduced transfer rate as the skin surface became loaded with contaminants [40]. The mass transfer of deposited aerosol particles between soft and hard surfaces has been observed to increase with increased surface roughness, and applied pressure [41], while the length of time of contact does not appear to make a difference in the efficiency of particle transfer.
Secondary transfer to environmental surfaces has been examined, with the transfer between fingertips and glass surfaces of viruses being lower than the transfer from surfaces to fingertips [42]. Rhinovirus transfer between the hands of individuals, via a non-porous door knob was shown to be up to 22% [43].
Person-to-person transfer rates: The transfer of microorganisms between individuals through direct contact pathways may occur by through physical contact, and can include shaking or holding hands, kissing, and hugging. Biological agent transferfrom skin to skin has been observed, for example during a handshake. Early studies into infection control demonstrated that pathogens may be transferred between hands in 90% of all handshakes [44]. Rotavirus transfer between contaminated and clean hands has been observed, with the amount transferred decreasing with the amount of time since contamination [45]. In studies of the transfer of Hepatitis A between hands, higher levels of pressure and friction during contact increased the transfer rates [46].
Airborne pathways
Airborne pathways are recognised as being a major source of infection. During an aerosolised bioattack, the risk of infection may be heightened if the occupants are aware of the attack having taken place; adrenaline will make occupants breath more rapidly, potentially increasing the risk of inhaling bioagent. Person-to-person transmission of airborne bioagent through breathing, coughing, or sneezing is unlikely during or immediately following an attack unless the infected individual is heavily exposed, as agents will not have multiplied inside infected hosts, and because the release of bioaerosols from infected individuals tends to be at the maximum only when symptoms begin to appear [47].
Air and contaminant movement: Contaminant movement throughout a building in the air will depend on the airflow network – that is, the doors, windows, ventilation system, the natural permeability of the walls that connect the different zones of the building, and the pressure differentials which dictate the directional flow.
In the absence of information about an attack, no mitigation procedures can be put in place to reduce the dissemination of the agents other than increasing the whole building air dilution, and the spread of the contaminant will proceed based on the typical operation of the building. The opening of doors and windows as individuals move around the building will prove new avenues for air and contaminant movement, depending on the pressure differences between the zones. Localised air movement caused by airflow sources and human activities may cause turbulence effects, which may result in contaminants remaining suspended for longer than they would under still conditions.
Indoor pressurisation systems are often used to direct airflow within a building. For example, zones such as stairwells may be pressurised in order to prevent smoke from entering the stairwell during fire emergencies, and to provide a clear evacuation passage for building occupants. It has been noted both clinically and using modelling techniques that opening doors may cause a transient breakdown in pressure differentials, allowing infectious air to move against a designated pressure gradient [48]. A large-scale building evacuation event may require the doors to the evacuation stairwell to be held open for a long period of time, meaning that pressure differentials may be temporarily lost inside the building zones.
Deposition and reaerosolisation
A number of human factors and behaviours may cause a bioagent to change pathways, through either deposition or reaerosolisation from a surface.
Deposition: Following a bioterror attack on a building, aerosolised agent may be deposited on internal surfaces, furnishings, and individuals within the buildings. Deposition can depend on a number of different factors, including the physical characteristics of the particles and the indoor airflow and building surfaces. Particular surfaces may be at a greater risk of contamination than other due to their hygrothermal properties, surface roughness, and static charge.
Hygrothermal properties and the moisture and thermal properties of a building material can influence the susceptibility of a surface to contamination in a number of ways. Boundary surfaces that are strong conductors of heat, or that are located in thermal bridges, may have cold surface temperatures, and may be susceptible to higher moisture levels. Condensation on cold surfaces may retain dust and particulates from the indoor air, and so may have an increased risk of attracting a bioagent. Temperature differences between a surface and air can cause thermophoretic forces, causing airborne particles to deposit on colder surfaces. Furthermore, temperature and moisture are important factors in the growth and persistence of microorganisms on surfaces, and some surfaces may be more susceptible than others to lingering contamination depending on the bioagent. Horizontal surfaces will accumulate more settled particles due to gravitation fall-out, and so are likely to have a higher level of bioagents. Vertical surfaces will accumulate particles originally suspended in the air and increasing air turbulence and air current velocity will increase the level of surface impaction. Deposition of super-micron particles (> 1μm) onto surfaces appears to increase with particle diameter, surface orientation, and airflow characteristics, while material surface roughness can also lead to a moderate increase in the deposition rate [49]. Particles within the size range of viruses (typically between 0.02 and 0.3μm) been observed to be higher on carpet and curtain than on glass and gypsum [50]. The surface roughness and increased deposition surface area of some textiles indicates that the clothing of individuals may contribute to the amount of agent retained on individuals following an attack. Deposition of particles onto humans appears to depend on a number of variables, including skin moisture, physical movement of the individuals, and hairiness (of, for example, exposed arms) [51].
The electrostatic charge and ionisation of a surface may also impact the level of particle deposition [52]. The process of aerosolising and dispersing bacteria can lead to an electrical charge on the cell wall as high as 13000 elementary electric charges [53]. Electrostatic charges may also impact the rate of attachment to individuals based on their choice of clothing [54] and the static charge carried by the clothing. TV screens have been observed to influence the deposition of submicron particles on humans due to the electrical charge of the device; therefore, individuals sitting close to an object with a high surface voltage, such as a TV screen, may be at higher risk [51]. Charged aerosols also have a higher tendency to form aggregates with other particles and settle to the ground or attach to a charged surface. Weaponisation of anthrax can involve neutralising the Anthrax spores to prolong their air suspension [55].
The ability of different surfaces and materials to experience higher levels of contamination means that certain individuals may require higher levels of decontamination following an aerosol attack. The clothing worn by an individual inside an attacked building may lead to an increased risk of bioagent attachment to the individual due to the natural static charge present in many materials, and coarse fabrics enabling greater attachment to the clothing by the contaminant or vector such as powder.
Secondary Aerosolisation: Bioagents and particulate vectors containing bioagents may be resuspended from surfaces by the activities of individuals following an attack. Resuspension of particulates in the indoor air is recognised as an important factor in indoor air quality [56]. Resuspension can be considered to be the net result of adhesion forces (van der Waals force, electrostatic force, and capillary forces) and resuspension forces (mechanical vibrational, aerodynamic forces, and electrostatic forces) [57].
The relationship between the surface concentration of biological agents and the concentration in the indoor air can be related to the type of surface [58] and the level of disturbance [59]. In addition, aerosolisation of mould species from surfaces in homes has been observed to be related to the air currents, the texture of the surface, and the vibration of the contaminated material [60]. The resuspension of allergens deposited on the ground was studied by Gomes, and was found to be due to disturbances from airflow rather than the mechanical forces of walking [61]. A model of particle resuspension due to walking in indoor environments indicates that shoe bottom roughness, foot size, walking velocity, background velocity, and the velocity of the vertical foot movement can affect particle resuspension rates [62].
Secondary aerosolisation of Anthrax spores was investigated in the aftermath of the attacks on the U.S. Senate Office in 2001. Stationary and personal air samplers were used to measure airborne spores, while surface dust and swab samples were used to measure the surface levels of Anthrax. Under simulated office activities (walking, paper handling, mail sorting), there was a significant increase in the amount of airborne Anthrax spores, of which more than 80% were in an alveolar respirable range of 0.95 to 3.5μm [27]. Spores were spread widely and unevenly throughout the buildings, suggesting that resuspension and tracking can contribute to an agent spread throughout a building. Soft surfaces such as carpets can trap particles, meaning that these particles are less likely to be resuspended compared to hard flooring [63,64].
Bioagents and bioagent-contaminated particles may also be resuspended following deposition on individuals. Particles contaminated by bacteria may be released from contaminated individuals from their clothing [65] and skin [66] during physical activity such as walking. Particle re-suspension from human body sources has been suggested as being a major source of exposure to contaminants in studies of radiopollutants [67]. The potential for bioagentreaerosolisation from contaminated individuals during activity means that removing clothing from individuals during decontamination may pose an additional risk.
Occupant response and contamination spread
Human behaviour plays a key role in the transmission of bioagents and design and success of mitigation strategies after an attack. If an attack is recognised, there are a number of mitigation strategies that can be enacted which can impact the degree of contamination within the building. These measures may include introducing ventilation strategies to reduce the concentration of bioagent in the indoor air, air cleaning strategies, and evacuation or isolation of the building’s population. All these interventions require recognising that an attack has taken place, and the building occupants enacting a plan or system to protect the building occupants. The effectiveness of the mitigation action will depend on its timely implementation, the system effectiveness, and the behaviour of building occupants.
The appropriate ventilation response for a building following an airborne bioterror attack will depend on the design of the ventilation system, including the filtrations systems, dampers, inlet and outlet locations, uncontrolled leakage from the ducts, and the amount of mixing in the system. In many cases, shutting down the ventilation may be the best response to a bioterror attack to prevent spread [5]. Strong airflow may help to keep bioagents suspended in the indoor air, or re-aerosolise them from a surface on which they have deposited due to gravity. Interventions by facility managers to either stop or increase ventilation following an attack will impact dispersion of an airborne bioagent through the building.
There are a number of portable air and surface cleaning technologies that can be activated once the agent has been released into the building environment, for example Ultraviolet Germicidal Irradiation (UVGI) systems and Photocatalytic Oxidation (PCO) Cleaners PCO cleaners. Like with ventilation strategies, their effectiveness will depend on their operation and positioning inside the building, and it is likely that positioning portable air cleaning devices in contaminated areas may put facility managers at unnecessary risk.
The decision to evacuate a building or shelter-in-place will be determined by the emergency plans and protection measures in place. Facility managers may make the decision to evacuate the building, or to shelter-in-place. If the building is evacuated, then mass movement in the building may cause secondary aerosolisation of the deposited agent into the indoor air, while the opening of doors can cause resuspension and open new avenues for contaminant transport through the building. Non-porous doorknobs, push-bars, and ID cards may hold a greater risk of surface to hand transmission of the biological agent to the evacuating individuals. In addition, the close contact between evacuating individuals may result in a higher rate of person-to-person transfer of bioagents. Finally, building occupants may panic during the evacuation, and the more frequent breathing may make increase the risk of respiratory infection.
Alternatively, the order may be given to shelter-in-place. Shelteringin- place will require remaining inside the building in a safe location until the building can be evacuated. The decision to shelter-in-place will also lead to a number of issues, including being isolated in an enclosed environment with potentially limited clean air supplies or inadequate Personal Protective Equipment (PPE). If the attack has been successful, a number of individuals may become contaminated by the bioagent, and they pose a contamination risk to those who have not yet been exposed. Many of the factors that can lead to the spread of infection can be reduced by segregating infected individuals from the presumed uninfected. The segregation and isolation of individuals, who are likely to have become infected raises a number of moral and ethical issues [68]. Healthy individuals presumed to be infected may subsequently become infected when held in quarantine with infected individuals. Contaminated individuals moving between shelter-in-place locations, dispersing bioagent through particle tracking and resuspension, and the behaviour of those held in quarantine, such as attempting to escape, can act to spread the infection further. Finally, as with evacuation, rapid breathing may increase the risk of inhalation of bioagent.
Following a bioattack, exposed individuals will need to be decontaminated and assessed medically. The process of decontaminating individuals following an attack may involve removing contaminated clothing or spraying with a therapeutic agent. Removing clothing may not be a safe solution without respiratory protection due to the potential for reaerosolisation of the contaminant. Electrostatic sprays are available which can form a film over a contaminated surface [69].
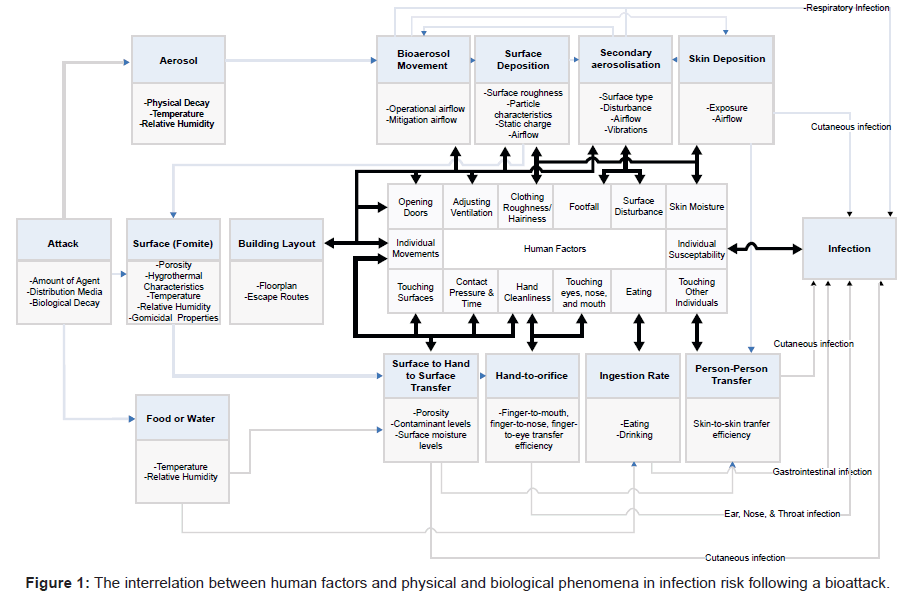
There are a number of conscious or unconscious human factors which may influence the spread of a bioagent through a building following an attack. The interaction between the bioagent resilience of the building and engineering systems, human activity, and the bioagent may all contribute to the dispersal of the agent through different pathways. An initial diagram of the complex relationship between human factors and the spread of infection can be seen in Figure 1.
Modelling contamination and human factors
The nature of contaminant transport and infection risk inside buildings attacked with bioagents is highly complex, with a number of influencing factors. Air and contaminant transport models are widely used to predict the dispersal of biological agents within buildings. These models range from the more simple multinode models, where rooms and their connections throughout the building are considered to more complex and detailed CFD models that provide more detailed predictions of the movement of air inside a well-defined environment. Stochastic formulations of such airflow models allow for users to take into account the uncertainty in the building operation, such as the opening of doors between rooms.
While there has been a great deal of research into the impact of the built environment on the movement of indoor air, there has been less work done to model the impact of human factors on the spread of infection. Models have been developed to describe the resuspension of particles into the indoor air [62,70], and a resuspension module has been developed for the multimode CONTAM contaminant transport program in order to simulate the secondary aerosolisation of particles from walking [71]. A model of environmental transport and human exposure to Category A agents inside an attacked building has been developed which can take into account ventilation rate, agent decay rates, deposition rates, and dose-response functions in order to estimate both fomite and aerosol exposure [72].
Markov chain modelling of infection spread within individuals has been performed by a number of authors using Markov chain models. [22,73,74]. By using environmental pathogen dynamics to calculate infection spread, these studies have been able to predict the spread of an infection throughout a population. Such models can be applied for predicting the spread of infection in a building following a bioterror attack.
One potentially useful tool for evacuation modelling of buildings attacked by bioagents is agent-based models. Agent based models have been combined with CFD models of contaminants to simulate the evacuation of a city following a chemical attack [75], and are widely used to simulate pandemics (e.g. [76]) and building evacuation (e.g. [77]). These models are able to simulate the actions and movements of autonomous agents, and could be used to model individuals within an attacked building. When combined with a contaminant transport model, and dose-response, re-aerosolisation, surface-hand, and person-person transfer data it is possible to model a range of attack and evacuation scenarios. This model would be able to predict those who were exposed to the initial attack, as well as those who are subsequently exposed to infected individuals or surfaces as they leave the building. Such a model would also be able to take into account temporary changes to the airflow network caused by doors opening during the evacuation.
Conclusions
While the spread of bioagents through a building in the indoor air can be modelled using a variety of engineering tools, there is little consideration for how the behaviour of individuals within the building may impact the spread of the agent. This paper has addressed the current understanding of how bioagents may be spread through the indoor environment and between individuals in the immediate aftermath of a bioattack. The interrelation between biological and physical processes, the indoor built environment, and human factors in pathogen transmission is complex. However, understanding how human behaviour inside the building may impact the spread of pathogens can help design buildings and emergency procedures to help minimise casualties and facilitate, 2nd infection control, crime scene inspection and building remediation. Computer modelling methodologies are valuable tools for understanding the impact of different scenarios associated with a bioterror event, and can be developed to take into account the actions and decisions of individuals within a targeted building.
Acknowledgements
The research leading to these results has received funding from the [European Union] [European Atomic Energy Community] Seventh Framework Programme ([FP7/2007- 2013].
[FP7/2007-2011]) under grant agreement n° [242497]. ZN is funded by EPSRC Grant Reference: EP/G029881/1.
References
- Lengel A (2005) Little Progress In FBI Probe of Anthrax Attacks. The Washington Post, Washington, USA.
- Graham B, Talent J, Allison G, Cleveland R, Rademaker S, et al. (2008) World at Risk: Report of the Commission on the Prevention of WMD Proliferation and Terrorism. Commission on the Prevention of WMD Proliferation and Terrorism, New York.
- Kowalski WJ (2002) Immune Building Systems Technology. McGraw-Hill, New York.
- LBNL (2005) Advice for Safeguarding Buildings Against Chemical or Biological Attack. Lawrence Berkeley National Laboratory.
- NIOSH (2002) Guidance for Protecting Building Environments from Airborne Chemical, Biological, or Radiological Attacks. National Institute for Occupational Safety and Health, Cincinnati.
- NIOSH (2003) Guidance for Filtration and Air-Cleaning Systems to Protect Building Environments from Airborne Chemical, Biological, or Radiological Attacks. National Institute for Occupational Safety and Health, Cincinnati.
- Chapman RE, Leng CJ (2004) Cost-Effective Responses to Terrorist Risks in Constructed Facilities’. National Institute of Standards and Technology , National Institute of Standards and Technology, Gaithersburg, MD.
- FEMA (2005) Risk assessment: a how-to guide to mitigate potential terrorist attacks against buildings. Risk Management Series. Federal Emergency Management Agency, Washington DC.
- Thatcher T, Wood EE, Edelson EC, Sextro RG (2005) Simplifying the assessment of building vulnerability to chemical, biological and radiological releases. Lawrence Berkeley National Laboratory, Berkleley, CA.
- Radosavljevic V, Belojevic G (2009) A new model of bioterrorism risk assessment. Biosecur Bioterror 7: 443-451.
- Thompson BP, Bank LC (2010) Use of system dynamics as a decision-making tool in building design and operation. Building and Environment 45: 1006-1015.
- Ezell BC, von Winterfeldt D (2009) Probabilistic risk analysis and bioterrorism risk. Biosecur Bioterror 7: 108-110.
- Agami RT, Jason F (2004) Uncertainty-Based Quantitative Model for Assessing Risks in Existing Buildings. ASHRAE Transactions 110: 217.
- Agami RT, Bahnfleth WP (2007) Requirements for a probabilistic quantitative relative risk-based decision methodology for reducing vulnerability of building occupants to extreme IAQ events. ASHRAE Transactions.
- Zilinskas RA, Hope B, North DW (2004) A discussion of findings and their possible implications from a workshop on bioterrorism threat assessment and risk management. Risk Anal 24: 901-908.
- U.S.D.D. (2007) Unified Facilities Criteria (UFC): DoD Minimum Antiterrorism Standards for Buildings. U.S. Department of Defence, Washington, DC.
- RIDHO (2004) HVAC Building Vulnerability Assessment Tool. Rhode Island Department of Health Office of Occupational & Radiological Health, Providence RI.
- UTRC (2004) CBT-Protection Improvement Design Protocol- Chem/Bio: User’s Guide. United Technologies Research Center, East Hartford, CT.
- Fielding JE, Schunhoff JF, Aguirre A (2006) BAC-Building Assessment Checklist Protection Against Airborne Hazards. County of Los Angeles Public Health, Los Angeles.
- Kowalski W, Bahnfleth W, Musser A (2003) Modeling Immune Building Systems for Bioterrorism Defense. Journal of Architectural Engineering 9: 86-96.
- Wang L, Chen Q (2008) Applications of a Coupled Multizone-CFD Model to Calculate Airflow and Contaminant Dispersion in Built Environments for Emergency Management. HVAC&R Research 14: 925-939.
- Nicas M, Sun G (2006) An integrated model of infection risk in a health-care environment. Risk Anal 26: 1085-1096.
- (2011) Bioterrorism Agents/Diseases. Centers for Disease Control and Prevention.
- Kramer A, Schwebke I, Kampf G (2006) How long do nosocomial pathogens persist on inanimate surfaces? A systematic review. BMC Infect Dis 6: 130.
- (2009) WHO Guidelines for Indoor Air Quality: Dampness and Mould. World Health Organisation, Copenhagen.
- Sinclair R, Boone S, Greenberg D, Keim P, Gerba CP (2008) Persistence of Category A Select Agents in the Environment. 74: 555-563.
- Weis CP, Intrepido AJ, Miller AK, Cowin PG, Durno MA, et al. (2002) Secondary aerosolization of viable Bacillus anthracis spores in a contaminated US Senate Office. JAMA 288: 2853-2858.
- (2011) Anthrax: What You Need To Know. Centers for Disease Control and Prevention.
- (2001) U.S. Army Medical Research Institute of Infectious Diseases. (4thedn) USAMRIID's Medical Management of Biological Casualties, Frederisk, Maryland.
- Weinstein RA (2004) Contamination, Disinfection, and Cross-Colonization: Are Hospital Surfaces Reservoirs for Nosocomial Infection? Clin Infect Dis 39: 1182-1189.
- Wallinga J, Edmunds WJ, Kretzschmar M (1999) Perspective: human contact patterns and the spread of airborne infectious diseases. Trends Microbiol 7: 372-377.
- Hendley JO, Gwaltney JM Jr (1988) Mechanisms of transmission of rhinovirus infections. Epidemiol Rev 10: 243-258.
- Rusin P, Maxwell S, Gerba C (2002) Comparative surface-to-hand and fingertip-to-mouth transfer efficiency of gram-positive bacteria, gram-negative bacteria, and phage. J Appl Microbiol 93: 585-592.
- Boyce JM (2007) Environmental contamination makes an important contribution to hospital infection. J Hosp Infect 65: 50-54.
- Scott E, Bloomfield SF (1990) Investigations of the effectiveness of detergent washing, drying and chemical disinfection on contamination of cleaning cloths. J Appl Bacteriol 68: 279-283.
- Mackintosh CA, Hoffman PN (1984) An extended model for transfer of micro-organisms via the hands: differences between organisms and the effect of alcohol disinfection. J Hyg (Lond) 92: 345-355.
- Sattar SA, Springthorpe S, Mani S, Gallant M, Nair RC, et al. (2001) Transfer of bacteria from fabrics to hands and other fabrics: development and application of a quantitative method using Staphylococcus aureus as a model. J Appl Microbiol 90: 962-970.
- Montville R, Schaffner DW (2003) Inoculum size influences bacterial cross contamination between surfaces. Appl Environ Microbiol 69: 7188-7193.
- Mbithi JN, Springthorpe VS, Boulet JR, Sattar SA (1992) Survival of hepatitis A virus on human hands and its transfer on contact with animate and inanimate surfaces. J Clin Microbiol 30: 757-763.
- Rodes CE, Newsome JR, Vanderpool RW, Antley JT, Lewis RG (2001) Experimental methodologies and preliminary transfer factor data for estimation of dermal exposures to particles. J Expo Anal Environ Epidemiol 11: 123-139.
- McDonagh A, Sextro RG, Byrne MA (2012) Mass transport of deposited particles by surface-to-surface contact. J Hazard Mater 227-228: 370-377.
- Julian TR, Leckie JO, Boehm AB (2010) Virus transfer between fingerpads and fomites. J Appl Microbiol 109: 1868-1874.
- Pancic F, Carpentier DC, Came PE (1980) Role of infectious secretions in the transmission of rhinovirus. J Clin Microbiol 12: 567-571.
- Hall HW, Matthews HM (1926) Transfer of infection by handshakes. Public Health Journal 17: 347-352.
- Ansari SA, Sattar SA, Springthorpe VS, Wells GA, Tostowaryk W (1998) Rotavirus survival on human hands and transfer of infectious virus to animate and nonporous inanimate surfaces. J Clin Microbiol 26: 1513-1518.
- Mbithi JN, Springthorpe VS, Boulet JR, Sattar SA (1992) Survival of hepatitis A virus on human hands and its transfer on contact with animate and inanimate surfaces.J Clin Microbiol 30: 757-763.
- Hall CB, Douglas RG Jr, Geiman JM, Meagher MP (1979) Viral shedding patterns of children with influenza B infection. J Infect Dis 140: 610-613.
- Tang JW, Eames I, Li Y, Taha YA, Wilson P, et al. (2005) Door-opening motion can potentially lead to a transient breakdown in negative-pressure isolation conditions: the importance of vorticity and buoyancy airflows. J Hosp Infect 61: 283-286.
- Lai ACK, Nazaroff WW (2005) Supermicron particle deposition from turbulent chamber flow onto smooth and rough vertical surfaces. Atmospheric Environment 39: 4893-4900.
- Afshari A, Gunnarsen L, Afshari M, Reinhold C (2007) Indoor deposition of fine and ultrafine particles: A full-scale study. Proceedings of Clima 2007, WellBeing Indoors, Helsinki, Finland.
- Andersson KG, Roed J, Byrne MA, Hession H (2006) Deposition of contaminant aerosol on human skin. J Environ Radioact 85: 182-195.
- Lai ACK (2006) Investigation of Electrostatic Forces on Particle Deposition in a Test Chamber. Indoor and Built Environment 15: 179-186.
- Mainelis G, Willeke K, Baron P, Reponen T, Grinshpun SA, et al. (2001) Electrical charges on airborne microorganisms. Journal of Aerosol Science 32: 1087-1110.
- Allen JE, Close JJ, Henshaw DL (2006) Static Electric Fields as a Mediator of Hospital Infection. Indoor and Built Environment 15: 49-52.
- Friedlander AM (2000) Anthrax: clinical features, pathogenesis, and potential biological warfare threat. Curr Clin Top Infect Dis 20: 335-349.
- Thatcher TL, Layton DW (1995) Deposition, resuspensiion, and penetration of particles within a residence. Atmospheric Environment 29: 1487-1497.
- Kim Y, Gidwani A, Wyslouzil BE, Sohn CW (2010) Source term models for fine particle resuspension from indoor surfaces. Building and Environment 45: 1854-1865.
- Buttner MP, Cruz-Perez P, Stetzenbach LD, Garrett PJ, Luedtke AE (2002) Measurement of airborne fungal spore dispersal from three types of flooring materials. Aerobiologia 18: 1-11.
- Price PN, Sohn MD, Lacommare KS, McWilliams JA (2009) Framework for evaluating anthrax risk in buildings. Environ Sci Technol 43: 1783-1787.
- Gorny RL, Reponen T, Grinshpun SA, Willeke K (2001) Source strength of fungal spore aerosolization from moldy building material. Atmospheric Environment 35: 4853-4862.
- Gomes C, Freihaut J, Bahnfleth W (2007) Resuspension of allergen-containing particles under mechanical and aerodynamic disturbances from human walking. Atmospheric Environment 41: 5257-5270.
- Zhang X, Ahmadi G, Qian J, Ferro A (2008) Particle Detachment, Resuspension and Transport Due to Human Walking in Indoor Environments. J Adhes Sci Technol 22: 591-621.
- Braun WX, Cicciarelli BA, Davidson DL, Hart EH, Luedtke A, et al. (2002) Indoor pollutant measurement and modeling: comparing impact of surface characteristic. Indoor Air 2002 - 9th International Conference on Indoor Air Quality and Climate, Monterey, CA, 885-890.
- Willie B (1974) Microbiological hygienic aspects of wall-to-wall carpeting in hospitals. Copenhagen Symposium, Copenhagen 2-37.
- DUGUID JP, WALLACE AT (1948) Air infection with dust liberated from clothing. Lancet 2: 845-849.
- Mackintosh CA, Lidwell OM, Towers AG, Marples RR (1978) The dimensions of skin fragments dispersed into the air during activity. J Hyg (Lond) 81: 471-479.
- Andersson KG, Fogh CL, Byrne MA, Roed J, Goddard AJ, et al. (2002) Radiation Dose Implications of Airborne Contaminant Deposition to Humans. Health Phys 82: 226-232.
- Borrion H, Mitchener-Nissen T, Taylor J, Lai K-M (2012) Countering Bioterrorism: Why smart buildings should have a code of ethics. European Conference in Intelligence Security Informatics, Odense, Denmark.
- Larkin M (2003) Decontamination spray could save lives after bioterrorist attack. Lancet Infect Dis 3: 318.
- Oberoi RC, Choi J-I, Edwards JR, Rosati JA, Thornburg J, et al. (2010) Human-Induced Particle Re-Suspension in a Room. Aerosol Science and Technology 44: 216-229.
- Bramwell L, Howard-Reed C, Dols S, Persily AK, Ferro AR (2009) Using CONTAM with a New Resuspension Module to Estimate Exposures from Human Walking. AAAR 28th Annual Conference: Minneapolis, Minnesota.
- Hong T, Gurian PL, Huang Y, Haas CN (2012) Prioritizing risks and uncertainties from intentional release of selected Category A pathogens. PLoS One 7: e32732.
- Li S, Eisenberg JN, Spicknall IH, Koopman JS (2009) Dynamics and control of infections transmitted from person to person through the environment. Am J Epidemiol 170: 257-265.
- Atkinson MP, Wein LM (2008) Quantifying the routes of transmission for pandemic influenza. Bull Math Biol 70: 820-867.
- Epstein JM, Pankajakshan R, Hammond RA (2011) Combining Computational Fluid Dynamics and Agent-Based Modeling: a new approach to evacuation planning. PLoS One 6: e20139.
- Epstein JM (2009) Modelling to contain pandemics. Nature 460: 687.
- Zheng X, Zhong T, Liu M (2009) Modeling crowd evacuation of a building based on seven methodological approaches. Building and Environment 44: 437-445.
Relevant Topics
- Anthrax Bioterrorism
- Bio surveilliance
- Biodefense
- Biohazards
- Biological Preparedness
- Biological Warfare
- Biological weapons
- Biorisk
- Bioterrorism
- Bioterrorism Agents
- Biothreat Agents
- Disease surveillance
- Emerging infectious disease
- Epidemiology of Breast Cancer
- Information Security
- Mass Prophylaxis
- Nuclear Terrorism
- Probabilistic risk assessment
- United States biological defense program
- Vaccines
Recommended Journals
Article Tools
Article Usage
- Total views: 14949
- [From(publication date):
July-2012 - Nov 27, 2024] - Breakdown by view type
- HTML page views : 10486
- PDF downloads : 4463