Research Article Open Access
HOPE Works: A Community-Based Obesity Intervention Addressing Social Determinants as Underlying Factors
Marci K. Campbell1,5, Salli Benedict2, Ziya Gizlice2, Kristine Kelsey1*, Katie Barnes2,4, Amy Ries1, Brenda DeVellis3 and Barbara Harris4
1Department of Nutrition, Gillings School of Global Public Health and School of Medicine, University of North Carolina at Chapel Hill
2Center for Health Promotion and Disease Prevention, University of North Carolina at Chapel Hill
3Department of Health Behavior and Health Education, University of North Carolina at Chapel Hill
4HOPE Works Community Action Council
5Marci Campbell died 14 December 2011
- *Corresponding Author:
- Kristine Kelsey, PhD
University of North Carolina at Chapel Hill
Department of Nutrition, Gillings School of Global Public Health and School of Medicine, CB #7294, 1700 Martin Luther King Blvd
Chapel Hill, NC 27599, USA
Tel: 336-376-5559
Fax: 919-966-7827
E-mail: kelseyk@email.unc.edu
Received date: March 12, 2012; Accepted date: May 31, 2012; Published date: June 02, 2012
Citation: Campbell MK, Benedict S, Gizlice Z, Kelsey K, Barnes K, et al. (2012) HOPE Works: A Community-Based Obesity Intervention Addressing Social Determinants as Underlying Factors. J Community Med Health Educ 2:154. doi: 10.4172/2161-0711.1000154
Copyright: © 2012 Campbell MK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Objectives: HOPE Works was an innovative, community-based participatory research (CBPR) intervention aimed at addressing health promotion and obesity in the context of social determinants for obese, low-income and minority rural North Carolina women. This study incorporated multiple social health determinants, including hope, which assesses participants’ abilities to set and achieve goals to reach desired health and life changes. Methods: Community Coordinators identified women to serve as HOPE Circle Leaders who received training and recruited women from their social networks. Thirty-four Circles met bi-weekly for 6 months following a manual-based curriculum and received tailored newsletters addressing health and economic literacy. Comparison women were drawn from the same communities. The primary outcome was weight loss. Secondary outcomes were moderate and vigorous physical activity (MVPA), fruit and vegetable (F&V) consumption, and hope. Outcomes were analyzed using the completer cohort and intent-to-treat (ITT), controlling for baseline weight, socioeconomic variables, and Circle cluster effects. Results: A total of 485 women (73% of baseline sample) completed both baseline and follow-up surveys (208 intervention; 277 comparison). Non-completers (117 intervention; 119 comparison) differed by race, employment status, household income, and contribution to household income in the past two years (all p < 0.05). Intervention women lost 4.5 (±1.2) pounds compared to 0.4 (±0.4) pounds for comparison women (p = 0.054 cohort, p = 0.154 ITT); 22.5% and 13.1% of the intervention and comparison groups respectively lost ≥5% of their body weight. Mean (SE) difference in total MVPA between groups was +51.8 (±19.2) minutes/week (p = 0.007), with non-significant improvement in F&V (p = 0.136). Overall hope level did not significantly increase; however, intervention women marginally improved on Agency (goal directed energy) (p = 0.060). Conclusion: Women receiving a community-based weight management program based on addressing social determinants can successfully lose weight. Future, streamlined efforts addressing the needs of women including those unable to participate are important to enhance program reach and public health impact.
Keywords
Women’s health; Health promotion; Health behaviors; Dietary intervention; Physical activity; Disease prevention; Tailored messages; Self-reported health; Positive affect; Coping; Exercise; Obesity; Hope; Social determinants of health; Community based participatory research; CBPR
Introduction
Obesity is one of the most significant public health problems in the United States and leads to increased risk for chronic disease including diabetes, heart disease, musculoskeletal problems, and certain cancers [1,2]. Obesity is more prevalent among women, and minority women are more likely to be obese compared to white women [3]. Although individual-based obesity intervention trials have been efficacious in weight loss [4], there has been relatively little translation to feasible and effective community-based approaches to reach the broader population. Public health experts recognize the need for an ecological approach to addressing determinants of health in community and environmental contexts [5,6]. Socioeconomic status is one of the strongest predictors of health, and determinants such as income, educational attainment, occupation, and neighborhood and community characteristics play a greater role in health than individual behaviors or access to health care [7]. Income disparity, the gap between those at the highest and lowest income levels, also predicts health and is increasing within North Carolina [8-10]. Health promotion interventions that ignore the socioeconomic context and social determinants of the health of populations cannot sustain positive effects, and according to Kaplan and colleagues, “there is growing evidence that the social and economic status of a community has a powerful effect on the health of the residents of that community; therefore, interventions to alleviate health problems such as obesity should address social and economic factors” [11].
We have conducted community-based intervention research with lower-income rural women in eastern North Carolina for nearly 20 years. Over this time we have built relationships with community members and partnered with them on projects focused on social determinants such as workplace health promotion among employed women in blue-collar industries [12,13]; however, widespread plant closings and job loss forced us to consider alternative intervention models. In addition to commonly identified socioeconomic barriers to better health, findings from formative research and input from our Community Action Council (CAC) indicated that a major barrier to health promotion among lower-income rural women was a sense of hopelessness, or lack of empowerment to make positive changes in their lives [9]. The CAC identified obesity as their primary major health promotion issue, but indicated that motivation to make healthy lifestyle changes was hampered by economic stress and lack of job opportunities, inadequate education, and inability to provide opportunities or assets for their children’s future [14].
In the field of positive psychology, the construct of hope offers a different framework for health behavior change, highlighting the ability to envision and achieve goals that will lead to the desired health and life changes. Hope is defined as “a positive motivational state that is based on an interactively derived sense of successful: a) Agency (goal-directed energy); and b) Pathways (planning to meet goals)” [15]. Agency thinking is the motivational component of hope theory, expressed with phrases such as “I won’t give up” [16]. Pathways thinking include the production of alternate routes to a goal, as well as positive selftalk about being able to attain it. Hope has been studied extensively in clinical medicine and psychology; much less has been done in the area of public health [17]. However, there is compelling evidence that agency is positively associated with fruit and vegetable consumption [18], and prior research from our own study communities reveals that higher hope is positively associated with self-reported health and negatively related to BMI [19].
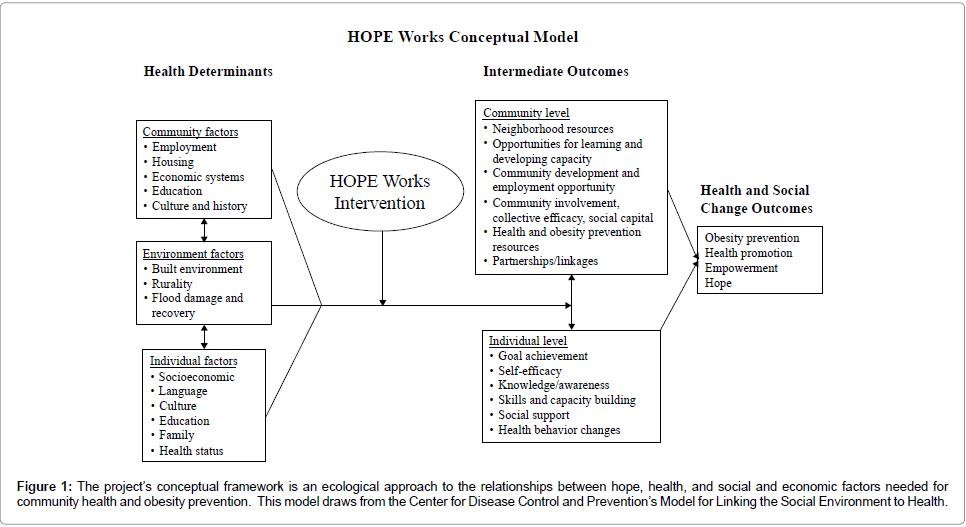
The goal of HOPE (Health, Opportunities, Partnerships, and Empowerment) Works was to develop, implement, and evaluate a community-based health promotion and social and economic empowerment program for overweight and obese, low-income, minority women in two rural counties through a communitybased participatory research (CBPR) approach [20]. The project’s conceptual framework, shown in Figure 1, is an ecological approach to the relationships between hope, health, and social and economic factors needed for community health and obesity prevention. This model draws from the Center for Disease Control and Prevention’s Model for Linking the Social Environment to Health [21]. Important social and environmental factors addressed in the model include civic engagement, community capacity, employment strategies, and opportunities for learning and developing skills.
Figure 1: The project’s conceptual framework is an ecological approach to the relationships between hope, health, and social and economic factors needed for community health and obesity prevention. This model draws from the Center for Disease Control and Prevention’s Model for Linking the Social Environment to Health.
The individual/interpersonal constructs are primarily drawn from Social Cognitive Theory (SCT) [21], Goal Systems Theory [22,23], social support models [24], and hope theory [25]. Important concepts from these theories include self-efficacy (confidence) to make changes, motivation, ability to set and achieve goals, and social support. We hypothesized that through education and skill-building, goal-setting, personalized feedback and reinforcement, and social support for change, women would be better able to improve health behaviors, control weight, improve their socioeconomic situation (e.g., complete a General Educational Development (GED) test to certify high schoollevel academic skills, obtain job training, start a micro-enterprise), and ultimately increase their sense of hope for a better future. Using formative research, we refined and adapted the conceptual model to each of the ethnic groups represented in the study to ensure that the interventions and strategies were culturally appropriate and responsive to community needs. This paper reports the main outcomes of the HOPE Works study.
Methods
Ethics statement
All participants (Circle Leaders (CLs), Circle members, and comparison women) completed a written, informed consent approved by the Committee on the Protection of the Rights of Human Subjects at the University of North Carolina Office of Human Research Ethics.
Study design and recruitment
A randomized controlled design was originally proposed; however, with concerns from our Community Action Council (CAC) that participants, including those in the comparison group, receive some type of intervention, we received approval from our funder, the Centers for Disease Control and Prevention, to switch to a quasiexperimental design. Recruitment for the intervention group occurred in stages. First, we hired four, paid, part-time female community coordinators (CCs), two African American, and one American Indian, and one Latina via subcontract with a community-based organization partner. CCs received recruitment and CL training, and then were asked to identify women from their communities with leadership skills to serve as HOPE CLs. Second, identified CLs received training, and each recruited 8-12 women from her existing social network further HOPE Circle. Overweight women interested in weight management were prioritized, but no one was excluded based on weight status. Women were eligible if they were at least 18 years of age, spoke English or Spanish (all surveys and materials were translated), and were not pregnant.
Comparison women were drawn from the same communities and, to the extent possible, similar social strata. We held community events and advertised via local media (newspaper stories and radio) to recruit comparison women to the study. Women in the comparison group received monthly newsletters on health topics such as back pain, sexually transmitted diseases, and injury prevention.
Women in the intervention group received $10 as an incentive for completion of the follow-up survey. In addition, women in the HOPE Circles received non-monetary gifts such as tote bags, water bottles, and t-shirts printed with the program logo. Comparison women received a $20 incentive to complete the baseline and follow-up surveys. All women received pedometers to help track their physical activity.
HOPE Works intervention
The HOPE Works intervention was delivered by the CLs, who received 22 hours of training that covered the weight management curriculum, leadership and group facilitation skills, and documentation/ record keeping of 70 CLs identified, 36 either did not complete training or did not successfully recruit women for a Circle. Thirty-one CLs completed training for the project over 3½ years of phased study implementation. Most CLs who completed training held one Circle. A total of 34 Circles were implemented between 2005 and 2010. HOPE Circles met at least twice per month for a minimum of 6 months in locations such as churches, community centers, and homes (designated by the participants). CLs kept detailed records of attendance. There was no formal record of Circle quality.
A manual-based curriculum was developed for the CLs, including12 sessions that addressed healthy eating, physical activity, weight control, stress management, education and job skills, goal setting, and micro-enterprise. Community coordinators and members of the CAC contributed to the development of the manual, ensuring that it appropriately addressed the needs of women in the participating communities. The manual was informally pilot tested with the CAC. CLs were trained to follow the content and the order of the topics in the curriculum. Goal setting was an important component of the Circle meetings. After the first meeting, women set one health behavior goal and one life goal related to finances, education, or job skills. These goals were reinforced with discussion about progress and brainstorming ways to overcome barriers to achieving the goals. At each session, women engaged in at least 20 minutes of light to moderate physical activity as a group and had a healthy snack. The first and last Circle sessions included time for survey administration. CCs provided the CLs with ongoing support in partnership with university staff through monthly CL meetings, phone calls, and visits to Circles. CLs supported each other by sharing strategies, tips, successes, and challenges.
In addition to attending the Circles, women received six, computertailored, printed health newsletters delivered once per month by mail to their homes. The newsletters were tailored on variables from each woman’s baseline survey, including health behaviors, psychosocial determinants, and hope-related goals (e.g., education, job). Each newsletter comprised four pages in full color (one 11 x 17 page folded in half), was personalized with the woman’s name, and included behavioral feedback (fruit and vegetable consumption, physical activity, weight), stage of change, and strategies for achieving health and life goals, overcoming barriers, and identifying social support. Each newsletter also provided information about local resources that could be accessed for assistance with the topics addressed in the newsletter. The content of the newsletters reinforced and built upon information provided in the Circle meetings. Community coordinators helped write the tailoring library of messages and provided photographs and testimonials to make the feedback and stories relevant to women of their respective ethnicities and communities.
Study participants completed self-administered paper-and-pencil surveys at baseline (first HOPE Circle meeting) and at 6-month followup. CCs attended the first meeting of each Circle to distribute and collect surveys and answer questions. The community data collector distributed and collected comparison women’s completed baseline and follow-up surveys at various locations and collected data on height and weight.
Measures
Weight was measured at baseline and 6-month follow-up using standardized scales brought to each HOPE Circle meeting site. Height was self-reported. Body mass index (BMI) was calculated using the standard formula of weight in kilograms divided by height in meters squared. BMI categories were defined as: normal (<25), overweight (25-29.9), and obese (30+).
Demographic information included age in years (18-99), years of education (mean 12.6; range 0-20 years), income (categorized as <$20,000, $20,000-$50,000, >$50,000), job status (employed, unemployed, and other, which included students, homemakers and retired women), and race (non-Hispanic white, non-Hispanic black, American Indian, and other).
Moderate and Vigorous Physical Activity (MVPA) was measured using modified physical activity questions from the Behavioral Risk Factor Surveillance System (BRFSS) [26]. Participants were asked whether they did any moderate PA for at least 10 minutes at a time during a usual week. If yes, they were asked about the frequency and duration of their activity. Moderate PA was defined as brisk walking, bicycling, vacuuming, gardening, dancing, light jogging, using a push mower, playing softball, or anything else that causes some increase in breathing or heart rate. Vigorous PA was defined as running, aerobics, and very heavy yard work such as tree removal, swimming, or anything else that causes large increases in breathing or heart rate. Items were modified based on survey pre-testing to provide categorical response options as opposed to open-ended responses. Frequency responses were: 1, 2, 3-4 (=3.5), 5-6 (=5.5) times per week, or every day. Duration responses were asked in minutes or hours: 10-20 minutes (=15), 21- 30 minutes (=25), 31-60 minutes (=45), 1-2 hours (=1.5), more than 2 hours (=2.5). The data were used to create a summary measure of total weekly minutes of moderate and vigorous physical activity. Women also completed the PAR-Q to assess possible health-related contraindications to exercise [27]. Women who checked any items as “yes” were required to get permission from a health care provider before participating in a HOPE Circle.
Fruit and vegetable intake was assessed using the BRFSS questions [26], which include six items about the frequency of consumption of fruit, fruit juices, and four categories of vegetables. Fruit juice was defined as “fruit juices such as orange, grapefruit, or tomato” with a serving size being 6 ounces. These were modified to categorical responses (never, 1-3 times/month=2, 1-2/week=1.5, 3-5/week=4, 1/ day, 2 or more/day). The survey detailed portion sizes. We also asked about total servings of fruit/juice per day and total servings of vegetables per day. The original six items were used to calculate total servings of fruit and vegetables per week and the two summary questions were used to calculate total servings of fruit and vegetables per day.
Hope was measured by the six-item self-report State Hope Scale [25], which includes responses with a range of 1=definitely false to 8=definitely true. Higher scores are indicative of higher levels of hope, and the scale assesses goal-directed thinking at a given moment in time. Sample items include: “There are lots of ways around any problem that I am facing now” (Pathways) and “At the present time, I am energetically pursuing my goals” (Agency). In four studies involving college students, the alpha values for reliability for the overall State Hope scale ranged from .79 to .95. Alphas for the Agency scale varied from .76 to .95 while, for the Pathways subscale, the range was .59 to .93 [28]. Overall, there is strong support for the internal reliability of the scale.
Psychosocial variables:
Health related goals included: eating a healthier diet; increasing physical activity, and working toward a healthier weight. Hope related goals included: getting a better education, owning one’s home, starting a business, improving job skills/finding a better job, and financial security (providing for family, getting out of debt). Stage of change, barriers, social support, information needs, and community resource measures were drawn from previous research [13]. These variables were used to individually tailor the newsletters and are not reported in this paper.
Process measures:
We collected attendance for each HOPE Circle. The HOPE Circle follow-up surveys assessed participants’ recall and perception of various aspects of the Circles and tailored newsletters. For Circles, we assessed level of trust in the accuracy of the information shared by the CL and the degree to which participating in the Circle assisted with changing health behaviors and reaching life goals. For newsletters, personal relevance, level of trust in the accuracy of the information, and degree of assistance in changing health behaviors and reaching life goals were assessed. Women rated their perception of these intervention components using a 4-point response of: 1=None; 2= A little; 3= Some; 4=All or most/A lot.
Statistical analysis
Data were entered using scannable teleform surveys and then imported into SAS Version 9.2 (SAS Institute, Cary, NC) for analysis. Data were checked for outliers and other anomalies. Baseline characteristics (including primary and secondary outcomes) were summarized using descriptive statistics such as means, medians, standard errors, and ranges, and were compared using chi-square tests and t-tests adjusted for clustering within HOPE Circle. Similarly, baseline characteristics were compared between respondents and nonrespondents (dropouts) to determine if they differed systematically on values of non-missing baseline variables. The intervention and comparison groups were not balanced with respect to education, income, weight, race, and job status. Dropout was associated with race, job status, education, and income levels. Analyses of primary (weight loss) and secondary outcomes were conducted using multivariable generalized linear mixed models (GLMM) with identity and logistic link functions for continuous and binary outcome variables, respectively. These GLMMs included HOPE Circles as a random effect, and weight, race, education level, job status, baseline values of outcomes, and study group as fixed effects (covariates) to compare adjusted differences in mean changes in primary and secondary outcomes. Because F&V data were skewed to the right, analyses of statistical significance were conducted using a natural log transformation (1+ ln F&V).All comparisons were made at p = 0.05.
All primary and secondary outcomes were analyzed both under the cohort and intent-to-treat (ITT) principle after imputing missing values of these outcomes. Missing values were imputed using the Markov chain Monte Carlo (MCMC) method and 50 imputed datasets created using SAS multiple imputations procedures [28]. For multiple imputations, minimum and maximum values of continuous variables were specified and values of categorical variables were rounded to the closest categories. These 50 imputed datasets (missing values imputed) were analyzed using the same GLMMs and the results were combined using the SAS PROC MIANALYZE procedure.
Results
A total of 758 participants completed the baseline survey. Women were excluded if they were pregnant (n=9), had surveys with questionable extreme values for key variables (n=5), observed as a CL (n=23), leaving 721 eligible in the baseline sample (n=325 intervention, n=396 comparison). At 6-month follow-up, 523 women completed surveys (73%). Of the 198 women lost to follow-up, reasons were: not attending a minimum of two Circle meetings (n=44), moved and lost contact (n=9), moved outside the intervention counties (n=9), medical reason (n=6), refusing follow-up (n=6), and not able to be reached (n=124). These 198 women were not included in cohort analyses but were accounted for in the ITT analyses. Additionally, participants were dropped from the dataset if they were pregnant at follow-up (n=7), reported extreme weight values, including extreme weight loss post gastric by-pass surgery (n=4), or had become a CL during the study (n=27). This resulted in an analysis sample of 485 participants at follow-up. (n=208 intervention, n=277 comparison).
Baseline comparisons of study arms were made for sociodemographic variables such as age, race, education, job status, income, and BMI. Intervention women were significantly different from comparison women (Table 1), being less likely to be white and more disadvantaged regarding education, job status, and income. Intervention women also had significantly higher BMI at baseline. Non-completers (117 intervention; 119 comparison), or approximately 32.7% of the 721 in the baseline sample were predominantly nonwhite, unemployed, had a household income less than $50,000, and no increase in percent contribution to their household income in the past 2 years (all p<0.05). All analyses for primary and secondary outcomes were adjusted for race, education level, and job status. Each outcome was adjusted for its baseline value. We present results for the study completer cohort, as well as the ITT analysis, including all eligible baseline participants.
| Variable | Intervention (n=325) Mean (SE)/% (#) | Comparison (n=396) Mean (SE)/% (#) | p-valuea |
|---|---|---|---|
| Age | 47.1(0.70) | 46.8(0.87) | 0.79 |
| Race/ethnicity | <0.001 | ||
| Black | 68% (220) | 64% (254) | |
| American Indian/ Other | 15% (49) | 8% (31) | |
| Education | 12.6 (0.15) | 14.3 (0.12) | <0.001 |
| Job status | <0.001 | ||
| Employed | 55% (180) | 72% (284) | |
| Unemployed | 15% (49) | 8% (33) | |
| Other | 30% (96) | 20% (79) | |
| Incomeb | <0.001 | ||
| <$20,000 | 46% (143) | 29% (109) | |
| $20,000-$50,000 | 44% (139) | 40% (149) | |
| ≥50,000 | 10% (32) | 32% (119) | |
| Weight (pounds) | 199 (3.17) | 192 (2.65) | 0.09 |
| Body Mass Index | 34.1 (0.52) | 32.6 (0.43) | 0.02 |
Table 1: Intervention and comparison group demographic and health characteristics at baseline (N=721) for the HOPE Works study in rural, eastern North Carolina, 2004-2009.
Primary outcome
Weight loss at 6 months:Women in the intervention group lost an average of 4.5 pounds (p<0.0001), versus comparison women who lost 0.4 pounds (p=0.51, Table 2). Cohort analyses adjusted for baseline values, covariates, and Circle cluster effects showed that intervention group participants lost an adjusted average of 2.83 more pounds than comparison group participants (p = 0.054) (Table 3). The effect, however, was not significant using the ITT analysis (setting all follow up non-respondent values to their baseline weight (p = 0.145)). Women in the intervention group decreased their BMI by an average of 0.74 and women in the comparison group decreased their BMI by an average of 0.04 (Table 2). The cohort analysis showed that intervention women decreased their BMI 0.51 units more than women in the comparison group, p = 0.056, however the ITT p-value was 0.145.
| Variable1 | Intervention (N=208) | Comparison (N=277) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | Change | Baseline | Follow-up | Change | ||||||
| Weight (lbs) | 204 (6.6) | 200 (6.1) | -4.46 (1.2) | 189 (3.2) | 189 (3.1) | -0.42 (0.4) | |||||
| BMI | 34.9 (1.1) | 34.1 (1.0) | -0.74 (0.2) | 32.2 (0.5) | 32.2 (0.5) | -0.04 (0.1) | |||||
| Physical activity | 149 (18.3) | 174 (17.4) | +25.4 (21.2) | 154 (14.0) | 122 (10.5) | -31.6 (14.2) | |||||
| Fruits & vegetables | 14.3 (0.6) | 16.5 (0.6) | +2.25 (0.5) | 16.1 (0.7) | 16.0 (0.6) | -0.11 (0.5) | |||||
| Hope | 35.6 (0.5) | 37.5 (0.6) | +1.86 (0.6) | 37.1 (0.4) | 37.9 (0.4) | +0.85 (0.4) | |||||
fruits and vegetables per week
Table 2: Baseline, follow-up, and crude change scores and standard errors (SE) for the primary and secondary outcomes of weight, physical activity, fruit and vegetable intake, and hope for intervention and comparison group participants in the HOPE Works intervention for women in rural, eastern North Carolina, 2004-2009.
| Variable | Mean difference between study groups (Cohort) | SE | Cohort p-value a | ITT p-value b |
|---|---|---|---|---|
| Weight (pounds) | -2.83 | 1.46 | 0.054 | 0.145 |
| BMI | -0.51 | 0.27 | 0.056 | 0.145 |
| Physical activity | 51.8 | 19.2 | 0.007 | 0.057 |
| Fruits & vegetables | 0.09 | 0.06 | 0.136 | 0.090 |
| Hope | 0.94 | 0.59 | 0.113 | 0.165 |
values of outcomes, and study group as covariates.
bITT analysis included data on all participants enrolled after imputing missing values of outcomes using Markov chain Monte Carlo method
Table 3: Results from the multivariate analysis of primary and secondary outcomes of weight, physical activity, fruit and vegetable intake, and hope for the HOPE Works intervention for women in rural, eastern North Carolina, 2004-2009.
In a subsequent analysis, we examined the proportion of women in the intervention and control groups who lost 5% or more of their body weight at 6 months. We found that 22.5% of the intervention group and 13.1% of the comparison group lost 5% or more of their body weight (p = 0.008) (data not shown). After adjusting for baseline weight, baseline educational attainment, educational attainment, race, and job status (using a GLMM with logistic link function), the predicted probabilities of at least 5% weight loss was 19% for the intervention and 13% for the comparison groups respectively (p = 0.107) (data not shown).
Secondary outcomes
Physical activity: Intervention women increased physical activity (MVPA) 25 minutes per week, compared to a decrease of 32 minutes per week for comparison women (Table 2).After adjustment, women in the intervention group reportedly exercised 52 more minutes per week than women in the comparison group (p = 0.007 and ITT p = 0.057) (Table 3). Because physical activity data were not normally distributed, we employed a square root transformation for further analysis. After adjusting for baseline total PA, baseline weight, educational attainment, race and job status, we found a significant difference in mean change between the intervention and comparison women (11.0 vs. 8.7 square root minutes/week; p = 0.002).
Fruit & vegetable consumption: Women in the intervention group increased their F&V intake by 2.25 servings per week on average, while women in the comparison group had an average reduction of 0.11 servings (Table 2). After adjustment for covariates and baseline intake, the effect was not statistically significant. The log-transformed difference in mean change of total servings of fruits and vegetables per week was 0.1 log servings/week (p = 0.13) (Table 3). Additional analyses of F&V intake using the two summary questions (total fruit juice/day and total vegetables/day) showed that, on average, intervention group participants increased daily fruit and vegetable consumption 0.22 servings more than comparison group participants (cohort p = 0.32, ITT p = 0.09) (data not shown).
Hope scale: After adjusting for baseline hope values, baseline weight, educational attainment, race and job status, the difference in mean change in the overall Hope scale between comparison (37.3 unit) and intervention (38.3 unit) women was 0.94 units (p = 0.11) for the cohort sample. The ITT p-value was 0.165 (Table 3). The change in the pathway sub-scale was not significantly different between arms (p = 0.39); however, the difference in the Agency subscale was greater (p = 0.07), suggesting a marginal association between motivation and sense of ability to change and weight.
Process evaluation measures
The process measures collected from intervention participants showed that the majority of women (77%) reported high trust in the accuracy of information provided by CLs. Women reported that HOPE Circles helped them change health behaviors (40% a lot and 40% some) and reach life goals (29% a lot and 45% some). Participants also had largely favorable perceptions of newsletters, primarily because they: felt that all, most, or some of the newsletter was written especially for them (78%); trusted a lot in the accuracy of the newsletter (66%), or felt the information in the newsletters somewhat helped them change their behaviors. Additionally, in response to an open-ended question about what women liked best about being in a Hope Circle, women most often referred to the support and fellowship of other Circle members to help them set and reach goals.
Discussion
The results of this study suggest that using an innovative CBPR approach to obesity reduction can be effective for low-income rural women who successfully participate. By partnering with the CAC and community organizations, we designed the HOPE Circle concept of addressing both social determinants and health promotion within one intervention model.
Women in HOPE Circles lost more weight than comparison women. Weight loss in the intervention group was statistically significant in the cohort analysis. However, multiple baseline differences between the two groups, likely resulting from differences in recruitment rather than randomization of Circles, coupled with 27% loss to follow-up and relatively high standard errors, may explain the non-significant statistical difference in the ITT analysis. Despite the ITT analyses, the cohort analyses suggest that those who successfully completed the intervention were able to lose weight. These results are similar to findings from other community-based and communitybased participatory research interventions [29,30]. Furthermore, as the subsequent analysis of weight loss at 6 months indicated, 23% of women in the intervention group lost 5% or more of their body weight, indicating promise for such an intervention in this population.
We saw improvements in both MVPA and F&V, particularly for MVPA. This improvement in physical activity further validates the measured weight loss among intervention women. It is likely that the group effect of exercising together in the Circles and also getting together for exercise outside of Circles helped women to increase their activity. Some Circles started walking groups, and one group walked two miles during each Circle meeting. The wrap-up celebration for the project was a 4 kilometer Fun Walk and Health Fair.
It was surprising that we did not see more differential change in the Hope scale. The comparison women started with higher hope scores, which might be expected given that they were less heavy and had relatively higher socioeconomic status. We demonstrated in previous research that a higher sense of hope is associated with education and income, and inversely associated with obesity level [19]. The trend towards greater improvement in the Agency sub-scale suggests that the intervention may have helped women increase their motivation and confidence to set and achieve goals, which is encouraging in such a brief intervention. At baseline, many women expressed difficulty setting goals because they were not used to thinking about or prioritizing their future plans. The lack of differential change in the Pathways subscale suggests that more needs to be done to help women find the “waypower” (resources, funds, access) to go from motivation and willpower to goal fulfillment. However, the challenges these women faced were not surprising. Literature on women with multi caregiver roles (i.e., multiple responsibilities to family and friends) indicates a need for support systems they can rely on to help them meet their daily responsibilities so they can make time for improving their health [31]. Future research should incorporate more emphasis on helping women find resources and information to improve credit, get a loan, save money, get a better job, and other aspects of moving out of poverty and improving health. In addition, changes to the built environment were not addressed in this study, but many of the communities did not have exercise facilities or a supermarket at a reasonable distance from home. Future projects might focus on ways to improve access to these types of resources, so that the healthy choice is an easier choice.
The challenges the women faced who successfully participated in the study may have been even more evident for those who were noncompleters. Of the 721 women at baseline, one-third dropped out, and they were more likely to be non-white and have low socioeconomic status. It is very likely that these factors were even more challenging for them than those who successfully completed the study. Such findings further substantiate the inherent burden of adverse social determinants and the even greater importance of identifying ways to engage this hard-to-reach group so that they can participate and potentially benefit from what the Circles offer.
This study had some limitations, including the relatively short 6-month follow-up period, whereas weight loss and changes in factors such as hope may take longer to achieve. We relied on self-report data for health behaviors, hope and height, although weight was measured by the study team. The study was not a randomized controlled trial, which, although desirable, was not feasible or acceptable to the community in this study. Although we adjusted for study arm differences in statistical analyses, it is likely that these may have affected our ability to detect outcomes. In addition, we had difficulty obtaining follow-up data from some women, despite concerted efforts by the CCs and community data collector. Women moved or changed contact information without informing us, and many disliked having to complete surveys, although we knew anecdotally from the CLs that some had made large changes and lost weight. Thus, use of the ITT analysis may have underestimated the study effects.
In conclusion, the HOPE Works study demonstrated that an innovative model of addressing social and economic issues along with health promotion can result in significant changes in physical activity and modest changes in weight. Although we failed to find a significant improvement in hope, we believe that longer-lasting interventions and more emphasis on pathways to change, such as resources and structural/ environmental supports, may achieve those results. Currently, our team is implementing the intervention for6 months with an option for continuing another 6 months as a reinforcement and maintenance phase. We are also working through community organizations to mobilize more environmental and structural support for behavior change, as well as create more opportunity for sustainability and dissemination of the intervention over time. In addition, in a different study we are testing the effect of adding an assets-building component to the HOPE Circle intervention using individual development accounts (IDAs) with matched savings. The results of these studies may help to inform future efforts to improve intervention and policy research and practice for women’s health promotion.
Acknowledgements
This research was funded by the Centers for Disease Control and Prevention Cooperative Agreement Number U48000059 to the University of North Carolina’s Prevention Research Center. Special thanks to the Community Action Council members, Community Coordinators A. Imani Rivera, Patricia Peterson, and Tabatha Brewer, and community organization partners Sharon Brown-Singleton (Commwell Health, Newton Grove, NC), Elizabeth Maynor (CoharieIntraTribal Council, Clinton, NC), and Anne Doolen (Multicultural Business Association, Roseboro, NC). Many thanks and much appreciation to Dr. Marci Campbell, the Principal Investigator for this project, who died on December 14, 2011. She made a positive impact on the lives of many people through her work on this and countless other innovative research projects.
References
- Centers for Disease Control and Prevention (2011) U.S. Obesity Trends. Atlanta, GA
- Must A, Spadano J, Coakley EH, Field AE, Colditz G, et al. (1999) The disease burden associated with overweight and obesity. JAMA 282: 1523-1529.
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, et al. (2006) Prevalence of overweight and obesity in the United States, 1999-2004. JAMA 295: 1549-1555.
- Heshka S, Anderson JW, Atkinson RL, Greenway FL, Hill JO, et al. (2003) Weight loss with self-help compared with a structured commercial program: a randomized trial. JAMA 289: 1792-1798.
- Muller MJ, Mast M, Asbeck I, Langnase K, Grund A (2001) Prevention of obesity--is it possible? Obes Rev 2: 15-28.
- Koplan JP, Fleming DW (2000) Current and future public health challenges. JAMA 284: 1696-1698.
- Marmot M (2005) Social determinants of health inequalities. Lancet 365: 1099-1104.
- Centers for Disease Control and Prevention (Public health puzzle: social determinants of health) 2002. Chronic Disease Notes and Reports 15: 1-9.
- Syme SL (1998) Social and economic disparities in health: thoughts about intervention. Milbank Q 76: 493-505, 306-307.
- Analysis BoE (2002) Bureau of Economic Analysis.
- Kaplan RM (2000) Two pathways to prevention. American psychologist 55: 382-396.
- Campbell MK, Tessaro I, DeVellis B, Benedict S, Kelsey K, et al. (2000) Tailoring and targeting a worksite health promotion program to address multiple health behaviors among blue-collar women. Am J Health Promot 14: 306-313.
- Campbell MK, Tessaro I, DeVellis B, Benedict S, Kelsey K, et al. (2002) Effects of a tailored health promotion program for female blue-collar workers: health works for women. Prev Med 34: 313-323.
- Benedict S, Campbell M, Doolen A, Rivera I, Negussie T, et al. (2007) Seeds of HOPE: a model for addressing social and economic determinants of health in a women's obesity prevention project in two rural communities. J Womens Health (Larchmt) 16: 1117-1124.
- Lopez SJ, Snyder CR, Teramoto Pedtrotti J (2003) Hope, cognitions, and emotions. In: Lopez SJ, Snyder CR (eds) Positive Psychological Assessment: A Handbook of Models and Measures, American Psychological Association, Washington D.C.: 94-107.
- Snyder CR, LaPointe AB, Crowson Jr. JJ, Early S (1998) Preferences of high- and low-hope people for self-referential input. Cognition & Motion 12: 807-828.
- Coughlin SS (2006) Hope, ethics, and public health. J Epidemiol Community Health 60: 826-827.
- Nollen N, Befort C, Pulvers K, James AS, Kaur H, et al. (2008) Demographic and psychosocial factors associated with increased fruit and vegetable consumption among smokers in public housing enrolled in a randomized trial. Health Psychol 27: S252-259.
- Kelsey KS, DeVellis BM, Gizlice Z, Ries A, Barnes K, et al. (2011) Obesity, hope, and health: findings from the HOPE Works community survey. Journal of community health 36: 919-924.
- Centers for Disease Control and Prevention (2011) Community Partnership. Atlanta, GA
- Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE, Task Force on Community Preventive Services (2003) The Community Guide's model for linking the social environment to health. Am J Prev Med 24: 12-20.
- Locke EA, Latham GP (2002) Building a practically useful theory of goal setting and task motivation. A 35-year odyssey. Am Psychol 57: 705-717.
- Strecher VJ, Seijts GH, Kok GJ, Latham GP, Glasgow R, et al. (1995) Goal setting as a strategy for health behavior change. Health Educ Q 22: 190-200.
- Silverberg DS, Baltuch L, Hermoni Y, Eyal P (1985) A national programme of hypertension control using a doctor-nurse team approach: the Israel experience. J Hypertens Suppl 3: S453-S455.
- Snyder C, Irving L, Anderson J (1991) Hope and health: measuring the will and the ways. In: Snyder C, Forsyth D (eds) Handbook of Social and Clinical Psychology: The Health Perspective, Pergamon Press, Elmsford, NY, pp 285-305.
- Centers for Disease Control and Prevention (2003) Behavioral Risk Factor Surveillance System Survey Questionnaire. Atlanta, GA
- Shephard RJ (1994) Readiness for physical activity. PCPFS Research Digest: 1-9.
- Little R, Rubin D (1997) Statistical Analysis with Missing Data, John Wiley and Sons, Inc., New York.
- Mau MK, Keawe’aimoku Kaholokula J, West MR, Leake A, Efird JT, et al. (2010) Translating diabetes prevention into native Hawaiian and Pacific Islander commuities: the PILI ‘Ohana Pilot poject. Prog Community Health Partnersh 4: 7-16.
- Bezzano AT, Zeldin AS, Diab IR, Garro NM, Allevato NA, et al. (2009) The Healthy Lifestyle Change Program: a pilot of a community-based health promotion intervention for adults with developmental disabilities. Am J Prev Med 37: S201-S208.
- Carter-Edwards L, Skelly AH, Cagle CS, Appel SJ (2004) "They care but don't understand": family support of African American women with type 2 diabetes. Diabetes Educ 30: 493-501.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 15403
- [From(publication date):
June-2012 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 10837
- PDF downloads : 4566