Research Article Open Access
Functional Status, Behaviour and Social Interaction of Residents with Dementia Living in Small-Scale and Traditional Long-Term Care Settings in the Netherlands and Belgium
Alida H.P.M. de Rooij1*, Katrien G. Luijkx2, Juliette Schaafsma3, Peggy M.J. Emmerink4, Jos M.G.A. Schols5 and Anja G. Declercq6
1De Kievitshorst Care Center, De Wever, Beneluxlaan 101, 5042 WN, Tilburg, The Netherlands, and Tilburg University, Tranzo Department, Warandelaan 2, 5000 LE, Tilburg, The Netherlands
2Tranzo Department, Tilburg University, Warandelaan 2, 5000 LE, Tilburg, The Netherlands
3Department of Humanities, Tilburg University, Warandelaan 2, 5000 LE, Tilburg, The Netherlands
4De Kievitshorst Care Center, De Wever, Beneluxlaan 101, 5042 WN, Tilburg, The Netherlands
5Department of General Practice and Department of Health Services Research, Maastricht University Caphri, PO Box 616, 6200 MD, Maastricht, The Netherlands
6Department of Lucas, K.U. Leuven, Kapucijnenvoer 39, 3000 Leuven, Belgium
- Corresponding Author:
- Alida H.P.M. de Rooij
Managing Director of De Kievitshorst Care Center/De Wever
Beneluxlaan 101, 5042 WN
Tilburg, The Netherlands
Tel: +31 (0)135 312737
E-mail: I.d.Rooij@dewever.nl
Received date: February 16, 2012; Accepted date: May 07, 2012; Published date: May 09, 2012
Citation: de Rooij AHPM, Luijkx KG, Schaafsma J, Emmerink PMJ, Schols JMGA, et al. (2012) Functional Status, Behaviour and Social Interaction of Residents with Dementia Living in Small-Scale and Traditional Long-Term Care Settings in the Netherlands and Belgium. J Alzheimers Dis Parkinsonism 2:106. doi:10.4172/2161-0460.1000106
Copyright: © 2012 de Rooij AHPM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Alzheimers Disease & Parkinsonism
Abstract
Study background: The aim of this study was to examine how residents with dementia living in small-scale and traditional long-term care settings in the Netherlands and Belgium differ in terms of activities of daily living, behavioural problems, depression, use of restraints, psychotropic medication, social engagement and visiting frequency of relatives. Methods: The study had a longitudinal design with a time interval of one year. Participants were 179 residents with dementia in Dutch small-scale (N=51) and traditional (N=51), and Belgian small-scale (N=47) and traditional (N=30) care settings. Data were obtained by professional caregivers using validated observational measurement instruments. Results: Results show few differences between residents in small-scale and traditional settings in the two countries. In the Netherlands, residents in small-scale settings were more socially engaged and better able to perform activities of daily living compared to residents in traditional settings. In Belgium, residents in small-scale settings were also better able to perform activities of daily living, and showed fewer depressive symptoms than residents in traditional settings. Over time, activities of daily living decreased in residents of both small-scale and traditional settings in both countries. Social engagement also decreased in both countries among residents in small-scale settings but remained stable among residents in traditional settings. Furthermore, behavioural problems decreased over time in traditional settings in both countries, but remained stable in small-scale settings. Conclusions: Relatively few differences were found between small-scale and traditional settings in the two countries as regards residents’ social engagement, activities of daily living, depression and behavioural problems. The assumption made in policy and practice, however, is that living in small-scale settings is better for residents with dementia. To better understand why small-scale settings may not always be more beneficial for residents compared to traditional settings, future research should examine the patterns found in this study in more depth
Keywords
Dementia; Small-scale living; Long-term care; Functional status; Behavioural characteristics; Behavioural interventions; Social interaction
Introduction
Some 4.6 million people are diagnosed with dementia throughout the world every year, and the expectation is that by 2030 there will be around 63 million people suffering from dementia worldwide [1]. The progression of the disease differs for every individual with dementia, as does the care trajectory for individual sufferers [2]. People usually prefer home-based care over residential care, but for a substantial number of people in the later stages of dementia, staying at home is no longer possible [3] and transfer to residential care is inevitable [4]. As the number of people with dementia is expected to increase, the demand for residential care will also increase.
Organizations providing residential care for people with dementia face the challenge of meeting this growing demand. Over the last decade, the emphasis in institutional dementia care has shifted towards a more home-like and person-centred approach, with more attention for the preferences of individual residents [5]. Whereas in traditional residential settings, the institutional rhythm is mainly determined by the logistics of medical and nursing care [6]. This new approach aims to enable residents to continue the way of living they were used to and to offer them possibilities for social participation. For this reason, in many countries with a long history of nursing home care, traditional, largescale nursing homes are currently trying to transform their hospitallike care environments into more normalized and person-centred settings. In addition, many newly developed long-term care settings for older persons with dementia are specifically trying to put this new approach into practice by creating small-scale living facilities [7-9].
An itemized overview of the key differences between typical smallscale and traditional long-term care settings is presented in Table 1.
| Small-scale long-term care settings | Traditional long-term care settings |
|---|---|
| Home-like, holistic and person-centred approacha | Medical- and nursing based approach |
| Focus on the normalization of living and maintenance of oneâÂ?Â?s original lifestyle | Focus on care |
| Additional focus on client interaction | Main focus on basic technical care giving skills |
| Participation in daily activities is stimulated | Staff performs most daily activities |
| Groups are relatively small (usually 6 âÂ?Â? 8) | Groups are larger (usually >20) |
| Day schedule according to residentâÂ?Â?s preferences | Routine institution directed day schedule |
| Environment is familiar and home-like | Environment is hospital-like |
| Number of caregivers is smaller | Number of caregivers is larger |
| Staff wears no uniforms | Staff wears uniforms |
| Staff tasks are integrated b | Staff tasks are more differentiated b |
| More individual decision making by staff members | More collective decision making by staff members |
a This means that the vision of small-scale living is to provide care that fits into the lifestyle that people were used to in their own home (home-like), that encompasses all aspects of people's needs, psychological, physical and social should be taken into account and seen as a whole (holistic) and of which the focus is on the needs of the individual resident (person-centred)
b In traditional long-term care settings staff members usually carry out a specific part of the care tasks. Tasks are thus differentiated between staff members. In small-scale long-term care settings staff members carry out all different tasks, such as cooking and social activities, as well as technical care giving tasks. Thus in these settings there is almost no task specialization.
Table 1: Itemized summary of the key differences between small-scale and traditional long-term care settings.
In today’s residential care practice, it is commonly assumed that small-scale, home-like environments are the preferred and best way to offer care to residents with dementia [10,11]. However, scientific research testing this assumption has thus far only been conducted on a small scale. Moreover, studies that have compared residential living conditions in small-scale and traditional settings have generally found mixed results and have not provided solid support for this assumption [7,12,13].
Furthermore, studies comparing traditional and small-scale living facilities have primarily focused on quality of life of the residents as the primary outcome [7,12,14,15]. Although quality of life of residents is a very important outcome parameter in the assessment of a care programme [16], it is also possible that residents of small-scale and traditional living facilities differ on other important outcome aspects, such as activities of daily living (ADL), behaviour and social interaction of persons with dementia. Yet, only a few researchers have compared traditional and small-scale care settings on one or more of these aspects [17-19]. An integral array of aspects influencing residents with dementia, incorporating for example behavioural problems, use of restraints and visits from family members, has to date not been examined in a single study design.
The aim of the present study was to fill this gap by examining the effect of living in a small-scale or traditional long-term care setting on functional status, behaviour and social interaction of people with dementia. More specifically, we examined whether and how residents in small-scale and traditional settings differ in functional status (i.e. the level of dependency in activities of daily living) and also in terms of behavioural characteristics (i.e. behavioural problems and depression), behavioural interventions (i.e. use of restraints and psychotropic medication) and social interaction (i.e. social engagement and visits from family). We also examined whether and how residents’ scores on these aspects changed over time (one year). This was done to rule out the possibility that findings might represent only a random indication at a specific moment in time. Furthermore, this allowed us to examine whether residents in small-scale settings would remain more stable over time in terms of their physical, psychological, and social functioning compared to residents in traditional settings. Data were collected among residents of small-scale and traditional settings in the Netherlands and in Belgium.
In this study, we expect that residents in small-scale living settings will show less decline in terms of their functional status compared to residents in traditional settings [12,18], in particular because smallscale settings offer residents more opportunities to perform activities of daily living themselves. There is evidence that this positively affects the independence of older people with dementia [20,21].
Mild to severe behavioural problems are present in about 64% of all cases of dementia [22]. We have no clear hypotheses about whether residents in small-scale settings differ from residents in traditional settings in terms of behavioural problems, because previous research has found no differences between units on this aspect [12,14,17].
One third of all people diagnosed with dementia also experience depressive symptoms [23] which have a very marked negative influence [24,25]. Nevertheless, it is unclear whether residents in small-scale and traditional settings differ in terms of depressive symptoms. Whereas some studies have found that residents in small-scale living settings reported fewer depressive symptoms [19] and had better emotional health [7] compared to residents in traditional nursing home care, a recent study in the Netherlands found no differences between smallscale living and traditional long-term care in terms of depression [14].
There is an ongoing discussion in the field of dementia care about the use of behavioural interventions, involving the need for and safety of the use of restraints and psychotropic medication. In longterm care settings it is still common practice for an array of restraints to be used. Research on the efficiency of restraints in nursing homes has, however, shown that restrictive devices can often be removed without negative consequences and that this is associated with positive patient outcomes [26]. Despite inconsistent results, we hypothesize that the use of restraints will be lower in small-scale living facilities compared to traditional units. Also administering psychotropic drugs to residents with dementia to control their neuropsychiatric symptoms is still common practice, but whether they are beneficial in all cases is questionable [27]. Prescription of psychotropic medication is expected to be lower in small-scale settings because the majority of studies have confirmed that psychotropic medication is less often prescribed for residents in small-scale settings [12,14].
Although social engagement is likely to change for a person with dementia (i.e. making contact often becomes more difficult as the disease progresses), they may actually benefit from targeted social interaction [28]. Regular visits from family and friends may temporarily reduce agitation [29] and visits in general have been shown to positively affect behavioural problems [30]. We expect residents in small-scale settings to be more socially engaged than residents in traditional dementia care units. In this regard, studies on small-scale living have also found that residents in small-scale care facilities are more frequently engaged in verbal communication [19], show more interest in their surroundings [18] and have better relationships with other residents and caregivers in the facility compared to traditional care settings [7]. One recent study in the Netherlands also found that residents in small-scale living settings were more socially engaged compared to residents living in traditional units [12]. We also expect the visiting frequency of relatives to be higher for residents in smallscale living settings compared to those in traditional settings, because small-scale facilities are likely to be more appealing for family members than the hospital-like environment in traditional units.
Setting the scene
This study was conducted in the Netherlands and Belgium. Both countries are welfare states, providing services for everyone in need of long-term care. Although the financing and funding systems of longterm dementia care show similarities in both countries, there are also some differences [10,31]. Funding of long-term care in the Netherlands is based on a system of Care Severity Packages provided by law (the Exceptional Medical Expenses Act, AWBZ) [32], which are individual budgets paid to institutions to enable them to provide care to their residents [33]. Residents are obliged to make an income-dependent contribution [34]. In Belgium, nursing homes are partly funded by the federal government and partly by the regional authorities. Additionally, residents have to pay a daily fee for food and lodging [35].
Moreover, Belgium has a longer history (since 1978) of small-scale long-term care [11] than the Netherlands (since 1986) [36]. In Dutch small-scale facilities, groups usually comprise six to eight residents [37], whereas in Belgium the number is usually between six and nine [11] and in Belgium the groups are sometimes enlarged to 12 to 15 residents due to funding issues [11].
Given these and other differences between the two countries, the focus in this study was on within-country comparisons between small-scale and traditional settings, rather than on between-country comparisons (e.g. between small-scale settings in the Netherlands and Belgium). We expected, however, to find a similar pattern of results in the two countries, because of the various similarities in their vision on and organisation of dementia care.
Materials and Methods
This study had a longitudinal design, with three measurement moments over a period of one year. Data were gathered at baseline, after six months and after twelve months in traditional and smallscale long-term care settings in the Netherlands and Belgium. The study was part of a larger longitudinal study on the similarities and differences between traditional and small-scale long-term dementia care settings, examining residents, family and professional caregivers in the Netherlands and Belgium [38]. The focus in this study was on functional status, various behavioural characteristics, behavioural interventions, and social interaction.
Sample
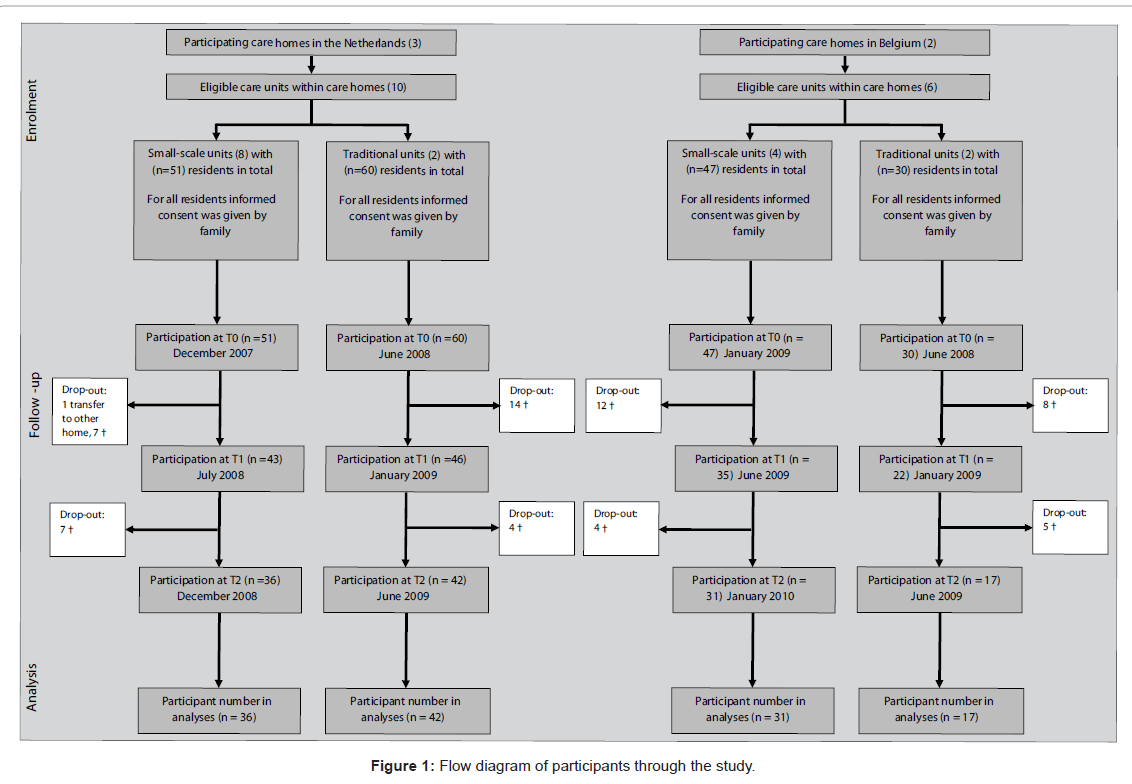
Five institutional long-term care organizations, operating four traditional and 12 small-scale units in the south of the Netherlands and the north of Belgium, were approached for the study and were willing to participate. Data were obtained from 179 residents (142 female, 37 male) aged over 65 years with dementia, who had been assessed to be suffering from dementia and in need of residential psychogeriatric care prior to their admission to the long-term care setting. Due to the severity of the disease, all participants in this study were not competent to act for themselves and were under the supervision of a legal representative. The representative is usually a family member; the assignment of responsibilities is controlled by law. Where no family members are available, an independent guardian is appointed by the relevant legal authority. For this study, the legal representatives gave informed consent on behalf of the participants. Data collection took place between December 2007 and January 2010. See Figure 1 for a flow diagram containing participant numbers in each setting at the different measurement moments.
Procedure
We selected validated observational assessment instruments (mainly questionnaires) that had to be filled in by professional caregivers and were applicable to older people in all stages of dementia. This method of observation is considered to be the best, most reliable and valid alternative method of data gathering [39]. Moreover, the instruments used were available in the residents’ and professional caregivers’ native language (Dutch). All questionnaires were completed at three measurement moments (at baseline, after six months and after 12 months) to examine changes over time and rule out the possibility that the findings might represent only a random indication at a specific moment in time.
Measurements and measurement instruments
To examine functional status, the Barthel Index [40] was administered. This index measures independence in ten basic activities of daily living, including personal hygiene, using the toilet, getting dressed, walking up and down stairs, bathing, mobility, (in) continence, requiring assistance in transferring from bed to chair, and requiring assistance with feeding. A score of 0 to 2 or 0 to 3 is recorded for each activity. The maximum possible score is 20, ranging from 0 to 4 = completely dependent through to 20 = completely ADL-independent [40]. The Barthel Index was filled in by nurses or nursing assistants who knew the residents very well.
Behavioural problems were assessed using the NPI-NH (Neuropsychiatric Inventory - Nursing Home Version), measuring separate behavioural disorders such as delusions, hallucinations, agitation, phobia, euphoria, apathy, aberrant motor behaviour, sleeping and eating disorders [41]. The NPI-NH gives an insight into the severity, frequency and workload of each of the separate behavioural disorders [41]. Behavioural problems were assessed by an independent psychologist interviewing the nurse or nursing assistant.
Depression was measured using the CSDD (Cornell Scale for Depression in Dementia), which has been specifically developed to identify depressive symptoms in older people with dementia [42]. The CSDD incorporates mood, behavioural disorders, physical characteristics of depression and cyclical functions and disorders in cognitive content. The observational scale contains 19 items and ranges from: a = cannot be judged, 0 = absent, 1 = mild, 2 = severe. Scores above 18 indicate a definite major depression [42]. The CSDD was filled in by nurses or nursing assistants who knew the residents very well.
The use of physical restraints, being any limitations imposed on an individual’s freedom of movement [43], including their number and type, was recorded as absent or present from the personal files of the residents. The range of restraining measures included fixation with belts, small and large bed-belts, (wheel) chair belts, securing the person to the mattress with a sheet, using a fixed table top in a chair, use of bilateral full-enclosure bedrails, and use of sensor mats and infrared sensors (motion alarms) in the bedroom.
The number of different psychotropic medications prescribed was taken from the medical files of the residents. Psychotropic medication was divided into three types: sedatives, antidepressants and antipsychotics [44].
Social engagement was measured using the RISE (Revised Index of Social Engagement), which is a subscale taken from the larger Resident Assessment Instrument 2.0 (RAI 2.0) [45]. The Revised Index for Social Engagement (RISE) measures the social involvement of residents with other residents, professional caregivers and relatives. The scale contains eight questions about the social interaction of the resident, indicating whether or not the specific social situation mentioned in the question has occurred over the last seven days. RISE is one of the scales derived from the larger instrument Resident Assessment Instrument 2.0 (RAI 2.0) [45]. The RAI 2.0 is used to assess a variety of factors related to the functioning of residents in care homes [46]. The RISE was filled in by nurses or nursing assistants who knew the residents very well.
The visiting frequency of relatives was recorded by a nurse or nursing assistant on a five-point scale ranging from almost every day, once or twice a week, once every two weeks, once a month to less than once a month.
To be able to control for potential differences in basic characteristics, age, sex and cognitive impairment were recorded. Residents with dementia being older or more severely impaired might perform worse on patient outcomes, just due to their impairment, and not due to living in a particular type of care unit. Age and sex were taken from the personal records of the residents. All residents had received a diagnosis of dementia prior to admission to the care facility. The S-MMSE (Standardized Mini Mental State Examination) was administered to each resident to assess the severity of cognitive impairment [47,48]. Residents were asked to answer a series of 11 questions. The maximum possible test score was 30 [48]. This test was performed by an independent psychologist interviewing the residents themselves.
To control for the number of nursing staff available to residents, full-time equivalent data (corrected for the number of residents living in each group) were collected for each care unit.
Analytic strategy
The data gathered had a ‘multilevel data structure’, i.e. observations over time (level 1) were nested within persons (level 2), which were then nested within settings (level 3). For this reason, the data were analyzed using a series of multilevel modelling analyses, using the HLM program [49].
In the first set of analyses, we estimated means for different outcome measures, and compared these means across the different types of settings in Belgium and the Netherlands. No predictors were entered in the level-1 and level-2 models, and so these models were “totally unconditional”. Differences among the small-scale and traditional settings in the Netherlands and Belgium were examined at level 3 with so-called no-intercept models, and the coefficients that resulted from these analyses represent the mean for each site on a specific measure. In a series of follow-up analyses, these coefficients (mean scores) were compared using ‘tests of fixed effects’ [50,51]. In these analyses, the means of the traditional and small-scale settings were compared within Belgium and the Netherlands1.
| Netherlands Traditional (A) (2 wards, n=51) | Netherlands Small-scale (B) (8 wards, n=51) | Belgium Traditional (C) (2 wards, n=30) | Belgium Small-scale (D) (4 wards, n=47) | |
|---|---|---|---|---|
| Age in years, M(SD) | 83.99 (5.12) C | 84.50 (5.86) C | 89.09 (5.67) A, B, D | 84.52 (7.05) C |
| Women (%) | 34 (67%) | 41 (80%) | Â 25 (83%) | 42 (89%) |
| S-MMSE (0-30) 1 | 4.96 (5.59) | 7.61 (6.26) | 8.10 (8.06) | 6.07 (5.57) |
| FTE 2 | 19.45 | 11.95 | 12.67 | 13.15 |
| Number of residents per unit, n | 30 (2 living rooms with 15 residents) | 12 (2 living rooms with 6 residents) | 30 (2 living rooms with 15 residents) | 30 (2 living rooms with 15 residents) |
| Available hours of care per capita, in hours per week | 23.34 | 35.85 | 16.05 | 16.66 |
Note: F-tests were conducted and letters are assigned to groups in superscripts indicating significantly different pairs (following Bonferroni correction) at the p <.01 level, two-tailed.
1 Higher scores mean better cognitive skills (S-MMSE).
2 FTEs are calculated on the basis of data provided by the nursing homes. A single FTE consists of 36 working hours in the Netherlands and 38 working hours in Belgium. Only nurses and nursing assistants were included (i.e. no medical doctors, physiotherapists, psychologists etc.).
Table 2: Characteristics of residents (N=179) and traditional and small-scale settings in the Netherlands and Belgium.
| The Netherlands | Belgium | |||
|---|---|---|---|---|
| Traditional | Small-scale | Traditional | Small-scale | |
| Activities of Daily Living (0-20) |  4.03 |  8.15*** |  5.14 |  6.97âÂ? |
| Behavioural Problems (0-144) | 17.53 | 21.43 | 15.75 | 17.57 |
| Depression (0-38) |  8.45 |  8.37 | 10.27 |  8.50âÂ? |
| Use of Restraints (#) | Â 1.11 | Â 1.18 | Â 1.11 | Â 1.16 |
| Prescription of Psychotropic Medication (#) | Â 1.47 | Â 1.29 | Â 1.68 | Â 1.99 |
| Social Engagement (0-8) | Â 2.43 | Â 3.69** | Â 2.52 | Â 2.71 |
| Visiting Frequency (1-5) | Â 2.27 | Â 1.95 | Â 2.25 | Â 2.07 |
Note: An asterisk indicates that the mean on a scale in traditional settings is significantly different from the mean in small-scale settings in the same country: *** p <.001, ** p < .01, âÂ? p < .10.
A higher score indicates a better ability to perform activities of daily living, more behavioural problems, higher depression, a higher number of absolute restraints and prescribed medications, more social engagement (rate 0-8 activities in the past two weeks) and fewer visits (1 = almost every day, 2 = once or twice a week, 3 = once every two weeks, 4 = once a month or 5 = less than once a month).
Table 3: Within-country comparisons of means (Aggregated across time) for functional status, behavioural characteristics, behavioural interventions and social interaction by type of setting.
A second set of analyses examined changes across time in the different outcome measures for small-scale and traditional settings in the Netherlands and Belgium. For this purpose, time of measurement (coded as 0, 1, or 2) was added (uncentered) at level 1. At level 2, no predictors were entered and at level 3, differences in the Time slope across small-scale and traditional settings in the Netherlands and Belgium were again examined with so-called no intercept models. In this model, the Time slope (Β10j) was brought up from level 1 and the resulting coefficients represented the mean slopes for each type of living facility in each country. Effects were modelled as fixed when the random error term was not significant2.
Results
Basic characteristics of participants and settings
Table 2 presents descriptive data of residents by country and type of setting. The mean age of the residents in years ranged from 83.99 in Dutch traditional settings to 89.09 in the Belgian traditional settings.
Mean differences in functional status, behavioural characteristics, behavioural interventions and social interaction between small-scale and traditional settings
Table 3 presents an overview of the (unadjusted) mean scores (aggregated over the three measurement moments) on the different measures in traditional and small-scale settings in the Netherlands and Belgium.
It was found that residents in small-scale settings in the Netherlands were reported to be more socially engaged (p = 0.004) and to be more independent in performing activities of daily living (p < 0.001) compared to residents in traditional settings. On the other measures, however, no differences were found between small-scale and traditional settings in the Netherlands. In Belgium, two differences were found between small-scale and traditional settings that reached conventional levels of significance: residents in small-scale settings were somewhat more independent in performing activities of daily living (p = 0.09), and were also reported to display fewer depressive symptoms (p = 0.09).
| Measure (Range) | Coëfficiënt | Baseline | Time 1 | Time 2 |
|---|---|---|---|---|
| Activities of Daily Living (0-20) | ||||
| Netherlands | ||||
| Traditional | -1.26*** | Â 5.15 | 3.89 | 2.63 |
| Small-scale | -0.81** | Â 8.82 | 8.01 | 7.20 |
| Belgium | ||||
| Traditional | -1.27** | Â 6.02 | 4.75 | 3.48 |
| Small-scale | -1.72*** | Â 8.28 | 6.56 | 4.84 |
| Behavioural Problems | ||||
| Netherlands | ||||
| Traditional | -3.72*** | 20.84 | 17.12 | 13.40 |
| Small-scale | -2.28 | 23.20 | 20.92 | 18.64 |
| Belgium | ||||
| Traditional | -4.52*** | 19.21 | 14.69 | 10.17 |
| Small-scale | Â 0.10 | 17.50 | 17.60 | 17.70 |
| Depression (0-38) | ||||
| Netherlands | ||||
| Traditional | Â 0.71 | Â 7.82 | 8.53 | 9.24 |
| Small-scale | -0.26 | Â 8.60 | 8.34 | 8.08 |
| Belgium | ||||
| Traditional | -1.16 | 11.05 | 9.89 | 8.73 |
| Small-scale |  1.03âÂ? |  7.72 | 8.75 | 9.78 |
| Use of Restraints (#) | ||||
| Netherlands | ||||
| Traditional | 0.10 | 1.03 | Â 1.13 | 1.23 |
| Small-scale | 0.04 | 1.14 | Â 1.18 | 1.22 |
| Belgium | ||||
| Traditional | 0.09 | 1.05 | Â 1.14 | 1.23 |
| Small-scale | 0.23** | 0.99 | Â 1.22 | 1.45 |
| Prescription of Psychotropic Medication (#) | ||||
| Netherlands | ||||
| Traditional | -0.05 | Â 1.51 | 1.46 | 1.41 |
| Small-scale | Â 0.15** | Â 1.16 | 1.31 | 1.46 |
| Belgium | ||||
| Traditional | -0.02 | Â 1.70 | 1.68 | 1.66 |
| Small-scale | Â 0.20** | Â 1.84 | 2.04 | 2.24 |
| Social Engagement (0-8) | ||||
| Netherlands | ||||
| Traditional | -0.13 | Â 2.56 | 2.43 | 2.30 |
| Small-scale | -0.67** | Â 4.28 | 3.61 | 2.94 |
| Belgium | ||||
| Traditional | -0.01 | Â 2.54 | 2.53 | 2.52 |
| Small-scale | -0.64* | Â 3.20 | 2.56 | 1.92 |
| Visiting Frequency (1-5) | ||||
| Netherlands | ||||
| Traditional | 0.02 | 2.24 | 2.26 | 2.28 |
| Small-scale | 0.04 | 1.91 | 1.95 | 1.99 |
| Belgium | ||||
| Traditional | 0.14 | 2.15 | 2.29 | 2.43 |
| Small-scale | 0.14* | 1.97 | 2.11 | 2.25 |
A higher score indicates a better ability to perform activities of daily living, more behavioural problems, higher depression, a higher number of absolute restraints and prescribed medications, more social engagement (rate 0-8 activities in the past two weeks) and fewer visits (1 = almost every day, 2 = once or twice a week, 3 = once every two weeks, 4 = once a month or 5 = less than once a month). Withincountry significantly different slopes are indicated by asterisks: *** p <.001, ** p < .01, * p < .05 âÂ? p < .10.
Table 4: Relationship between time of measurement of functional status, behavioural characteristics, behavioural interventions and social interaction in traditional and small-scale settings in the Netherlands and Belgium: Coefficients and estimated mean scores.
In an additional set of analyses, we controlled for relevant background variables (i.e., sex, age, cognitive impairment, and FTE nursing staff). This did not change the pattern of results meaningfully, however, except that the p-value for the difference between small-scale and traditional settings in Belgium in independence in activities of daily living when controlling for cognitive impairment decreased from (p = 0.09) to (p = 0.02).
Changes across time within Dutch and Belgian small-scale and traditional settings
The results from the analyses assessing changes across time are presented in Table 4.
As can be deduced from this table, the pattern of results was roughly similar for the Dutch and Belgian samples. At baseline, social engagement was relatively high in small-scale settings in both countries but decreased over time (ps < 0.016)3 and at Time 2 social engagement scores in small-scale and traditional settings were comparable. Independence in activities of daily living decreased in both traditional and small-scale settings in Belgium and the Netherlands (ps < 0.006), but were still meaningfully higher at Time 2 in small-scale settings than in traditional wards. It was also found, however, that the use of psychotropic medication increased in smallscale settings in both the Netherlands and Belgium (ps < 0.023). Furthermore, it was found that mean scores on behavioural problems decreased over time in traditional wards in the Netherlands and Belgium, but not in small-scale settings (ps < 0.024). In the Belgian sample, the use of restraints also increased over time in small-scale settings (p = 0.005), as did the visiting frequency of relatives (p = 0.046).
In an additional set of analyses, we controlled for relevant background variables (age, sex, cognitive impairment, group size and FTE nursing staff). This did not, however, change the pattern of results meaningfully.
Discussion
This study examined whether residents in small-scale settings, compared to residents in traditional settings, show less decline in functional status, display different levels of behavioural problems, have different levels of depressive symptoms, are more socially engaged and receive more visits from family. Moreover, it was also examined whether fewer restraints were employed and whether less medication was prescribed in small-scale settings. Contrary to our expectations, it was found that residents in small-scale settings differed on only a few aspects from residents in traditional settings. In the Netherlands, residents in small-scale settings were more independent in activities of daily living and were also more socially engaged compared to residents in traditional settings. In Belgium, residents in small-scale settings were found to be more independent in activities of daily living and were also reported to display fewer depressive symptoms. The results in the Dutch and Belgian settings on independence in ADL resemble the results of two recent studies in the Netherlands [12,37] and are in line are encouraged to perform activities themselves (as long as possible) and have more opportunities to participate socially. Moreover, a difference was found in the Belgian settings on depression, where residents in small-scale settings displayed fewer depressive symptoms. This finding is in line with some other previous studies that found fewer depressive symptoms and better emotional health in small-scale settings [7,19]. On the other dimensions, however, no differences were found between small-scale and traditional settings. Looking at changes across time, the results were roughly similar in the Netherlands and Belgium. Nevertheless, some interesting differences between residents in small-scale and traditional settings appeared. At baseline, social engagement of residents was relatively high in small-scale settings in both countries but decreased over time, while the level of engagement in traditional settings remained the same. This is interesting, because other studies comparing small-scale and traditional settings found evidence that residents in small-scale settings are generally more socially engaged [7,14,18,19]. Furthermore, activities of daily living decreased over time in both traditional and small-scale settings in both countries. However, they were still meaningfully higher after one year in smallscale compared to traditional settings.
The use of psychotropic medication increased in small-scale settings in the Netherlands and Belgium, whereas it remained the same in traditional settings. Because these results did not fit in with our expectations, we checked whether in daily practice medication prescription protocols differed between small-scale and traditional long-term care settings. We found that the protocols indeed did not differ much, which might be a possible explanation for finding no differences in medication prescription.
Behavioural problems remained stable in small-scale settings, whereas in traditional settings the number of behavioural problems displayed by residents decreased over time. It might be that the differences in patterns can be explained by the more structured living environment and fixed daily rhythm in traditional settings. However, on the basis of our data we cannot draw definite conclusions. Therefore, these differences deserve more research attention.
All in all, this study demonstrates that small-scale settings seem to be positively related to residents’ social engagement, activities of daily living, depression and visiting frequency, whereas traditional settings seem to be positively related to behavioural problems. Nevertheless, this study also has some limitations. Due to ethical considerations, a randomised controlled trial design was impossible. Although the participating settings were selected based on their similar view of care giving, the small-scale and traditional settings in the two countries might possibly differ on aspects that were not taken into account, such as different nursing methods, handling of behavioural problems, staff attitudes, design of the environment, culture, atmosphere and means of family participation in care. The settings are real-life care settings and have specific characteristics that may vary within and between countries.
In daily long-term care practice, it is still assumed that living in small-scale settings is more beneficial for residents with dementia, and this vision also dominates policy and practice. However, the findings of this study do not provide unconditional support for this assumption, and future studies should examine this in more detail. For example, qualitative studies might provide a better understanding of the patterns that were found in this study. Moreover, future research in this field should focus more on the quality and content of the care provided.
Acknowledgements
The authors would like to thank Caroline Wouters, an independent psychologist, for her assistance with data collection, and Julian Ross, for providing linguistic help.
Conflict of Interest
No one to declare.
Funding
This study was funded by De Wever, The Society for Nursing Home Care and Tranzo, Tilburg University.
Ethical Approval
This study was part of a project registered under trial number: Current Controlled Trials ISRCTN23772945. The Ethics Committee at De Wever care organisation, Tilburg, gave its approval for the complete trial in September 2008. The study protocol was published elsewhere [42].
1 The level 1 model in these analyses was as follows: ytij = π0ij + etij. In this model, ytij is an outcome measure (e.g. social engagement) at time t for person i in setting j, π0ij is a random coefficient representing the mean of y for person i in setting j, and etij represents the error associated with each measure. The level 2 model was: π0ij = β0ij + r0ij. In this model, β0ij is the mean on an outcome measure in setting j, and r0ij is a random “setting” effect (i.e., the deviation of person ij’s mean from the setting mean). At level 3, the model was: β0ij= γ001(BSmall)j + γ002(BTrad)j + γ003(NSmall) j +γ004(NTrad)j + u0ij. In these models, BSmall, BTrad, NSmall, and NTrad were uncentered dummy-coded variables representing the small-scale or traditional settings in Belgium or the Netherlands.
2 In these analyses, the level 1 model was: ytij = π0ij + π1ij (Time)tij + etij. In this model, π1ijrepresents the relationship between time of measurement (at baseline, after six months, and after one year) and an outcome measure. At level 2, the model was: π0ij = β00j + r0ij. At level 3, the Time slope (Β10j) was brought up from level 1 in the following model: Β10j = γ001(BSmall)j + γ002(BTrad) j + γ003(NSmall) j + γ004(NTrad) j + u10j. The resulting coefficients represented the mean slopes for each type of living facility in each country.
3 ps stands for p-value in plural, for example (ps < 0.016) means that all found p-values of the indicated effect were below .016.
References
- Wimo A, Winblad B, Aguero-Torres H, von Strauss E (2003) The magnitude of dementia occurrence in the world. Alzheimer Dis Assoc Disord 17: 63-67.
- Gustafson L (1996) What is dementia? Acta Neurol Scand Suppl 168: 22-24.
- Mitchell SL, Morris JN, Park PS, Fries BE (2004) Terminal care for persons with advanced dementia in the nursing home and home care settings. J Palliat Med 7: 808-816.
- Schols J, De toekomst van de chronische zorg ... ons een zorg? Van oude structuren, de dingen, die voorbijgaan... (The future of care for the chronically ill ... do we care?) ISBN: 90-3619-092-4, 2004, Dutch University Press: Tilburg.
- Flicker L (1999) Dementia reconsidered: the person comes first. BMJ 318: 880A.
- White-Chu EF, Graves WJ, Godfrey SM, Bonner A, Sloane P (2009) Beyond the medical model: the culture change revolution in long-term care. J Am Med Dir Assoc 10: 370-378.
- Kane RA, Lum TY, Cutler LJ, Degenholtz HB, Yu TC (2007) Resident outcomes in small-house nursing homes: a longitudinal evaluation of the initial green house program. J Am Geriatr Soc 55: 832-839.
- Morley JE, Flaherty JH (2002) Putting the "home" back in nursing home. J Gerontol A Biol Sci Med Sci 57: M419-M421.
- Rabig J, Thomas W, Kane RA, Cutler LJ, McAlilly S (2006) Radical redesign of nursing homes: applying the green house concept in Tupelo, Mississippi. Gerontologist 46: 533-539.
- Bussemaker J (2009) Stimuleren kleinschalig wonen voor mensen met dementia. Ministerie van Volksgezondheid Welzijn en Sport 1-8.
- Van Audenhove C, Declercq A, De Coster I, Spruytte N, Molenberghs C, et al. (2003) Kleinschalig genormaliseerd wonen voor personen met dementia. Garant Uitgevers NV.
- te Boekhorst S, Depla MF, de Lange J, Pot AM, Eefsting JA (2009) The effects of group living homes on older people with dementia: a comparison with traditional nursing home care. Int J Geriatr Psychiatry 24: 970-978.
- Verbeek H, van Rossum E, Zwakhalen SM, Kempen GI, Hamers JP (2009) Small, homelike care environments for older people with dementia: a literature review. Int Psychogeriatr 21: 252-264.
- Verbeek H, Zwakhalen SM, van Rossum E, Ambergen T, Kempen GI, et al. (2010) Dementia care redesigned: Effects of small-scale living facilities on residents, their family caregivers, and staff. J Am Med Dir Assoc 11: 662-670.
- de Rooij AH, Luijkx KG, Schaafsma J, Declercq AG, Emmerink PM, et al. (2012) Quality of life of residents with dementia in traditional versus small-scale long-term care settings: A quasi-experimental study. Int J Nurs Stud
- Prince PN, Prince CR (2001) Subjective quality of life in the evaluation of programs for people with serious and persistent mental illness. Clin Psychol Rev 21: 1005-1036.
- Macdonald A, Philpot M, Briggs C (2004) An attempt to determine the benefits of a 'home-for-life' principle in residential care for people with dementia and behavioural problems: a comparative cohort study. Dement Geriatr Cogn Disord 18: 6-14.
- Reimer MA, Slaughter S, Donaldson C, Currie G, Eliasziw M (2004) Special care facility compared with traditional environments for dementia care: a longitudinal study of quality of life. J Am Geriatr Soc 52: 1085-1092.
- Ritchie K, Colvez A, Ankri J, Ledesert B , Gardent H, et al. (1992) The evaluation of long-term care for the dementing elderly: A comparative study of hospital and collective non-medical care in France. Int J Geriatr Psychiatry 7: 549-557.
- Andersen CK, Wittrup-Jensen KU, Lolk A, Andersen K, Kragh-SÃÂ?¸rensen P (2004) Ability to perform activities of daily living is the main factor affecting quality of life in patients with dementia. Health Qual Life Outcomes 2: 52.
- Woods B (1999) Promoting well-being and independence for people with dementia. Int J Geriatr Psychiatry 14: 97-105.
- Bellelli G, Frisoni GB, Bianchetti A, Boffelli S, Guerrini GB, et al. (1998) Special care units for demented patients: a multicenter study. Gerontologist 38: 456-462.
- Prado-Jean A, Couratier P, Druet-Cabanac M, Nubukpo P, Bernard-Bourzeix L, et al. (2010) Specific psychological and behavioral symptoms of depression in patients with dementia. Int J Geriatr Psychiatry 25: 1065-1072.
- Mahendra B (1985) Depression and dementia: the multi-faceted relationship. Psychol Med 15: 227-236.
- Teri L (1994) Behavioral treatment of depression in patients with dementia. Alzheimer Dis Assoc Disord 8: 66-74.
- Capezuti E (2004) Minimizing the use of restrictive devices in dementia patients at risk for falling. Nurs Clin North Am 39: 625-647.
- Tjia J, Rothman MR, Kiely DK, Shaffer ML, Holmes HM, et al. (2010) Daily medication use in nursing home residents with advanced dementia. J Am Geriatr Soc 58: 880-888.
- Perrin T (1997) Occupational need in severe dementia: a descriptive study. J Adv Nurs 25: 934-941.
- Martin-Cook K, Hynan L, Chafetz PK, Weiner MF (2001) Impact of family visits on agitation in residents with dementia. Am J Alzheimers Dis Other Demen 16: 163-166.
- Minematsu A (2006) The frequency of family visits influences the behavioral and psychological symptoms of dementia (BPSD) of aged people with dementia in a nursing home. Journal of Physical Therapy Sciences 18: 123-126.
- Spruytte N, LUCAS (2009) Kleinschalig genormaliseerd wonen voor mensen met dementie: Het antwoord op 101 vragen. Garant Uitgevers NV 234.
- Den Haag (1967) Ministerie van Volksgezondheid Welzijn en Sport, Algemene Wet Bijzondere Ziektekosten (AWBZ).
- Hoeksma HEM, Zorgzwaartepakketten sector V&V, in HHM, W.e.s.M.v. Volksgezondheid, Editor 2008.
- Schols JM, Crebolder HF, van Weel C (2004) Nursing home and nursing home physician: the Dutch experience. J Am Med Dir Assoc 5: 207-212.
- Juriwel (2009) Woonzorgdecreet (Decree of Department of Health Care) Juriwel 1-17.
- Van Ijperen MJ (2005) Kleinschalige zorg; grote verschillen? Erasmus University Rotterdam 1-108.
- Verbeek H (2011) Redesigning dementia care. Maastricht: Maastricht University.
- de Rooij AH, Luijkx KG, Declercq AG, Schols JM (2011) Quality of life of residents with dementia in long-term care settings in the Netherlands and Belgium: design of a longitudinal comparative study in traditional nursing homes and small-scale living facilities. BMC Geriatr 11: 20.
- SchÃÂ?¶lzel-Dorenbos CJ, Ettema TP, Bos J, Boelens-van der Knoop E, Gerritsen DL, et al. (2007) Evaluating the outcome of interventions on quality of life in dementia: selection of the appropriate scale. Int J Geriatr Psychiatry 22: 511-519.
- MAHONEY FI, BARTHEL DW (1965) FUNCTIONAL EVALUATION: THE BARTHEL INDEX. Md State Med J 14: 61-65.
- Iverson GL, Hopp GA, DeWolfe K, Solomons K (2002) Measuring change in psychiatric symptoms using the Neuropsychiatric Inventory: Nursing Home version. Int J Geriatr Psychiatry 17: 438-443.
- Alexopoulos GS, Abrams RC, Young RC, Shamoian CA (1988) Cornell Scale for Depression in Dementia. Biol Psychiatry 23: 271-284.
- Gulpers MJ, Bleijlevens MH, van Rossum E, Capezuti E, Hamers JP (2010) Belt restraint reduction in nursing homes: design of a quasi-experimental study. BMC Geriatr 10: 11.
- WHO, Anatomical Therapeutic Chemical (ATC) classification index with defined daily doses (DDDs) for plain substances 1997, Oslo: World Health Organization Collaborating Centre for Drug Statistics Methodology.
- Gerritsen DL, Steverink N, Frijters DH, Hirdes JP, Ooms ME, et al. (2008) A revised Index for Social Engagement for long-term care. J Gerontol Nurs 34: 40-48.
- Achterberg W, Pot AM, van Campen C, Ribbe M (1999) [Resident Assessment Instrument (RAI): a review of international research on the psychometric qualities and effects of implementation in nursing homes]. Tijdschr Gerontol Geriatr 30: 264-270.
- Haubois G, Annweiler C, Launay C, Fantino B, de Decker L, et al. (2011) Development of a short form of Mini-Mental State Examination for the screening of dementia in older adults with a memory complaint: a case control study. BMC Geriatr 11: 59.
- Molloy DW, Alemayehu E, Roberts R (1991) Reliability of a Standardized Mini-Mental State Examination compared with the traditional Mini-Mental State Examination. Am J Psychiatry 148: 102-105.
- Raudenbush SW, Anthony Bryk, Yuk Fai Cheong, Richard Congdon, Mathilda du Toit (2004) HLM 6: Hierarchical and nonlinear modeling. Lincolnwood, IL: Scientific Software International, Inc.
- Nezlek JB (2001) Multilevel random coefficient analyses of event and interval contingent data in social and personality psychology research. Pers Soc Psychol Bull 27: 771-785.
- Raudenbush SW, Bryk AS (2002) Hierarchical linear models: Applications and data analysis methods, (2nd edn), Newbury Park, CA: Sage.
Relevant Topics
- Advanced Parkinson Treatment
- Advances in Alzheimers Therapy
- Alzheimers Medicine
- Alzheimers Products & Market Analysis
- Alzheimers Symptoms
- Degenerative Disorders
- Diagnostic Alzheimer
- Parkinson
- Parkinsonism Diagnosis
- Parkinsonism Gene Therapy
- Parkinsonism Stages and Treatment
- Stem cell Treatment Parkinson
Recommended Journals
Article Tools
Article Usage
- Total views: 14560
- [From(publication date):
August-2012 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 10025
- PDF downloads : 4535