Case Report Open Access
Enteral Nutrition Support in Patients with Pyloric Obstruction
Yuanfan Yang1,2, Jianchun Yu2*, Weiming Kang2, and Yan Li2
1Peking Union Medical College, Beijing, China
2Department of General Surgery, Peking Union Medical College Hospital, Beijing, China
- *Corresponding Author:
- Jianchun Yu
Professor, Department of General Surgery
Peking Union Medical College Hospital
Beijing, 100005, China
E-mail: yu-jch@163.com
Received date: August 08, 2013; Accepted date: September 11, 2013; Published date: September 13, 2013
Citation: Yang Y, Yu J, Kang W, Li Y (2013) Enteral Nutrition Support in Patients with Pyloric Obstruction. J Gastroint Dig Syst 3:136. doi:10.4172/2161-069X.1000136
Copyright: © 2013 Yang Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Pyloric obstruction is a common clinical diagnosis in Asian countries because there is a higher incidence of gastric cancer in the population. Patients, especially in rural areas, present to hospital late when gastric outlet obstruction has become so severe that oral feeding is almost impossible. Each hospital has developed its own method of feeding to provide nutritional support for these patients before pyloric obstruction is relieved, usually by surgery. Until recently, most hospitals use parenteral nutrition (PN), which requires less effort in setting access route. However both ESPEN and the Chinese guideline would recommend post pyloric enteral nutrition (EN) for patients with a partially functional GI tract, as EN has been demonstrated to be safer, cheaper and associated with less metabolic complications. Setting a safe and convenient route for post-pyloric feeding requires a more dedicated team and solid protocol. Here we report the EN support for 3 patients with pyloric obstruction in June 2013, utilizing the combination nasogastric decompression-nasojejunal feeding tube system. An additional paragraph is given to nutrition evaluation, nursing care of the feeding system, and trouble shooting.
Keywords
Pyloric obstruction; Gastric outlet obstruction; Nutrition; Post pyloric feeding; Tri-lumen feeding tube; Combination nasogastric decompression-nasojejunal feeding tube
Introduction
Pyloric obstruction, often caused by an underlying organic lesion near the gastric outlet, is a common clinical diagnosis based on its typical history, imaging and endoscopic findings. Patients usually present with progressive nausea, vomiting of residual food, abdominal distension and sometimes abdominal pain. Besides these direct results of pyloric obstruction, prolonged GI disorder often results in reduced intake of food and rapid weight loss. Although extensive diagnostic and therapeutic efforts, mainly various surgical options, have been explored to establish definitive diagnosis and relieve obstruction, less attention is paid to the perioperative nutrition evaluation and support for these patients. It has been demonstrated that improving the nutritional status of these patients will lead to better surgical outcome [1]. While until recently, most hospitals would still directly initiate PN for these patients for ease of setting access route, even though it is more expensive and associated with higher risk of infection and metabolic complications. Choosing between PN and EN has become particularly important when a clear pathological diagnosis is hard to reach and patients require nutritional support for weeks while waiting for a series of gastroscopy to find evidence or exclude the possibility of malignancy. Proper EN support can safely and conveniently improve the nutritional status of these patients while better prepares them for later surgical procedures.
Here we report a case series at our ward in June 2013, to illustrate our experience offering post pyloric enteral nutrition support through a tri-lumen feeding tube in pyloric obstruction patients, with particular emphasis on the nutrition evaluation, application of enteral nutrition formula and complication managements.
Case 1
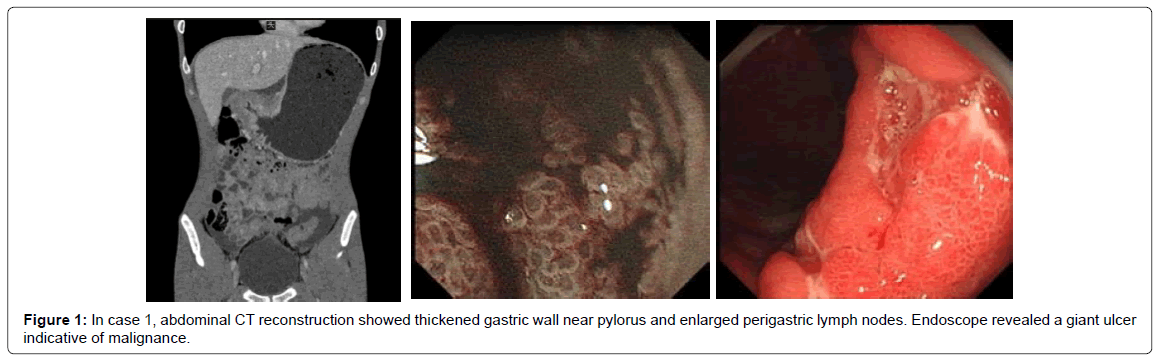
A 19 year old young man began with intermittent regurgitation 4 month ago and later developed progressive abdominal distension, vomiting of residual food after a big meal. Symptoms becomes so severe in the recent one month that he had nausea and vomiting up to twice a day, felt not like eating any solid food, passed stool only once a week. An upper gastrointestinal double contrast radiograph revealed a mass lesion in the pyloric lumen, and subsequent GI endoscopic biopsy confirmed the diagnosis of signet-ring cell carcinoma. During this period, he could have only one liquid meal a day, losing 11 kg in 3 months. On admission to hospital, he was 44 kg, with a BMI of 15.2 kg/m2 and a mid-arm circumference of 21 cm. He was not as alert as before and his gait was unsteady when walking. We decompressed the stomach with gastric tube and orally gave 500 ml of EN solution, but 6 hours later we removed almost the same amount of fluid from gastric tube, revealing a near complete obstruction of pylorus. A trilumen nasogastric decompression-jejunal feeding tube was then placed under fluoroscope so that PN was switched to EN. He experienced one episode of hypoglycemia when he tried to increase the infusion rate himself. Nasal mucosal ulceration and sinusitis also occurred in the young man but resolved spontaneously in 3 days. EN through the tube has supported him for 3 months during neo-adjuvant chemotherapy through a PICC line. In the first 2 weeks a caloric goal of 1500 kCal/d (34 kcal/kg·d) was given but there is no weight gain. The caloric goal was then set to 2000 kcal/d (44 kcal/kg·d) and patient gained 2 kg in 2 weeks. CA 19-9 level was steady, 181~191 U/ml after diagnosis. GI discomfort induced by chemotherapy didn’t affect jejunum feeding and the patient is scheduled for surgery after full course of preoperative chemotherapy (Figure 1).
Case 2
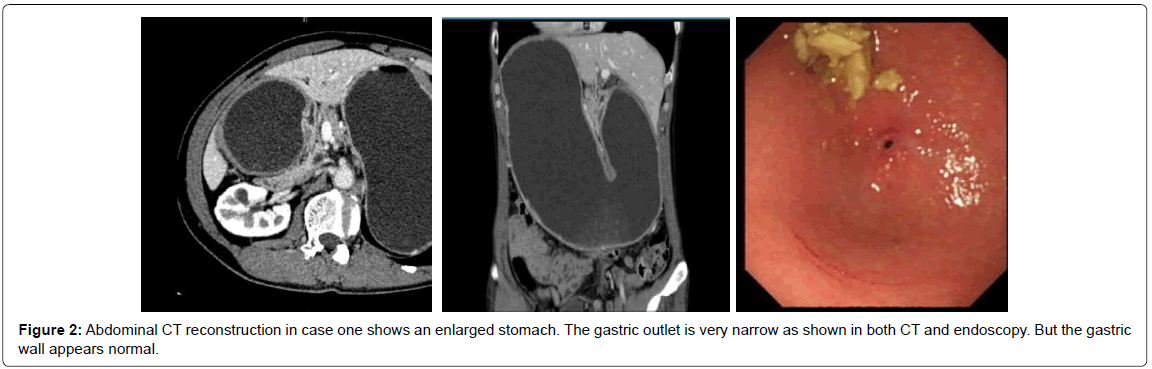
A 53 year old bus driver, with a history of chronic gastric ulcer for 20 years, came to the hospital complaining of aggravating upper abdominal pain, regurgitation, nausea and vomiting beginning from half a year ago. He underwent 5 consecutive gastric endoscopies in 6 months which showed partial pyloric obstruction, and gastric retention. Endoscopic biopsy revealed only chronic inflammation. With partial parenteral nutrition and very limited liquid food, his weight still decreases from 60 kg to 48 kg in 5 month, with a BMI of 16.1 kg/m2 on admission. After admission, a tri-lumen feeding tube was placed under fluoroscope and PN was switched to EN. Patient experienced nasal discomfort and nausea, which resolved in 5 days. A caloric goal of 30 kcal/kg·d was gradually reached in 3 days. The patient gained 2 kg after 3 weeks when stenosis partially resolved spontaneously and patient was given partial oral liquid diet for 1 week before surgery. After one month of EN, his general condition was improved, and his pre albumin level increased from 220 mg/L to 287 mg/L in the first 2 weeks before operation and was kept steady. 1 month later, the patient went through subtotal gastrectomy with Roux-en-Y anastomosis during which a jejunostomy tube was placed to provide early postoperative EN. He had an uneventful postoperative recovery (Figure 2).
Discussion
Clinical algorithm to initiate EN
Most patients with prolonged pyloric obstruction will develop nutrition impairment. Proper identification and subsequent nutritional support are relevant to the surgical outcome: reducing complications of disease and treatment, accelerating postoperative recovery and improving general condition of the patient. Patients with a NRS 2002 score ≥ 3, which is usually the case, are nutritionally at risk and nutritional support should be initiated according to the ESPEN guideline for nutrition screen. EN is only contraindicated in fully or partially dysfunction GI tract. While in pyloric obstruction patients, the whole GI tract distal to pylorus is structurally and functionally normal and EN should be initiated as a more physiological feeding pathway unless surgery is scheduled in a week. Patients usually could not use the oral route for EN support as a result of the GI obstruction. In this case, EN should be supplied distal to the pylorus, usually 40 cm past the Treitz ligament to prevent fluid reflux. This can be done permanently through jejunostomy, or temporarily through naso-jejunal feeding tube. For patients with pyloric obstruction that cannot resolve after conservative therapy, or in the case of gastric cancer undergoing neoadjuvant therapy, a definitive surgery is usually scheduled later on. So a temporal naso-jejunal feeding route is appropriate and could be removed when possible. This step is technically demanding and somewhat hinders the wide-spread application of EN in such patients. For medical centers with high patient volume, endoscopy assisted tube placement is now giving way to fluoroscope, which is more convenient and less expensive. Then we evaluate whether the energy needs could be met and optimize the nutritional plan. With proper pre-and postoperative nutrition therapy combined, improved quality of life could be achieved in long term follow up of surgical patients [2].
Common problem neglected
Gastric outlet obstruction is a common finding in general surgical departments in China and some other Asian countries, partly because of significantly higher prevalence of gastric cancer in the Chinese population than in Caucasians. It is particularly important in rural areas of China, as patients usually present to hospital late due to limited availability of medical care. These patients, besides symptoms directly related to GI obstruction, usually have severe weight loss, impaired nutritional status, dehydration, and sometimes electrolyte disturbance.
It has been demonstrated early that weight loss greater than 20% is associated with increased operative complication and mortality in gastric ulcer patients [1]. Later work reinforced the association between malnutrition and poor surgical outcome [3,4]. However, little attention is paid to signs and symptoms of nutritional inadequacies or imbalances when physicians are too focused on reaching a pathological diagnosis and surgical treatment to relieve obstruction.
Nutrition evaluation
To provide adequate nutrition support for these patients with a suspected pyloric obstruction, a thorough nutrition evaluation should be given on admission. This includes a detailed history of GI symptoms, change in body weight and eating habits, as well as basic numerical measurements like BMI (Body Mass Index), triceps skin fold thickness, mid-arm muscle circumference (MAMC), etc. Studies have also show that biochemical parameters as serum albumin, pre-albumin, and transferrin could be used to evaluate and monitor long-term and ongoing nutritional status of critically ill patients [4].
The NRS2002 Nutritional Risk Screening is a standard tool for evaluation and documentation of nutritional status [5]. Patients with severe pyloric obstruction could easily be identified in initial screening with their typical low BMI, recent weight loss and difficulty in eating. Both the two cases we encountered had severe weight loss with BMI<18.5 kg/m2, which reveals high nutritional risk and prompts immediate nutrition support.
EN is preferred for pyloric obstruction
There are two major routes, by either enteral nutrition (EN) or parenteral nutrition (PN) to temporarily support these patients. And in the case of pyloric obstruction, enteral nutrition can only be given distal to the pylorus, through temporarily placed nasoduodenal or nasojejunal tubes, or rarely through long-term percutaneous endoscopic jejuostomy (PEJ).
In the past, each medical center developed its own protocol of feeding for patients with gastric outlet obstruction, based on clinical experience, availability of feeding equipment and support from nursing team as well as nutrition departments. For convenience of administration and nursing care, some secondary and primary care facilities in China are using PN support before a definitive or palliative surgery is offered to relieve the pyloric obstruction.
However, both current Western and Chinese guidelines have emphasized the importance of EN in patients with even partly functional GI tract. It is a more physiological method of nutrition, which helps maintain intestinal microbiota, nourishing mucosal associated lymphoid tissue (MALT), in addition to supplying basic caloric needs. EN is associated with less infectious and metabolic complications [6], and a summary of clinical experience with double lumen nasogastric decompression-jejunal feeding (NGJ) in 50 gastric outlet obstruction patients have shown effective outcome, and 98% patients tolerated the nasally inserted feeding tube [7].
Tri-lumen feeding tube system
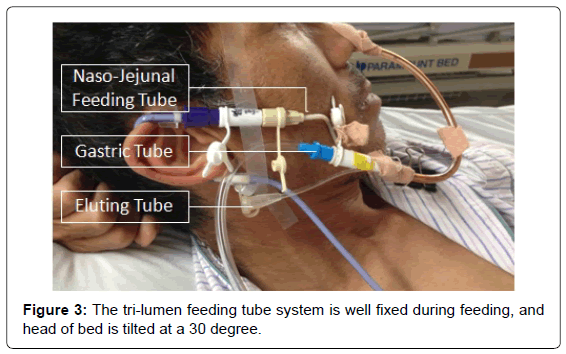
We have been using a tri-lumen feeding system since 5 years ago and had reasonably well experience in placement and management of the system. It is a combination nasogastric decompression-jejunal balloon feeding tube made of relatively soft silicon rubber. The device consists of a naso-gastric decompression tube, a naso-jejunum tube within the lumen of the gastric tube for post pyloric feeding, and a thin tube to inflate a balloon at gastric cardia, which prevents dislocation of the tube. The gastric decompression tube helps drain gastric secretions, thus reducing risk of vomiting or aspiration. Gastric juice can also be collected through the gastric tube and then re-administered into jejunal feeding tube, therefore maintaining fluid and electrolyte balance (Figure 3).
After excluding absolute contraindications for post pyloric enteral feeding (including bowel obstruction, perforation or leakage, etc.), the tube is placed under fluoroscopy with a guide wire. This is done fluently under X-ray without sedation, usually within 10 minutes. It should be noticed that in pancreatitis patients with pseudocyst formation that cause pyloric obstruction, a barium meal under fluoroscopy may reveal inflammatory stricture or internal fistula of the intestine. A surgical approach has to be considered in this situation [8].
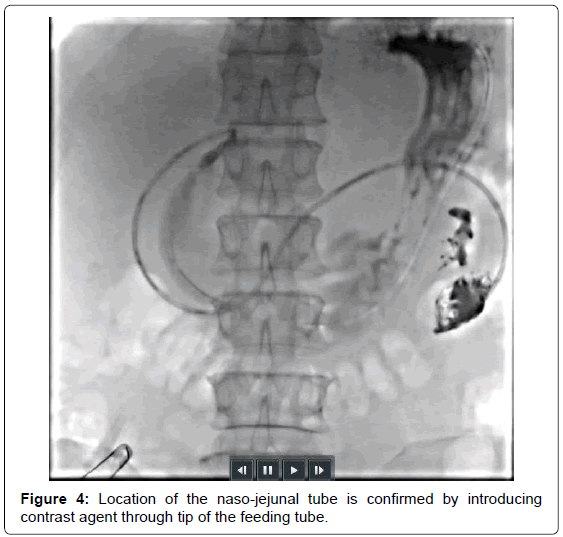
The tip of the naso-jejunal feeding tube is placed 40 cm past the ligament of Treitz, which is confirmed under fluoroscopy (Figure 4). This is the essential distance to prevent stimulation of pancreatic secretion as in intra-duodenal feeding. However, Naso-duodenal tube is too short to achieve pancreatic rest, with higher risk of recoiling back, displacement and aspiration [9]. As a result, jejunal feeding has become widely accepted for pyloric obstruction patients. Its difference compared with PN is shown in Table 1.
| Difference between EN (through tri-lumen tube system) and PN for pyloric obstruction | ||
|---|---|---|
| Tri-Lumen tube system | Parenteral Nutrition | |
| Access Route | fluoroscope (rarely endoscope) | usually through PICC, X-ray film confirm |
| Costs | Equipment cost $120, Daily Nutrition cost $30/day |
Equipment cost $200, Daily Nutrition cost $130/day |
| Physiology | More physiological, maintains GI mucosal integrity, less metabolic disturbance | Not physiological, nutritional imbalance, liver function impairment |
| Feeding Mode | Continues in the beginningàintermittentàbolus | Intermittent |
| Complications | Less complication but physically discomfort | More metabolic and infectious complications |
| Nursing Efforts | More effort dealing with mechanical complications, prevent clogging of the tube | Less nursing efforts. Higher requirement on preparing the IV formula. |
| Home feeding | Likely after self-learning | Very hard |
| Liver toxicity | Low | High if long term |
Table 1: Difference between EN (through tri-lumen tube system) and PN for pyloric obstruction. The naso-jejunal feeding is more physiological, cheaper and safer, but requires a longer learning curve.
Tube feeding and trouble shooting
After successfully placing the tube, enteral nutrition is given slowly at 20 ml/h on the first day. Intact protein formula is appropriate because the digestive tract distal to pylorus is fully functional. It should be noticed that rapid replenish of nutrition in severely malnourished patients should be avoided to prevent metabolic disturbance like re-feeding syndrome or dumping syndrome [10]. Like in our first case, the boy experienced episodes of hypoglycemia presented as weakness of the limb and sweating when he tried to adjust the infusion rate to 80 ml/h himself. He is concerned of this because the long duration of pump feeding prevents him from a social life. Both patients and the nursing team must fully understand that infusion rate has to be increased gradually, usually 20 ml/h higher than the previous day, to reach the desired caloric goal between 20-30 kcal/kg·d for severely malnourished patients.
To achieve standard nursing care for the post pyloric feeding system, continuing medical education programs must be offered to all ward staff. We have set the following, but not limited to, as standard operating procedure.
The tube for pumping nutrition must be replaced at least once every 24 hours, since jejunal nutrition must be sterile to prevent enteric flora disturbance. Infusion rate and nutrition osmolarity must be low in the beginning and gradually progress. The tube should be fixed my tape as shown in Figure 1 to prevent dislocation. It must be flushed with 10 ml saline every 4-6 h, as well as before and after nutrition infusion. Gastric residue should be checked every 8h to prevent aspiration. Liquid drug could be administered independently through the feeding tube, and the tube was flushed by 10-15 ml saline to prevent clogging.
Funding Source
Beijing Natural Science Foundation on Clinical Medicine, Grant 713209.
References
- McClave SA, Greene LM, Snider HL, Makk LJ, Cheadle WG, et al. (1997) Comparison of the safety of early enteral vs parenteral nutrition in mild acute pancreatitis. JPEN J Parenter Enteral Nutr 21: 14-20.
- Meng QB, Yu JC, Kang WM, Ma ZQ, Ye X, et al. (2013) Effect of enteral nutrition via jejunostomy catheter on quality of life in gastric cancer patients who have undergone gastrectomy. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 35: 332-336.
- Studley HO (2001) Percentage of weight loss: a basic indicator of surgical risk in patients with chronic peptic ulcer. 1936. Nutr Hosp 16: 141-143.
- Rhoads JE, Alexander CE (1955) Nutritional problems of surgical patients. Ann N Y Acad Sci 63: 268-275.
- Mullen JL, Gertner MH, Buzby GP, Goodhart GL, Rosato EF (1979) Implications of malnutrition in the surgical patient. Arch Surg 114: 121-125.
- Kondrup J, Allison SP, Elia M, Vellas B, Plauth M (2002) Educational and Clinical Practice Committee, et al. (2003) ESPEN guidelines for nutrition screening 2002. Clin Nutr 22: 415-421.
- McClave SA, Chang WK, Dhaliwal R, Heyland DK (2006) Nutrition support in acute pancreatitis: a systematic review of the literature. JPEN J Parenter Enteral Nutr 30: 143-156.
- O'Keefe S, Rolniak S, Raina A, Graham T, Hegazi R, et al. (2012) Enteral feeding patients with gastric outlet obstruction. Nutr Clin Pract 27: 76-81.
- Rombeau JL (1986) Enteral feeding into the jejunum with combined gastric decompression. Nutrition in clinical practice 1: 205-208.
- Ledeboer M, Masclee AA, Biemond I, Lamers CB (1998) Effect of intragastric or intraduodenal administration of a polymeric diet on gallbladder motility, small-bowel transit time, and hormone release. Am J Gastroenterol 93: 2089-2096.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 18454
- [From(publication date):
October-2013 - Dec 19, 2025] - Breakdown by view type
- HTML page views : 13623
- PDF downloads : 4831