Research Article Open Access
Evaluation of Different Strategies for Post-Exposure Treatment of Ebola Virus Infection in Rodents
Jason S. Richardson1#, Gary Wong1,3#, Stéphane Pillet1, Samantha Schindle1, Jane Ennis2, Jeffrey Turner2, James E. Strong1,3 and Gary P. Kobinger1,3,4*
1Special Pathogens Program, National Microbiology Laboratory, Public Health Agency of Canada, Winnipeg, Manitoba, Canada
2Defyrus Incorporated, Toronto, Ontario, Canada
3Department of Medical Microbiology, University of Manitoba, Winnipeg, Manitoba, Canada
4Department of Immunology, University of Manitoba, Winnipeg, Manitoba, Canada
#The authors contributed equally to the work.
- *Corresponding Author:
- Gary P. Kobinger, PhD
Special Pathogens Program
National Microbiology Laboratory
Public Health Agency of Canada
1015 Arlington Street,Winnipeg
MB, R3E 3R2, Canada
Tel: 204-784-5923
Fax: 204-789-2140
E-mail: gary_kobinger@phac-aspc.gc.ca
Received Date: August 31, 2011; Accepted Date: October 18, 2011; Published Date: October 20, 2011
Citation: Richardson JS, Wong G, Pillet S, Schindle S, Ennis J, et al. (2011) Evaluation of Different Strategies for Post-Exposure Treatment of Ebola Virus Infection in Rodents. J Bioterr Biodef S1:007. doi: 10.4172/2157-2526.S1-007
Copyright: © 2011 Richardson JS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Bioterrorism & Biodefense
Abstract
Zaire Ebola virus (ZEBOV) is a pathogen that causes severe hemorrhagic fever in humans and non-human
primates. There are currently no licensed vaccines or approved treatments available against ZEBOV infections. The goal of this work was to evaluate different treatment strategies in conjunction with a replication deficient, recombinant human adenovirus serotype 5 (Ad-CAGopt)-based vaccine expressing the Zaire Ebola virus glycoprotein (ZGP) in Ebola infected mice and guinea pigs. Guinea pigs were treated with Ad-CAGoptZGP in combination with different treatment strategies after challenge with guinea pig adapted-ZEBOV (GA-ZEBOV). B10.BR mice were used to further characterize efficacy and immune
responses following co-administration of Ad-CAGoptZGP with the most effective treatment: AdHu5 expressing recombinant IFN-α (hereafter termed DEF201) after challenge with a lethal dose of mouse adapted-ZEBOV (MA-ZEBOV). In mice, DEF201 treatment was able to elicit full protection against a lethal dose of MA-ZEBOV when administered 30 minutes after infection. In guinea pigs the Ad-CAGoptZGP and DEF201 combination therapy elicited full protection when treated 30 minutes post-exposure and were a superior treatment to Ad-CAGoptZGP supplemented with recombinant IFN-α protein. Further analysis of the immune response revealed that addition of DEF201 to Ad-CAGoptZGP enhances the resulting adaptive immune response against ZGP. The results highlight the importance of the innate immune response in the prevention of ZEBOV pathogenesis and support further development of the Ad-CAGoptZGP with DEF201 treatment combination for post-exposure therapy against ZEBOV infection.
Introduction
Ebola virus (EBOV) is a member of the family Filoviridae. They are enveloped, single-stranded, negative-sense RNA viruses, which cause severe hemorrhagic fever and are associated with highly lethal infections in humans. Several strains of EBOV have been identified to date including the Zaire, Sudan, Bundibugyo, Ivory Coast and Reston Ebola virus [1]. The most aggressive strain identified is the Zaire Ebola virus (ZEBOV) with mortality rates reported to be as high as 90% [2]. Outbreaks of EBOV infection have occurred sporadically in Africa in the past and caused substantial fatalities within the affected communities. Several factors including high lethality rates in humans, the ease of in vitro propagation and the potential for aerosol dissemination make EBOV a causative agent for biological warfare [3]. While significant progress has been made in understanding the pathogenesis of EBOV infection there is still no clinically approved EBOV vaccine or treatment available. Thus, the development of an effective post-exposure therapy is considered a high priority despite the limited impact of EBOV on the human population worldwide.
Over the years many candidate vaccine platforms have been evaluated for their efficacy against ZEBOV. These include: naked or lipid encapsulated DNA [4,5], virus-like particle preparations (VLPs) [6-9], Vesicular stomatitis virus, strain Indiana (VSV) [10-14], Human parainfluenza virus 3 (HPIV-3) [15-17], vaccinia [18], Venezuelan equine encephalitis virus (VEEV) and replication-deficient human adenovirus serotype 5 (AdHu5) vectors [4,19]. Among these strategies, the VSV-based ZEBOV vaccine demonstrated 50% survival of NHPs when administered 30 minutes post-ZEBOV infection [10]. In another study, NHPs treated with encapsulated siRNA targeting the ZEBOV RNA polymerase resulted in complete protection when administered 30 minutes after ZEBOV infection followed by additional siRNA administration on days 1 through 6 [20]. It has also been reported that administration of recombinant nematode anticoagulant protein c2 (rNAPc2), a potent inhibitor of tissue factor-initiated blood coagulation, protected 33% of infected rhesus macaques [21].
Macrophages and dendritic cells (DCs) are important components of the innate immune system and known to be the primary early targets for EBOV infection [22]. Upon infection of macrophages with ZEBOV, sustained cytokine and chemokine production was observed but with little or no interferon-alpha (IFN-α) response in vitro [23]. ZEBOV-infected DCs also did not produce IFN-α [24], but contrary to macrophages, infected DCs do not become fully activated and hence do not secrete pro-inflammatory cytokines, upregulate co-stimulatory molecules or properly stimulate T-cells [25]. This lack of stimulation results in a poor adaptive immune response. EBOV infection results in the suppression of a normal stimulation of the host interferon response through VP35 and VP24 viral proteins. VP35 has been shown to block IFN-α/β production by small ubiquitin-like modifier (SUMO)- ylation of interferon regulatory factor 7 (IRF-7) [26] and inhibition of the IRF-3 kinases, namely IKK-ε and TBK-1 [27]. VP24 can interact with host cell importin-α proteins which prevent the nuclear import and accumulation of phosphorylated STAT-1 [28]. Since the STAT-1 transcription factor is utilized by both IFN-α/β and IFN-γ signaling pathways, the presence of VP24 inhibits cellular responses to both Type I and II IFN [28]. As a result the dysregulated innate immune response becomes ineffective at limiting and clearing viral infection, promotes non-productive inflammation as well as negatively impacting the potency of subsequent specific adaptive immune responses. The robust non-specific inflammatory response is suspected to contribute to the progression to shock-like symptoms, coagulation abnormalities and multiple organ failure ultimately causing a fatal outcome to the infected host. Modulating the innate immune system during the early stages of EBOV infection may therefore improve host immune defenses and lead to a more positive outcome. Bolus administration of recombinant interferon was shown to delay EBOV replication in vitro [29] and induce survival in infected mice [30] but this strategy was not successful in NHPs [29]. However, constitutive in situ production of IFN-α via a replication deficient adenovirus has demonstrated strong antiviral efficacy against SARS [31] and Yellow Fever Virus [32].
The present study compares several treatment strategies, some which modulate the innate immune system and investigates whether these treatments are able to enhance survival against a lethal ZEBOV challenge in mice and guinea pigs. The strategies evaluated include: isopropanol, dextrose, azithromycin, CD40 ligand (CD40L), AdHu5- iMYD88.CD40 with the AP1903 dimerization drug, recombinant IFN-α protein (rIFN-α), and an adenovirus expressing recombinant IFN-α (DEF201).
Materials and Methods
Construction and production of adenoviral vectors
Molecular clones of E1-deleted human adenovirus serotype 5 vectors (AdHu5) expressing ZEBOV glycoprotein (ZGP) were generated and called Ad-CAGoptZGP as described previously [42]. The authenticity of each vector was confirmed by sequencing and the recombinant virus was rescued by transfecting the linearized DNA into HEK 293 cells maintained in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 1% penicillin, 1% streptomycin, 1% L-glutamine, 1% sodium pyruvate, and 10% fetal bovine serum. Largescale infections (5 x 108 cells) were initiated from positive transfectants and purified by cesium chloride as previously described [43]. Genome structures of vectors were analyzed by restriction digestions of viral DNA and compared with those of the molecular clones as previously described [43]. Particle number and infectivity (IFU) of vectors were determined by standard optical density and immunodetection of the AdHu5 hexon protein respectively, following infection of HEK 293 cells with limiting dilutions of each vector preparation according to the recommendations by the manufacturer (Adeno-X rapid titer kit, Clontech, Mountain View, CA). Several Ad-CAGoptZGP preparations were generated and quantified for both infectious particle and total particle number. Preparations with a ratio of at least 1:200 infectious to total particle were used in this study. AdHu5 expressing recombinant IFN-α (DEF201) were provided by Defyrus Incorporated, ON and manufactured as described [44].
Animal models, vaccination and challenge
Groups of 5 or 10 B10.BR mice (Jackson Laboratory, ME) were challenged by intraperitoneal (I.P.) injection with 1000 x LD50 of mouse-adapted ZEBOV strain Mayinga [45]. They were then treated by intramuscular (I.M.) injection with 1 x 107 infectious particles of either empty recombinant adenoviral vector diluted to a total of 500μl volume with PBS or DEF201 via the I.M. or I.N. routes 30 minutes post challenge. The mice were then weighed every day for 14 days and monitored for clinical signs of disease for 30 days following challenge.
Hartley breed of guinea pigs (Charles River, QC) were challenged by I.P. injection of 100 x LD50 of guinea pig-adapted ZEBOV strain Mayinga [46]. 30 minutes post challenge they were either treated I.M. with 2 x 108 infectious particles of DEF201, or by I.M. vaccination with 1 x 1010 infectious particles of Ad-CAGoptZGP, with or without treatment of a subcutaneous (S.C) injection of 2g/Kg of isopropanol (6 hours post-challenge), S.C. injection of 5% dextrose solution dissolved in water, S.C. injection of azithromycin (20mg/Kg on day 1, 10mg/Kg on days 2-5 post challenge), mixed I.M. injection of 2 x 1010 infectious particles of AdHu5-iMYD88.CD40, mixed I.M. injection of 0.44μg/Kg rIFN-α, mixed I.M. injection of CD40L, or mixed I.M. injection of 2 x 108 infectious particles of DEF201. Guinea pigs were weighed every day for 16 days and monitored for clinical signs of disease.
All animal procedures and scoring sheets were approved by the Institutional Animal Care Committee at the National Microbiology Laboratory (NML) of the Public Health Agency of Canada (PHAC) according to the guidelines of the Canadian Council on Animal Care. All infectious work was performed in the ‘Biosafety Level 4’ (BSL4) facility at NML, PHAC.
Neutralizing antibody assay
Sera harvested from rodents 28 days post vaccination were inactivated at 56°C for 45 minutes. Twofold serial dilutions of each sample (1:10, 1:20, 1:40, etc, in 50 ml of DMEM) was mixed with equal volume of ZEBOV encoding the eGFP reporter gene (100 transducing units/well) and incubated at 37°C for 60 minutes. The mixture was then transferred onto sub-confluent VeroE6 cells in 96-well flat-bottomed plates and incubated for 90 minutes at 37°C in 5% CO2. Control wells were infected with equal amounts of ZEBOV-eGFP with or without the addition of serum. 100 ml of DMEM supplemented with 20% FBS was then added to each well and plates were incubated at 37°C in 5% CO2 for 48 hr. Dilutions were scored as positive for the presence of NAbs when there was a greater than a 50% reduction in the number of cells expressing eGFP in a field of view using a fluorescent microscope. The highest serum dilution scoring positive for NAb was recorded and neutralization titers were reported as the reciprocal of this dilution. Positive and negative control sera used in this experiment were harvested from mice or guinea pigs 28 days post immunization with a VSV vaccine expressing ZGP, or naïve mice or guinea pig sera respectively. All infectious in vitro work was performed in the biocontainment level 4 laboratory of the NML, PHAC.
ZGP-specific IgG ELISA
Immulon 2 HB 96 well flat bottom MicroTiter ELISA Plates (Thermo Scientific) were coated overnight with 50μl/well of 1 μg/ ml His-ZEBOV-GP capture antigen diluted in PBS [47]. Plates were washed three times with wash buffer (PBS 0.1% TWEEN 20) and then blocked for 90 min with blocking buffer (5% skim milk powder/ PBS/0.2% Tween 20) at 37°C [47]. Plates were washed three times with wash buffer. Sera collected from either mice or guinea pigs were inactivated at 56°C for 45 minutes. Serum was diluted at 1:50 in blocking buffer and 50μl of dilution was added to each well and incubated for 60 min at 37°C. The plates were washed three times with wash buffer. A secondary antibody for mouse (horseradish peroxidase (HRP)-conjugated rat anti-mouse antibody to mouse IgG) (Jackson Laboratories) or for guinea pig (HRP-conjugated goat antiguinea pig antibody to guinea pig IgG), (KPL) or for NHPs (HRPconjugated Goat anti-Human antibody to IgG) (KPL) was added to the plate and then incubated for 60 min at 37°C Horseradish peroxidase substrate (3% hydrogen peroxide solution with ABTS [2,2’-azinobis(3- ethylbenzthiazolinesulfonic acid)]) was then added and incubated at room temperature for 30 min. The plates were read using a VMax Kinetic ELISA Microplate Reader (Molecular Devices) and the data was analyzed using CellMaxPro software for the detection of ZGPspecific IgG antibodies. The data is reported as the optical density measured by absorbance at 405nm. Positive and negative control sera used in this experiment were harvested from mice or guinea pigs 28 days post immunization with a VSV vaccine expressing ZGP, or naïve mice or guinea pig sera respectively.
Flow cytometry analysis
The frequency of CD4+ or CD8+ cells producing IFN-γ TNF-α and IL-2 was assessed by flow cytometry. Mouse splenocytes were isolated day 10 post Ad-CAGoptZGP vaccination by harvesting the spleens and grinding spleen tissues. Splenocytes were seeded at 2 x 106 cells per well in DMEM media supplemented with 10% FBS 1% penicillin, 1% streptomycin, 1% L-glutamine, 1% non-essential amino acids, 1% sodium pyruvate, 1% HEPES buffer, 5 × 10−3 M 2-mecaptoethanol. Cells were stimulated for 5 hours with 5μg/ml of the peptide carrying the immunodominant MHC class I epitope of ZGP (TELRTFSI) for mice with the H-2k haplotype [48] in the presence of 1μl/ml of the protein transport inhibitor GolgiPlug (BD Biosciences). Splenocytes were then stained with PacBlue-conjugated rat anti-mouse CD4 and PerCp-Cy5.5-conjugated rat anti-mouse CD8 antibodies (BD Biosciences), followed by a 20 minute incubation in Cytofix/Cytoperm (BD Biosciences). Intracellular cytokines were detected after staining with PE-conjugated anti-mouse IFN- γ, PECy7-conjugated anti-mouse TNF-α (BD Biosciences), and APC-conjugated anti-mouse IL-2 diluted in PermWash buffer (BD Biosciences). At least 300 000 events were analysed using the 17-color flow cytometer (LSR II Flow Cytometer, BD Biosciences).
Results
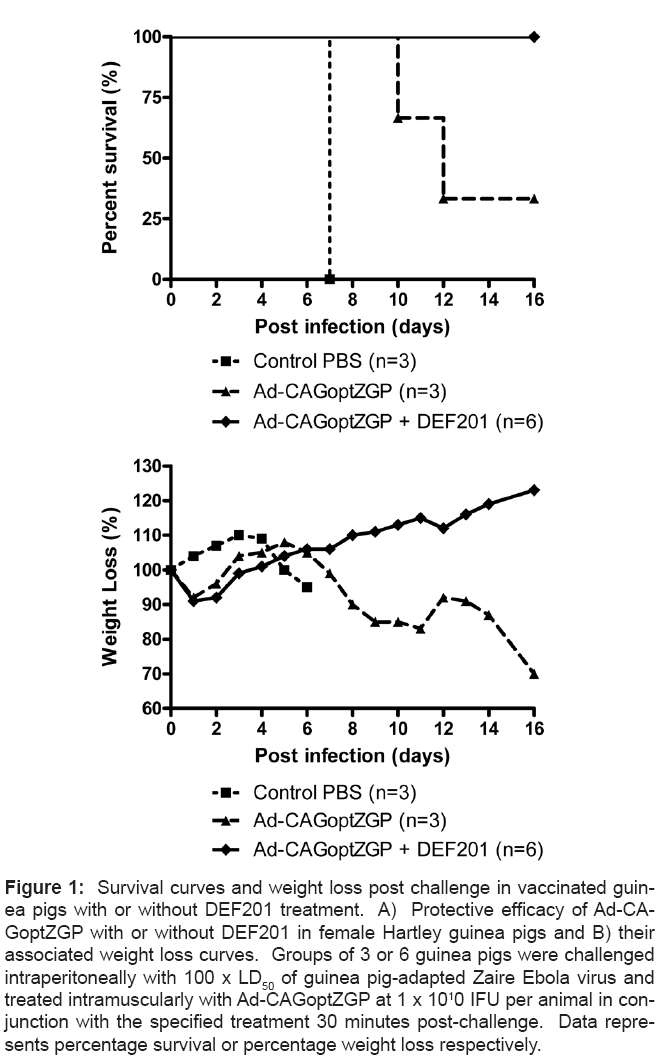
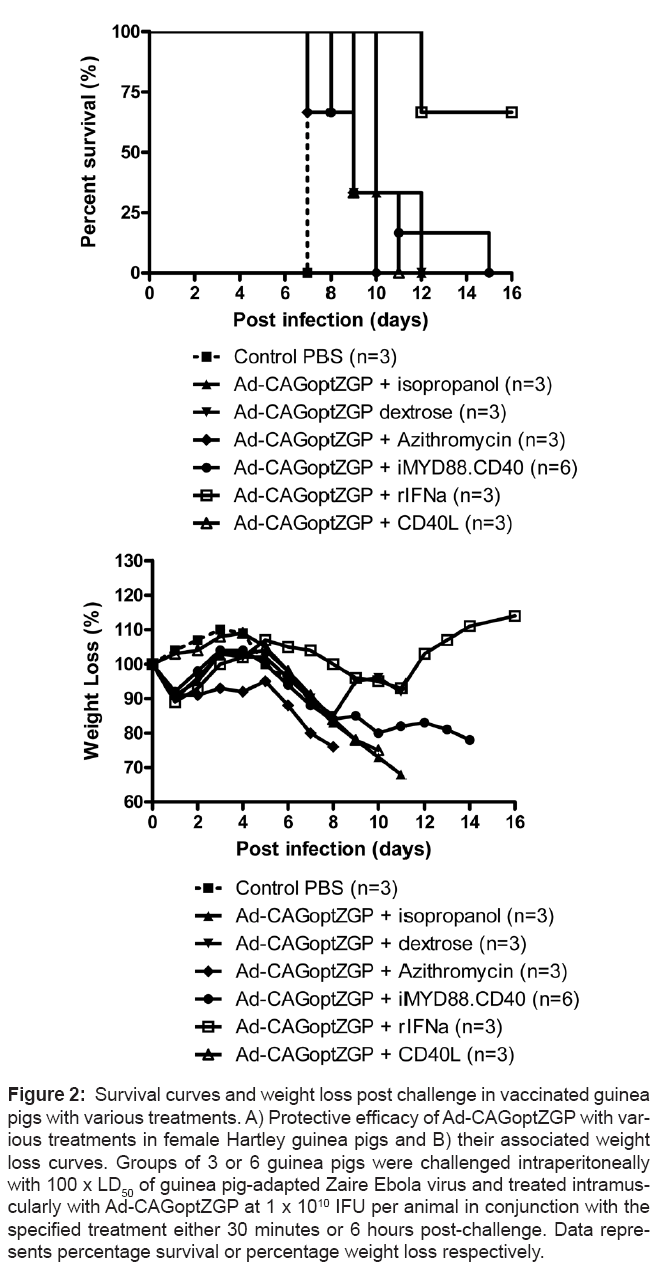
Complete survival was previously observed in mice administered Ad-CAGoptZGP 30 minutes after infection with 1000 x LD50 of MAZEBOV [33]. However, the same strategy resulted in delayed time to death with only 1 survivor out of 3 guinea pigs after challenge with 100 x LD50 of GA-ZEBOV in a pilot experiment (Figures 1A and 1B). In an attempt to improve the survival rate, several treatments were evaluated in guinea pigs when administered 30 minutes after lethal challenge with GA-ZEBOV. Selected strategies hypothesized to improve survival included modulators of the innate immune response; fluids or an antibiotic each evaluated in conjunction with the Ad-CAGoptZGP vaccine. Guinea pigs were first infected with 100 x LD50 of GA-ZEBOV, followed 30 minutes later by a single intramuscular (I.M.) injection of 1 x 1010 infectious forming units (IFU) of Ad-CAGoptZGP per animal in conjunction with either dextrose, AdHu5-iMYD88.CD40 with dimer drug, CD40L, rIFN-α, DEF201 or 6 hours later with isopropanol, or azithromycin from days 1-5 post-challenge. Control guinea pigs were injected I.M. with PBS. Infection of control guinea pigs resulted in rapid weight loss combined with 100% mortality by day 7 post infection. Delays to time of death were observed for the isopropanol treatment (day 12), dextrose (day 12), azithromycin (day 10), AdHu5- iMYD88.CD40 with the dimer drug (day 15) and CD40L (day 11) but survival was not observed for these treatment groups (Figures 2A and 2B). Treatment of guinea pigs with Ad-CAGoptZGP in combination with rIFN-α resulted in 2 of 3 survivors where surviving animals demonstrated moderate clinical symptoms with on average a maximum weight loss of 11% (Figures 2A and 2B). When DEF201 was mixed with the Ad-CAGoptZGP vaccine and injected I.M. into guinea pigs, complete protection (6 survivors out of 6) was observed with little to no weight loss or clinical symptoms (Figures 1A and 1B). Interestingly, treatment with DEF201 alone did not provide protection in guinea pigs against a lethal challenge with GA-ZEBOV (data not shown).
Figure 1: Survival curves and weight loss post challenge in vaccinated guinea pigs with or without DEF201 treatment. A) Protective efficacy of Ad-CAGoptZGP with or without DEF201 in female Hartley guinea pigs and B) their associated weight loss curves. Groups of 3 or 6 guinea pigs were challenged intraperitoneally with 100 x LD50 of guinea pig-adapted Zaire Ebola virus and treated intramuscularly with Ad-CAGoptZGP at 1 x 1010 IFU per animal in conjunction with the specified treatment 30 minutes post-challenge. Data represents percentage survival or percentage weight loss respectively.
Figure 2: Survival curves and weight loss post challenge in vaccinated guinea pigs with various treatments. A) Protective efficacy of Ad-CAGoptZGP with various treatments in female Hartley guinea pigs and B) their associated weight loss curves. Groups of 3 or 6 guinea pigs were challenged intraperitoneally with 100 x LD50 of guinea pig-adapted Zaire Ebola virus and treated intramuscularly with Ad-CAGoptZGP at 1 x 1010 IFU per animal in conjunction with the specified treatment either 30 minutes or 6 hours post-challenge. Data represents percentage survival or percentage weight loss respectively.
Survival and weight loss in mice following Ebola virus challenge and treatment
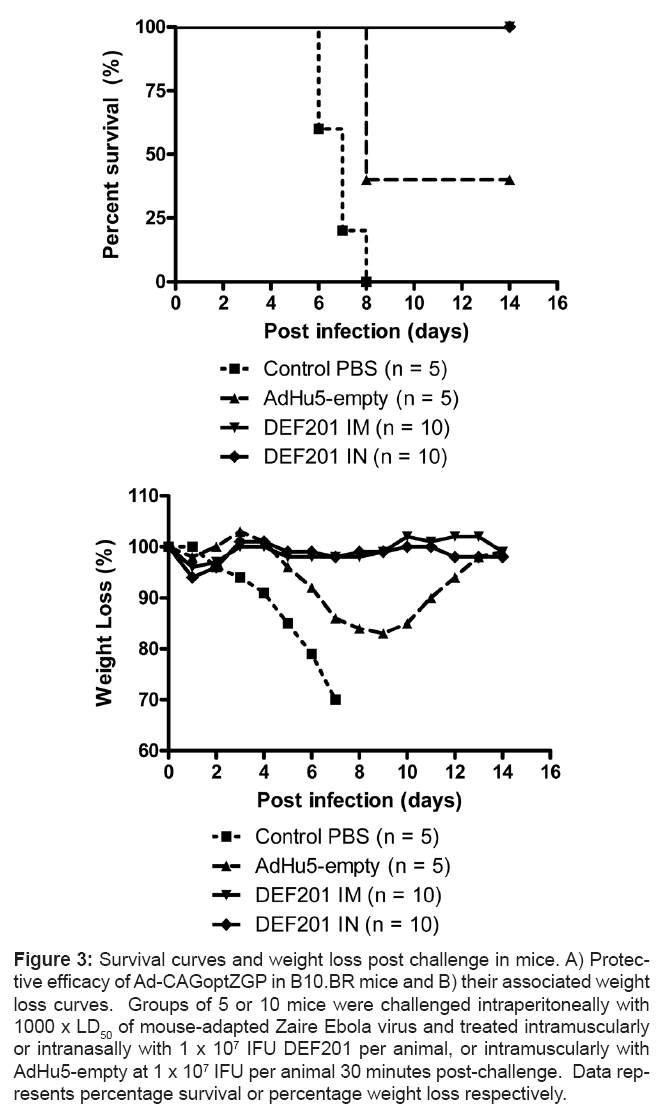
There are currently only limited reagents available for studying the immune response in guinea pigs. Therefore mice were used to better define the additive effect of DEF201, either directly or indirectly, to Ad-CAGoptZGP. Thirty minutes after challenge with 1000 x LD50 of MA-ZEBOV, B10.BR mice were administered with either a single I.M. or intranasal (I.N.) dose of 1 x 107 IFU of DEF201 per animal. Control B10.BR mice were administered PBS. An additional control consisting of mice administered replication-deficient AdHu5 vector not expressing any transgene (AdHu5-empty) I.M. was added to evaluate the contribution the vector alone since AdHu5 particles were shown to modulate the innate immune response [34]. Infection of PBS control mice resulted in rapid weight loss and 100% mortality between days 6 and 8 post-challenge. In contrast, complete survival was observed in MA-ZEBOV challenged mice following treatment with either I.M. or I.N. administration of 1 x 107 IFU of DEF201 with no weight loss or clinical symptoms (Figure 3A). Interestingly, treatment of B10.BR mice with AdHu5-empty at the same dose resulted in 40% survival. Surviving mice displayed signs of illness with an average maximum weight loss of 17% (Figure 3B).
Figure 3: Survival curves and weight loss post challenge in mice. A) Protective efficacy of Ad-CAGoptZGP in B10.BR mice and B) their associated weight loss curves. Groups of 5 or 10 mice were challenged intraperitoneally with 1000 x LD50 of mouse-adapted Zaire Ebola virus and treated intramuscularly or intranasally with 1 x 107 IFU DEF201 per animal, or intramuscularly with AdHu5-empty at 1 x 107 IFU per animal 30 minutes post-challenge. Data represents percentage survival or percentage weight loss respectively.
Immune responses in mice following treatment
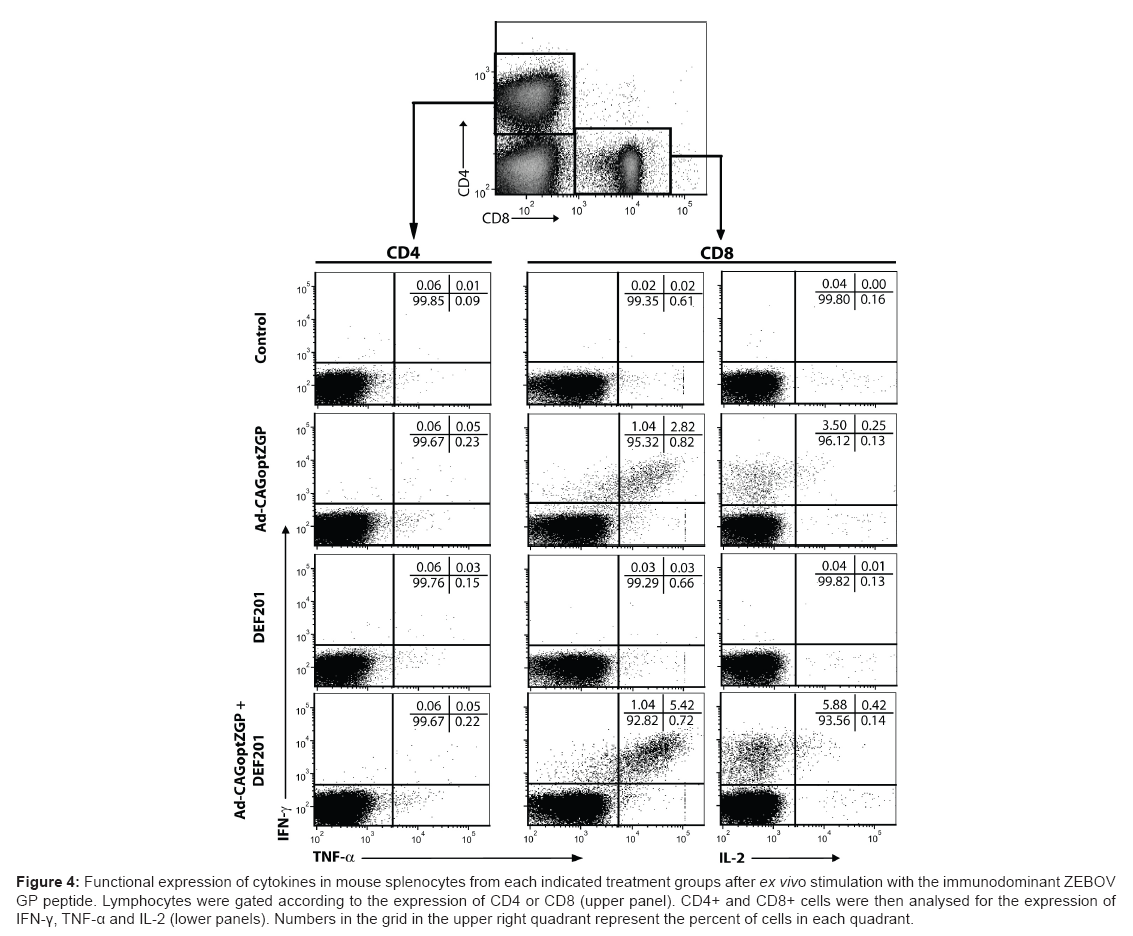
The increased protection observed in guinea pigs with the addition of DEF201 to Ad-CAGoptZGP could be due to an independent antiviral effect from the expression of IFN-α directly on ZEBOV, and/or that IFN-α further improves the adaptive immune response generated by Ad-CAGoptZGP. To address this last possibility, cellular and humoral immune responses were evaluated in the mouse model. The flow cytometry analysis revealed that vaccination with Ad-CAGoptZGP primed a T-cell response characterized by functional CD8+ effector cells producing IFN-γ and TNF-α after restimulation with the immunodominant ZGP peptide, and the absence of these cytokines in CD4+ cells (Figure 4, middle and left panels respectively). A significant amount of those CD8+/IFN-γ/TNF-α+ cells also produced IL-2 (Figure 4, right panel). Co-treatment with DEF201 increased the proportion of the CD8+/IFN-γ+ cells to 5.42% from 2.82% and CD8+/IFN-γ/IL-2+ cells to 0.42% from 0.25% with Ad-CAGoptZGP alone (Figure 4, lower panel). As expected, no ZGP-specific response was observed in cells from mice treated with DEF201 alone.
Figure 4: Functional expression of cytokines in mouse splenocytes from each indicated treatment groups after ex vivo stimulation with the immunodominant ZEBOV GP peptide. Lymphocytes were gated according to the expression of CD4 or CD8 (upper panel). CD4+ and CD8+ cells were then analysed for the expression of IFN-γ, TNF-α and IL-2 (lower panels). Numbers in the grid in the upper right quadrant represent the percent of cells in each quadrant.
The humoral immune response was analyzed on mice serum harvested at 28 days post treatment via total anti-ZGP IgG ELISAs and neutralizing antibody (NAb) assays. Significant levels of total anti-ZGP IgG antibodies were detected for both the Ad-CAGoptZGP with and without DEF201 treatment groups, with corresponding A405 values at 1.31±0.03 and 1.24±0.02 respectively. Background levels of IgG were observed for the DEF201 treatment group with an A405 value of 0.19+0.01 (Figure 5A). Neutralizing assays revealed that sera from DEF201 treated B10.BR mice did not have detectable NAb levels on day 28, where the limit of detection was set at 10 reciprocal dilutions. Significant levels of NAb were detected from sera of mice treated with the Ad-CAGoptZGP with or without DEF201, with average NAb titers of 42±13 or 23±6 reciprocal dilutions respectively on day 28 (Figure 5B).
Figure 5: Humoral immune responses in vaccinated mice with or without DEF201 treatment. A) Serum ZEBOV GP-specific IgG ELISAs. The harvested serum samples were also tested for the presence of IgG antibodies against ZEBOV GP at a 1:50 dilution ratio. The data is reported as the optical density measured by absorbance at 405nm. B) Serum ZEBOV GP-specific neutralizing antibody response. Groups of 3 to 6 mice were vaccinated and treated with or without DEF201, where serum was harvested 28 days post-vaccination. Serum neutralizing antibody levels were reported as the reciprocal of the dilution where greater than 50% viral neutralization was observed.
Humoral immune responses in guinea pigs following treatment
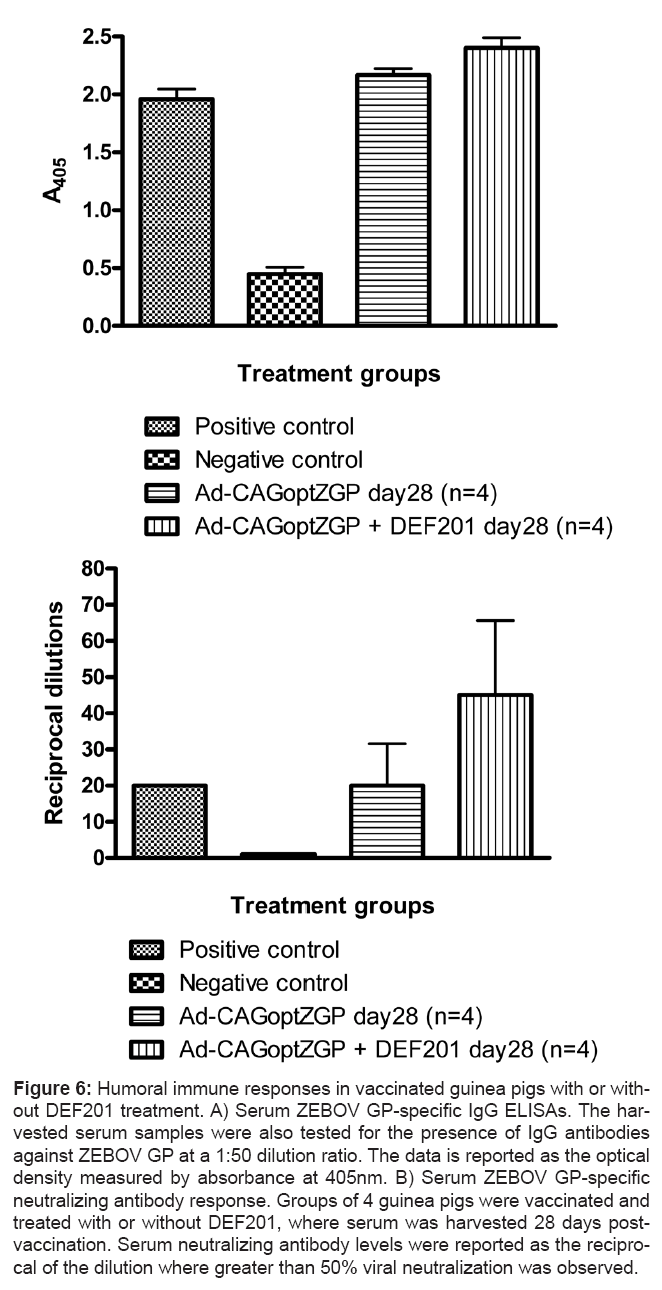
The humoral immune response was also analyzed on guinea pig serum harvested 28 days post vaccination via total anti-ZGP IgG ELISAs and neutralizing antibody (NAb) assays. Significant levels of total anti- ZGP IgG antibodies were detected from sera of animals treated with Ad-CAGoptZGP with or without DEF201, with corresponding A405 values of 2.40±0.09 or 2.17±0.06 respectively (Figure 6A). Similarly, significant levels of NAb were detected in the serum of guinea pigs treated with Ad-CAGoptZGP alone or in combination with DEF201 with corresponding values at 20±12 and 45±21 respectively (Figure 6B).
Figure 6: Humoral immune responses in vaccinated guinea pigs with or without DEF201 treatment. A) Serum ZEBOV GP-specific IgG ELISAs. The harvested serum samples were also tested for the presence of IgG antibodies against ZEBOV GP at a 1:50 dilution ratio. The data is reported as the optical density measured by absorbance at 405nm. B) Serum ZEBOV GP-specific neutralizing antibody response. Groups of 4 guinea pigs were vaccinated and treated with or without DEF201, where serum was harvested 28 days postvaccination. Serum neutralizing antibody levels were reported as the reciprocal of the dilution where greater than 50% viral neutralization was observed.
Discussion
EBOV viruses are among the most deadly infectious agents in humans and it is thought that their virulence is in part due to their capacity to suppress and evade host IFN responses [1]. Consequently, it was hypothesized that productive modulation of the innate immune response with interferon could suppress EBOV replication in vivo sufficiently enough to allow the immune system to mount a protective adaptive response.
Several strategies which modulate the innate immune response were investigated in this study. Isopropanol administration has been shown to have immunosuppressive properties that prevent toxic shock [35], a common suspected occurrence in EBOV human cases. Dextrose administration induces a temporary state of acute hyperglycemia which causes endothelial progenitor cells to adapt a pro-inflammatory phenotype and enhance naïve T-cell activation [36]. Azithromycin is a macrolide antibiotic with the ability to suppress the pro-inflammatory activity of macrophages and is used to treat chronic inflammatory diseases [37]. Since loss of intestinal integrity is common in advanced EBOV infection, it also has the added benefit of preventing the normal intestinal flora from causing further infection after traversing the gastrointestinal barrier. CD40 ligand (CD40L) can partially mimic CD4+ T-cell activation of the CD40 receptor on DCs which aids in the maturation of immature DCs [36]. AdHu5-iMYD88.CD40 treatment in combination with the AP1903 dimerization drug targets the sustained activation of DCs and results in higher antigen-specific CD8+ T-cell responses [36]. IFN-α has been shown to be a clinically effective general immunotherapeutic antiviral in the past, where it is responsible for priming the host innate immune response and then transitioning into an effective adaptive immune response by regulating various cytokines and their receptors [38]. Furthermore, administration of recombinant IFN-α was shown to prevent death in EBOV-infected mice but not in nonhuman primates thus far [29].
Protection against ZEBOV infection was demonstrated in mice following I.M. and I.N. administration with DEF201. Surprisingly partial protection was observed within the AdHu5-empty control group, where 2 of 5 mice survived despite being challenged with a uniformly lethal dose of MA-ZEBOV. This suggests that the AdHu5 vector itself also contributes to the stimulation of a protective immune response against ZEBOV. Indeed, the AdHu5 vector has been shown to promote both transduced and bystander DC maturation as well as stimulate Type I IFN production [39].
While protection was not observed with the isopropanol, dextrose, azithromycin, CD40L, and AdHu5-iMYD88.CD40 treatments on guinea pigs, delays in the occurrence of clinical symptoms and median time to death were observed for all these treatments, suggesting that they participated in delaying ZEBOV-induced pathogenesis. It is possible that further optimization of some of these interventions could lead to better outcome and in turn be useful notably for improving patient management. In all aspects, the present study further support the concept that IFN-α is important early in EBOV infection with regards to survival. This was also a conclusion of previous work, which showed that I.M. administration of IFN-α2β protein into cynomolgus macaques was able to delay viremia and death from lethal ZEBOV infection by several days [29]. Unfortunately, recombinant IFN-α has a short half-life of 8 hours in vivo [40] and can be extremely costly. Effective treatment of EBOV infection may require sustained levels of IFN-α for days in order to increase efficacy and give more time to the adaptive immunity to mount a protective response. DEF201 can produce constitutively high levels of IFN-α for days in a cost efficient manner. In addition to higher and more sustained expression of IFN-α, the AdHu5 particles themselves resulted in improved survival in mice when administered 30 minutes after lethal MA-ZEBOV infection. The addition of DEF201 to the Ad-CAGoptZGP vector resulted in improved survival in comparison to recombinant IFN-α together with Ad-CAGoptZGP. The lack of survival in guinea pigs administered only DEF201 further highlights the enhanced protection of the combination therapy.
Analysis of the resulting T- and B-cell immune response following Ad-CAGoptZGP administration with DEF201 showed overall elevated cellular and humoral responses relative to Ad-CAGoptZGP alone. CD8+ cells primed by the Ad-CAGoptZGP vaccination were functional according to their ability to produce IFN-γ and TNF-α after ex vivo restimulation. The presence of a significant proportion of these cells producing IL-2 is indicative of resting memory T cells [41]. Therefore, DEF201 treatment could contribute to a better clearance of the virus and also promote the establishment of memory cells. However, the positive effect observed with DEF201 alone also indicates that the antiviral state induced by added expression of IFN-α plays a role in controlling or delaying EBOV replication. Interestingly, even only delaying replication is likely to be helpful in providing more time for the generation of a protective immune response. Taken together the results further emphasize the role of IFN-α and the innate immune response in early ZEBOV infection. Future work will need to evaluate the combination of DEF201 with Ad-CAGoptZGP as a treatment to nonhuman primates already infected with a lethal dose of ZEBOV.
Acknowledgements
Financial support was received from the following sources: The Public Health Agency of Canada and the Chemical, Biological, Radiological or Nuclear Research and Technology Initiative (grant #CRTI-06-0218RD and CRTI-09-453TD awarded to G.P.K.). G.W. is the recipient of a Doctoral Research Award from CIHR. The authors would like to thank Heinz Feldmann, Andrea Marzi and Xiangguo Qiu for providing reagents. The authors would also like to thank David Spencer and Maria Croyle for their experimental discussion and input. The authors would also like to thank Geoff Soule, Max Abou, Kaylie Tran, Gregg Schumer, Akeel Baig, Jason Gren and Shane Jones for their technical support.
References
- Basler CF, Amarasinghe GK (2009) Evasion of interferon responses by Ebola and Marburg viruses. J Interferon Cytokine Res 29: 511-520.
- Wilson JA, Bosio CM, Hart MK (2001) Ebola virus: the search for vaccines and treatments. Cell Mol Life Sci 58: 1826-41.
- Geisbert TW, Daddario-Dicaprio KM, Geisbert JB, Reed DS, Feldmann F, et al. (2008) Vesicular stomatitis virus-based vaccines protect nonhuman primates against aerosol challenge with Ebola and Marburg viruses. Vaccine 26: 6894- 6900.
- Hart MK (2003) Vaccine research efforts for filoviruses. Int J Parasitol 33:583- 595.
- Xu L, Sanchez A, Yang Z, Zaki SR, Nabel EG, et al. (1998) Immunization for Ebola virus infection. Nat Med 4: 37-42.
- Swenson DL, Warfield KL, Negley DL, Schmaljohn A, Aman MJ, et al. (2005) Virus-like particles exhibit potential as a pan-filovirus vaccine for both Ebola and Marburg viral infections. Vaccine, 23: 3033-3042.
- Warfield KL, Bosio CM, Welcher BC, Deal EM, Mohamadzadeh M, et al. (2003) Ebola virus-like particles protect from lethal Ebola virus infection. Proc Natl Acad Sci USA, 100: 15889-15994.
- Warfield KL, Olinger G, Deal EM, Swenson DL, Bailey M, et al. (2005) Induction of humoral and CD8+ T cell responses are required for protection against lethal Ebola virus infection. J Immunol 175: 1184-1191.
- Kelly LW, Dana LS, Gene GO, Warren VK, MJ Aman, et al.(2007) Ebola viruslike particle-based vaccine protects nonhuman primates against lethal Ebola virus challenge. J Infect Dis 196 Suppl 2: s430-s437.
- Feldmann H, Jones SM, Daddario-DiCaprio KM, Geisbert JB,Ströher U,et al.(2007) Effective post-exposure treatment of Ebola infection. PLoS Pathog 3: e2.
- Garbutt M, Liebscher R ,Wahl-Jensen V, Jones S, Möller P (2004) Properties of replication-competent vesicular stomatitis virus vectors expressing glycoproteins of filoviruses and arenaviruses. J Virol 78: 5458-5465.
- Geisbert T W, Geisbert JB, Leung A, Daddario-DiCaprio KM, Hensley LE, et al. (2009) Single-injection vaccine protects nonhuman primates against infection with marburg virus and three species of ebola virus. J Virol 83: 7296-7304.
- Jones SM, Feldmann H, Ströher U, Geisbert JB, Fernando L, et al. (2005) Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses. Nat Med 11: 786-790.
- Qiu X, Fernando L, Alimonti JB, Melito PL, Feldmann F, et al. (2009) Mucosal immunization of cynomolgus macaques with the VSVDeltaG/ZEBOVGP vaccine stimulates strong ebola GP-specific immune responses. PLoS One 4: e5547.
- Bukreyev A, Rollin PE, Tate MK, Yang L, Zaki SR, et al. (2007) Successful topical respiratory tract immunization of primates against Ebola virus. J Virol 81: 6379-6388.
- Bukreyev A,Yang L, Zaki SR, Shieh WJ, Rollin PE, et al. (2006) A single intranasal inoculation with a paramyxovirus-vectored vaccine protects guinea pigs against a lethal-dose Ebola virus challenge. J Virol 80: 2267-2279.
- Yang L, Sanchez A, Ward JM, Murphy BR, Collins PL, et al. (2008) A paramyxovirus-vectored intranasal vaccine against Ebola virus is immunogenic in vector-immune animals. Virology 377: 255-264.
- Geisbert T W,Pushko P, Anderson K, Smith J, Davis KJ,et al. (2002) Evaluation in nonhuman primates of vaccines against Ebola virus. Emerg Infect Dis 8: 503-507.
- Geisbert T W,P B Jahrling (2003) Towards a vaccine against Ebola virus. Expert Rev Vaccines 2:777-789.
- Geisbert T W, Lee AC, Robbins M, Geisbert JB, Honko AN, et al. (2010) Postexposure protection of non-human primates against a lethal Ebola virus challenge with RNA interference: a proof-of-concept study. Lancet 375: 1896- 1905.
- Geisbert T W, Hensley LE, Jahrling PB, Larsen T, Geisbert JB, et al.(2003) Treatment of Ebola virus infection with a recombinant inhibitor of factor VIIa/ tissue factor: a study in rhesus monkeys. Lancet 362: 1953-1958.
- Bray M, T W Geisbert (2005) Ebola virus: the role of macrophages and dendritic cells in the pathogenesis of Ebola hemorrhagic fever. Int J Biochem Cell Biol 37: 1560-1566.
- Gupta M., Mahanty S, Ahmed R, Rollin PE (2001) Monocyte-derived human macrophages and peripheral blood mononuclear cells infected with ebola virus secrete MIP-1alpha and TNF-alpha and inhibit poly-IC-induced IFN-alpha in vitro. Virology 284: 20-25.
- Bosio C M, Aman MJ, Grogan C, Hogan R, Ruthel G, et al. (2003) Ebola and Marburg viruses replicate in monocyte-derived dendritic cells without inducing the production of cytokines and full maturation. J Infect Dis 188: 1630-1638.
- Mahanty S, Hutchinson K, Agarwal S, McRae M, Rollin PE, et al. (2003) Cutting edge: impairment of dendritic cells and adaptive immunity by Ebola and Lassa viruses. J Immunol 170: 2797-2801.
- Chang T H, Kubota T, Matsuoka M, Jones S, Bradfute SB, et al. (2009) Ebola Zaire virus blocks type I interferon production by exploiting the host SUMO modification machinery. PLoS Pathog 5: e1000493.
- Prins K C, W B Cardenas, C F Basler (2009) Ebola virus protein VP35 impairs the function of interferon regulatory factor-activating kinases IKKepsilon and TBK-1. J Virol 83: 3069-3077.
- Reid S P. Leung LW, Hartman AL, Martinez O, Shaw ML, et al. (2006) Ebola virus VP24 binds karyopherin alpha1 and blocks STAT1 nuclear accumulation. J Virol 80: 5156-5167.
- Jahrling P B. Geisbert TW, Geisbert JB, Swearengen JR, Bray M, et al. (1999) Evaluation of immune globulin and recombinant interferon-alpha2b for treatment of experimental Ebola virus infections. J Infect Dis 179: 224-234.
- Bray M, J Driscoll, J W Huggins (2000) Treatment of lethal Ebola virus infection in mice with a single dose of an S-adenosyl-L-homocysteine hydrolase inhibitor. Antiviral Res 45: 135-147.
- Kumaki Y, Ennis J, Rahbar R, Turner JD, Wandersee MK, et al. (2011) Singledose intranasal administration with mDEF201 (adenovirus vectored mouse interferon-alpha) confers protection from mortality in a lethal SARS-CoV BALB/c mouse model. Antiviral Res 89: 75-82.
- Julander J G, Ennis J, Turner J, Morrey JD( 2011) Treatment of yellow fever virus with an adenovirus-vectored interferon, DEF201, in a hamster model. Antimicrob Agents Chemother 55: 2067-2073.
- Richardson J S, Yao MK, Tran KN, Croyle MA, Strong JE, et al. (2009) Enhanced protection against Ebola virus mediated by an improved adenovirusbased vaccine. PLoS One 4: e5308.
- Tatsis N H C Ertl (2004) Adenoviruses as vaccine vectors. Mol Ther 10: 616- 629.
- Desy O, Carignan D, Caruso M, de Campos-Lima PO (2008) Immunosuppressive effect of isopropanol: down-regulation of cytokine production results from the alteration of discrete transcriptional pathways in activated lymphocytes. J Immunol 181: 2348-2355.
- Loomans C J, van Haperen R, Duijs JM, Verseyden C, de Crom R, et al. (2009) Differentiation of bone marrow-derived endothelial progenitor cells is shifted into a proinflammatory phenotype by hyperglycemia. Mol Med 15: 152-159.
- Yamauchi K, Shibata Y, Kimura T, Abe S, Inoue S, et al. (2009) Azithromycin suppresses interleukin-12p40 expression in lipopolysaccharide and interferongamma stimulated macrophages. Int J Biol Sci 5: 667-678.
- Brassard D L, M J Grace, Bordens RW (2002) Interferon-alpha as an immunotherapeutic protein. J Leukoc Biol 71: 565-581.
- Hensley S E, Giles-Davis W, McCoy KC, Weninger W, Ertl HC (2005) Dendritic cell maturation, but not CD8+ T cell induction, is dependent on type I IFN signaling during vaccination with adenovirus vectors. J Immunol 175: 6032- 6041.
- Reddy K R, Wright TL, Pockros PJ, Shiffman M, Everson G, et al. (2001) Efficacy and safety of pegylated (40-kd) interferon alpha-2a compared with interferon alpha-2a in noncirrhotic patients with chronic hepatitis C. Hepatology 33: 433-438.
- Mueller S N,Langley WA, Carnero E, García-Sastre A, Ahmed R (2010) Immunization with live attenuated influenza viruses that express altered NS1 proteins results in potent and protective memory CD8+ T-cell responses. J Virol 84: 1847-1855.
- Gao G, Zhou X, Alvira MR, Tran P, Marsh J, et al. (2003) High throughput creation of recombinant adenovirus vectors by direct cloning, green-white selection and I-Sce I-mediated rescue of circular adenovirus plasmids in 293 cells. Gene Ther 10: 1926-1930.
- Kobinger G P, Feldmann H, Zhi Y, Schumer G, Gao G, et al. (2006) Chimpanzee adenovirus vaccine protects against Zaire Ebola virus. Virology 346: 394-401.
- Wu J Q, Barabé ND, Huang YM, Rayner GA, Christopher ME, et al. (2007) Preand post-exposure protection against Western equine encephalitis virus after single inoculation with adenovirus vector expressing interferon alpha. Virology 369: 206-213.
- Bray M, Davis K, Geisbert T, Schmaljohn C, Huggins J (1998) A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J Infect Dis 178: 651-661.
- Connolly B M, Steele KE, Davis KJ, Geisbert TW, Kell WM, et al. (1999) Pathogenesis of experimental Ebola virus infection in guinea pigs. J Infect Dis 179: 203-217.
- Nakayama E, Yokoyama A, Miyamoto H, Igarashi M, Kishida N, et al. (2010) Enzyme-linked immunosorbent assay for the detection of filovirus speciesspecific antibodies. Clin Vaccine Immunol 17: 1723-1728.
- Rao M, Matyas GR, Grieder F, Anderson K, Jahrling PB, et al. (1999) Cytotoxic T lymphocytes to Ebola Zaire virus are induced in mice by immunization with liposomes containing lipid A. Vaccine 17: 2991-2998.
Relevant Topics
- Anthrax Bioterrorism
- Bio surveilliance
- Biodefense
- Biohazards
- Biological Preparedness
- Biological Warfare
- Biological weapons
- Biorisk
- Bioterrorism
- Bioterrorism Agents
- Biothreat Agents
- Disease surveillance
- Emerging infectious disease
- Epidemiology of Breast Cancer
- Information Security
- Mass Prophylaxis
- Nuclear Terrorism
- Probabilistic risk assessment
- United States biological defense program
- Vaccines
Recommended Journals
Article Tools
Article Usage
- Total views: 14189
- [From(publication date):
specialissue-2011 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 9585
- PDF downloads : 4604