Research Article Open Access
Health Seeking Behaviours of Women with Cervical Cancer
Gayle Langley1 and Nonhlanhla Mary2*1University of Witwatersrand, South Africa
2Nursing University of Witwatersrand, South Africa
- *Corresponding Author:
- Nonhlanhla Mary-Immaculate Nkabinde
M.Sc Nursing University of Witwatersrand
P.O.Box 8849, Newcastle 2940, South Africa
Tel: (076) 569-3985/(034) 312-2378
Fax: (034) 312-2378
E-mail: nhlanhla200@yahoo.com
Received date: September 17, 2012; Accepted date: September 22, 2012; Published date: September 24, 2012
Citation: Langley G, Mary N (2012) Health Seeking Behaviours of Women with Cervical Cancer. J Community Med Health Educ 2:170. doi: 10.4172/2161-0711.1000170
Copyright: © 2012 Langley G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Background: Cervical cancer is the most common cancer in South Africa among Black women. It is one of the few cancers where screening can identify pre-cancerous lesions and where the association between screening and mortality decline has been demonstrated.
Objectives: An exploratory, descriptive survey was conducted at a Radiation Oncology Outpatient Department of a large academic hospital in Gauteng. The aim was to explore and describe the action patients had taken when they noticed symptoms, which they consulted, how many health care providers they saw before the diagnosis, their awareness of the Pap smear, the stage of the disease they presented with and to identify their predisposing factors.
Method: A systemic random sample was used to select patients who were returning for follow-up consultation after they had been diagnosed and treated for cancer of the cervix. Data were obtained using a questionnaire and were analysed by means of descriptive statistics.
Results and conclusion: Most of the participants were diagnosed at advanced stages of cervical cancer, 54% (n=65) at stage 2b and 22% (n=26) at stage 3b of cervical cancer Most went to a clinical facility when they noticed symptoms: 45% (n=55) to a hospital and 42% (n=52) to a clinic. Almost half of the respondents: 49% (n=57), did not know what caused the symptoms, a similar number (n=57) took some time to consult a clinician after noticing symptoms and 53 (n=60) knew what a Pap-smear was but had only had it done when they became ill. The study revealed that women’s general knowledge of cancer of the cervix is very poor. It was apparent that the health care facilities are effective in performing Pap smears as the majority of the participants saw only two health care providers before the diagnosis was made.
Keywords
Cervical cancer; Invasive cancer; Pap smear; Women
Introduction
Cancer is a serious illness most often characterized by remissions and relapses and often requires extensive and debilitating treatments. Cancer continues to take a heavy toll despite intensive research and aggressive treatment [1]. Cervical cancer is the most common cancer in South Africa among Black women and is one of the few cancers where screening can identify pre-cancerous lesions and where the association between screening and mortality decline has been demonstrated by Fonn et al. [2].
Fonn et al. [2] investigated the prevalence of pre-cancerous lesions and cervical cancer in South Africa. A sample of 20 603 women participated in this study. It was found that 468 (2.42%) of the women screened were found to have low-grade squamous intra-epithelial lesions (LSIL); the average age of these women was 33.1 years. Three hundred and sixty-six (1.8%) had high-grade SIL (HSLI) and these women were statistically significantly older at 37.97% years of age. Ninety two women (0.47%) were found to have invasive cancer on cytological diagnosis. These women were significantly older, with an average age of 51.3 years. A clear relationship was found between age and LSIL, with younger women having a high rate of LSIL, which decreases with increasing age. A similar but inverse relationship between age and invasive cancer was described with the rate being low in young women and increasing with the increasing age (Ibid: 55). In Sub-Saharan Africa, the association between HIV seropositivity with resulting immunosuppression and abnormal Pap smear results is significant [3]. www.cancer.org/Cancer/CervicalCancer, [4] and the need to screen for cervical lesions is, consequently, important.
Literature Review
The development of cancer of the cervix
Cancer of the cervix is a culmination of a progressive disease that begins as a neoplastic alteration of the squamo-columnar junction. Over time, these abnormal cells can progress to involve the full thickness of the epithelium and invade the stromal tissue of the cervix. The initial preinvasive or premalignant changes are called cervical intraepithelial neoplasm (CIN). Once the disease progresses beyond the basement membrane and invades the cervical stroma, the disease is considered to be invasive and malignant [5].
Predisposing factors of cervical cancer
Squamous cell carcinoma of the cervix and its intraepithelial precursor follow a pattern typical of sexually transmitted disease. The most important risk factor being infection by the human papilloma virus (HPV), particularly HP types 16 to 18 - about two thirds of all cervical cancers are caused by HPV types 16 and 18. (www.cancer.org/ CervicalCancer) [4].
The risk of cervical cancer is increased in sex workers and in women who have first coitus at a younger age, those who have multiple sexual partners, have sexually transmitted diseases, or bear children at a younger age. Promiscuous sexual behaviour in male partners is also a risk and some research suggests that women with partners who have been circumcised are less likely to get cervical cancer [6]. Other factors that may be associated with cervical cancer include cigarette smoking, immunodeficiency, vitamin A or C deficiency and oral contraceptive use [7].
High parity is a significant predisposing factor for cervical cancer. Results of a few case-control studies of cervical carcinoma confirmed an independent role for high parity. After allowance for several indicators of sexual habits, the risk of cervical cancer was increased by more than two-fold in women who had four children or more compared with those who had one or none [8]. Women in developing countries have a higher risk [6]. It is rare in women who have not been exposed to risk factors, for example: virgins, nuns, Jewish and Arabic women.
Signs and symptoms of cervical cancer
Early signs and symptoms of cervical cancer are: abnormal vaginal bleeding, which could be intermenstrual, postmenstrual, and/or postmenopausal watery and offensive discharge. Late signs are pain, pain during intercourse, frequency of micturition, haematuria, fistula formation, anaemia and cachexia and bone pain due to metastasis [9].
The symptoms of cancer of the cervix only begin when the surface of the growth becomes ulcerated; hence they appear later with endocervical growths. The chief symptom is a watery, offensive and blood-stained discharge, or bleeding – particularly after coitus [10].
Treatment of cervical cancer
Cervical cancer is mainly treated by surgery and radiation. Cassidy et al. [11] explain the treatment as follows: When the disease is localized to the ectocervix (CIN 3), surgery recommended includes colposcopy, loop diathermy, cryoprobe or laser, and when the disease has extended to the endocervical canal or microinvasion cone biopsy is recommended. Surgery recommended for invasive carcinoma less than 4 cm, confined to the cervix, is Wertheim’s hysterectomy which removes parametrium and pelvic nodes.
The radiotherapy given is external beam radiation followed by intra-cavitary brachytherapy over a period of four to six weeks. Chemotherapy has no established role in the radical treatment of this cancer, despite a considerable number of studies. Patients with recurrent pelvic or systemic metastatic disease may benefit from palliative chemotherapy.
Traditional means of treating illness and cervical cancer
Many African people of all social groups and educational levels consult both Western and traditional health care providers concurrently. Natural and supernatural exist in the African context and both health care systems are consulted to clarify the ‘how’, ‘where’, ‘when’, and ‘why’ of illness as the belief is that an illness is always caused by something. Consulting a traditional health care provider clarifies especially the ‘why’ and ‘who’ of an illness [12]. Steyn and Muller [13] explain that traditional treatment used for females with cervical cancer includes a mixture of mpambani (a blue stone) and water which is applied to the sore (tumour) by cotton wool, steaming with medicine while the patient is covered in a blanket, mixing ‘muti’ (medicine) called ‘lekoni sekgala’ forming it into a ball and inserting it into the vagina and the use of systemic medicine to stop vaginal bleeding.
Research Method and Methodology
Research design
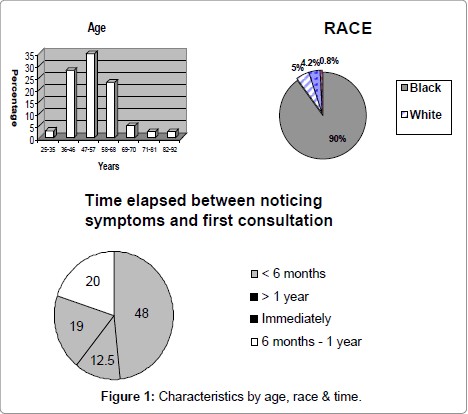
An exploratory, descriptive survey was used to obtain information from a sample of women who were returning for consultation following treatment for cancer of the cervix (Figure 1).
Research setting
The site was the specialist Radiation Oncology Outpatient Department of a large level 3 academic hospital in Johannesburg. Approximately 600 new cases of patients presenting with cancer of the cervix are seen every year for diagnosis and treatment. Patients are referred by gynaecologists or general practitioners from other secondary and tertiary hospitals and from other provinces in South Africa, particularly Limpopo, Mpumalanga and KwaZulu-Natal. Once treatment is completed they are referred back to their referral hospital, and come back for follow-up assessment and treatment annually. Approximately thirty to forty follow-up patients are seen every Tuesday; these patients were included in this research.
Population
The population in this study comprised of all the patients who were diagnosed and treated for cancer of the cervix and were returning for their scheduled annual follow up appointments. Approximately 30 to 40 patients are seen every week: therefore the expected population over the period of three months was 480.
Sample selection
Systemic random sampling was used in order to randomly capture respondents over the period of three months to achieve a sample of 120 participants. The register of patients returning for follow up was used as a sampling frame and every 4th patient presenting for followup consultation was included invited to participate. Ten patients per week were asked to participate and, if they were willing to volunteer, informed consent was obtained.
Data collection
The instrument: The questionnaire was divided into three sections. Section A elicited the respondents’ demographic data, Section B elicited their signs and symptoms, whom they consulted when they noticed symptoms, if they were referred to someone else, how many health care providers were seen before the diagnosis of cancer was made, how long after the first symptom the person went for consultation, what made them go for the first consultation. Their usual means of transport to the academic hospital was also elicited. Section C elicited the participants’ exposure to predisposing factors of cervical cancer and their awareness of the Pap smear as a screening and preventative measure for cervical cancer. Because these questions were sensitive and personal, they were placed at the end of the questionnaire in order to allow participants time to establish rapport. Close-ended questions were used. The researcher was available to administer the questionnaire herself should the participants wish and remained with patients to assist with problems of literacy or to clarify concepts where required.
Results
Demographics
Forty three of the one hundred and twenty participants (35%) were in the age range of 47-57 years. Black Africans comprised the majority (90%; n=108), 49% (n=59) had a primary school education, most were unemployed 63% (n=76) and were receiving an income of R500-R999 (51% n=61). Many grew up in the township 43% (n=51), and most indicated that they were living in houses 71% (n=85).
Signs and symptoms initially experienced
Respondents presented with post-coital bleeding, lower abdominal pain, postmenopausal bleeding, dyspanuria, intermenstual bleeding, foul smelling and watery per vaginal discharge and lower backache. The majority 48% (n=57) did not know what caused the symptoms.
Forty five percent (n=54) went to a hospital and 42% (n=52) consulted a clinic when they noticed symptoms. Eighty two percent (n=98) of the sample consulted because the symptoms increased; 48% (n=58) took less than six months to consult when they noticed symptoms.
Sixty percent (n=72) of the sample were referred to another hospital after their first consultation, 38% (n=46) saw two health care providers before the diagnosis of cancer of the cervix was made. The majority of the sample 73% (n=90) use public transport to get to and from the academic hospital.
Predisposing factors
Almost half of the sample (49%; n=59) never used tobacco. Forty three percent (n=52) stated that they had had their first sexual experience between the ages of 17 and 23 years. Forty three percent (n=40) had their first sexual experience between the ages of 12 to 16 years, 55% between 17 and 23 years. Forty five of the participants had been pregnant for the first time at a young age; 45% (n=55) between the ages of 14-18 years. Most were multi-parous – 70% (n=84) had been pregnant from 1-5 times and 68% (n=82) of the sample had had 1-5 babies (Table 1).
The majority 80% (n=96) of the sample did not have a family history of cancer of the cervix, thirty percent (n=36) of the sample had 1-5 sexual partners. The majority 57% (n=68) had never suffered from sexually transmitted infections. Forty nine percent (n=59) knew about the Pap smear, but they had never done it before it was only done when they became ill. The majority 54% (n=65) presented with stage 2b of the disease followed by stage 3b 22% (n=26) (Table 2).
Limitations
The limitations of the study were:
• The question regarding the parity of the respondents in section C of the questionnaire was not sufficiently specific. The question asked how many times they had been pregnant. The majority of the participants were pregnant one to five times, which could have been once or five times, and this does not specify multiparity or null parity. The question regarding the number of babies the respondents had was also not sufficiently specific.
• Nothing was asked or mentioned about the sample’s HIV status, yet it is a major predisposing factor of the disease with the incidence steadily increasing. Ethical considerations precluded the researcher from ascertaining or asking respondents about their HIV status. It has been proposed that the reason AIDS is spreading at such frightening rate in South Africa and elsewhere is primarily due to men’s sexual behaviour – in particular their common preference for sexual experiences with many different partners, their unaccountability to female partners and their domination of women in sexual interactions [14].
• The question regarding accessibility of health care facilities was another limitation because patients were asked how they travel to the large academic hospital in Gauteng, which was the research setting. However, most of them had been referred from other hospitals for treatment. Instead one could have asked about accessibility of the health care facilities when they first consulted.
• The respondents were presenting at the research setting for scheduled annual follow-up care after they had received treatment years ago. It could have been noted when they received treatment in order to elicit how long they had been in remission so as to note the survival rate. This is important in order to ascertain the effectiveness of treatment for cancer of the cervix and was a notable limitation of this study.
Recommendations
The recommendations for this study will be discussed under three headings –that is, for nursing practice, nursing education and nursing research.
Nursing practice
It is recommended that health education should be given to women about the disease. The health education campaigns can be held at places like antenatal clinics, well baby clinics, family planning clinics and sexually transmitted infections clinics because these are the places where women gather. The broadcasting media (television and radio) should be used as a health education strategy to cater for the functionally illiterate.
Nursing education
Cancer of the cervix is the most common malignant tumour to affect black females in South Africa. There is an urgent necessity for nurses to be knowledgeable and skilled in the education of females, and in screening for cervical cancer. It is important that the nursing curriculum of both undergraduate/basic and postgraduate/post-basic address content and skill development to empower nurses to meet this challenge.
Nursing research
It is recommended that the study be replicated at a private hospital in order to compare the socio-economic status of the respondents – thus confirming whether or not cervical cancer is a disease of the socioeconomically disadvantaged. A comparative study should be done with HIV-positive and HIV-negative patients in order to ascertain how much influence HIV has on cancer of the cervix. A qualitative study is recommended to determine why women present with advanced disease.
Conclusions
The conclusions drawn from the study was that women’s general knowledge about cancer of the cervix was very poor. The majority of the respondents did not know what caused the symptoms, took some time before they consulted and did not utilize the Pap smear as a preventative and screening measure of the disease. The participants were already exposed to treatment of cervical cancer and they had suffered from this disease for a long time but they still had poor knowledge of it. They could not relate the symptoms they presented with to the disease they had been suffering from for such a long time.
The socio-economic status of the respondents did not confirm that the disease is characteristic of the socio-economically disadvantaged because of the research setting: patients who attended the large academic hospital in Gauteng could not afford private hospitals and did not have medical insurances. It is recommended that the same study be conducted at a private hospital to compare the profile of females utilizing the private health care facilities in order to investigate socio-economic status as a factor in the epidemiology of cancer of the cervix in South Africa, and then a conclusion can be drawn.
This study also supported and demonstrated that health care facilities are efficient in doing Pap smears since patients only saw two health care providers before the diagnosis was made: they did not have to go from pillar to post not knowing what was wrong with them. This study indicated that South African women need health education about cervical cancer.
References
- Rogers-ClarkRC, Smith A (1998) Women’s health: aprimary health care approach, Australia: Maclenan and Pelty Pty.
- Fonn S, Bloch B, Mabina M,Carpenter S, Cronje H, et al. (2002) Prevalenceof pre-cancerous lesions and cervical cancer in South Africa--a multicentrestudy. S Afr Med J 92: 148-156.
- Gaym A, Mashego M,Kharsany AB, Walldorf J, Frohlich J, et al. (2007) High prevalence of abnormalPap smears among young women co-infected with HIV in rural South Africa –implications for cervical cancer screening policies in high HIV prevalencepopulations. S Afr Med J 97: 120-123.
- American Cancer Society(2011) Learn about Cancer. Accessed 14/10/2011.
- Groenwald SL,Frogge MH, Goodman M, Yabro H (1993) Cancernursing principles and practice (3rd edn), London, Jones andBartlett publishers.
- CancerHelpUK (2011) Cervical cancer risks and causes. Accessed 14/10/2011.
- Devita DT, HellmanS, Rosenberg S (2001) Cancer principlesand practice of oncology. (6th edn), USA, Lippincott Williamsand Wilkins.
- MuñozN, Franceschi S, Bosetti C, Moreno V, Herrero R, et al. (2002) Role of parity and human papillomavirus incervical cancer: the IARC multicentric case-control study. The Lancet359: 1093-2101.
- Pervan V, CohenLH, Jaftha T (1995) Oncology for healthcare professionals, RSA, Juta and Company.
- Chamberlain G,Hamilton-Fairley D (1997) Lecture noteson obstetrics and gynaecology, Cornwell: MPG Books limited.
- CassidyJ, Bissett D, Spence OBE RA (2002) Oxfordhandbook of oncology, Great Britain: Oxford University Press.
- Pienaar A,Manaka-Mkhwanazi I (2001) AfricanTraditional Concept of Health Care: Mental Health Nursing- A SouthAfrican perspective. (4th edn), RSA: Juta and Company Limited.
- Steyn M, Muller A (2000) Traditional healers and cancer prevention,Curationis 23: 4-11.
- Klugman S, WeinerR (1992) Women’s health status in SouthAfrica, University of the Witwatersrand : Department of CommunityHealth.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 14638
- [From(publication date):
August-2012 - Oct 04, 2025] - Breakdown by view type
- HTML page views : 10017
- PDF downloads : 4621