Special Issue Article Open Access
Clinical Malaria and Nutritional Status in Children Admitted in Lwiro Hospital, Democratic Republic of Congo
Mitangala Ndeba Prudence1,5*, Umberto D’Alessandro2, Philippe Donnen3,5, Philippe Hennart3,5, Denis Porignon4, Bisimwa Balaluka Ghislain5,6, Zozo Nyarukweba Déogratias6 and Michèle Dramaix Wilmet1,51Département de biostatistique, Ecole de Santé Publique, Université Libre de Bruxelles (Belgique)
2Department of Parasitology, Institute Tropical Medicine, Antwerp, Belgium
3Département d’épidémiologie et médecine préventive, Ecole de santé Publique, Université Libre de Bruxelles (Belgique).
4Unité de santé internationale, Département des Sciences de la Santé Publique, Université de Liège (Belgique)
5Centre Scientifique et Médical de l’Université Libre de Bruxelles pour ses Activités de Coopération (CEMUBAC)
6Département de nutrition, Centre de Recherche en Sciences Naturelles / Lwiro (République Démocratique du Congo)
- *Corresponding Author:
- Mitangala Ndeba Prudence
département de biostatistique ESP/ULB, CP 598
Route de Lennik 808, 1070 Bruxelles, Belgique
Tel: +243 998 088 072
E-mail: prudendeb@yahoo.fr
Received Date: December 13, 2011; Accepted Date: April 20, 2012; Published Date: April 24, 2012
Citation: Prudence MN, D’Alessandro U, Donnen P, Hennart P, Porignon D, et al. (2012) Clinical Malaria and Nutritional Status in Children Admitted in Lwiro Hospital, Democratic Republic of Congo. J Clin Exp Pathol S3:004. doi: 10.4172/2161-0681.S3-004
Copyright: © 2012 Prudence MN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Clinical & Experimental Pathology
Abstract
Abstract
Background: The relationship between malaria and nutritional status is still unclear and difficult to establish.
Methods: For this purpose, information on 1 994 children admitted between January 2003 and November 2006
in Lwiro paediatric hospital, located in the Kivu region in the east of the Democratic Republic of Congo (RDC), was
analyzed. The relationship between indicators of Protein Energy Malnutrition (PEM) on admission and the risk of
clinical malaria during hospitalization was determined using Poisson regression.
Results: The clinical malaria incidence during hospitalization was 7.65/1 000 child-days (228/29 803) and was
significantly higher in children with the lowest nutritional indexes, requiring therapeutic feeding. Multivariate analysis
showed that malaria incidence was significantly higher in children with the middle upper arm circumference < 115
mm (IRR: 1.75; 95% CI: 1.16 – 2.38) and with nutritional oedemas (IRR 1.66; 95% CI: 1.16 – 2.38).
Conclusion: Children hospitalized with severe PEM and undergoing therapeutic refeeding were at a higher risk
of clinical malaria and should be specifically protected against such a risk.
Keywords
Malnutrition; Malaria; Nutritional rehabilitation; DRC
Introduction
Malaria is the most common and deadly parasitic disease worldwide. In sub-Saharan Africa, malaria is an important cause of morbidity and mortality [1]. In 2000, the number of malaria fevers associated with high parasite density in children of less than 5 years was estimated at about 115 million and that of hospitalized from severe malaria cases in the same age group at more than half a million [2]. In the same year, the number of children having died of malaria was estimated at about 800 000, with 24 000 having recovered with permanent neurological damages [3].
In developing countries, including those in sub-Saharan Africa, malnutrition represents an additional burden and often co-exists with malaria [4]; in 2008, it is estimated that almost 30% of children of less than 5 years of age were underweight [5].
In Democratic Republic of Congo (DRC), malaria and malnutrition are significant problems among children. A demographic survey in 2007 found that about 10% of children under five years of age were undernourished and 4% severely undernourished [6]. In 2006, DRC reported 11% of all malaria cases in the African region and 9.6% worldwide [7].
The relationship between under nutrition and the susceptibility to uncomplicated malaria is controversial. Previous papers showed that under nutrition increased [8-10] the malaria risk. Formers studies showed that malnutrition decreased [11,12], or had no effect [13,14] on the malaria risk. At Lwiro, in the province of South Kivu, DRC, children without nutritional oedema at the time of hospitalization had a higher risk of malaria infection [15]. These contradictory results reflect the complexity of the interaction between the nutritional status and uncomplicated malaria.
About mortality, it has been shown that survival was lower in children hospitalized for malaria and suffering from Protein Energy Malnutrition (PEM) compared to those with a good nutritional status [16]. In addition, survival increased with decreasing severity of PEM [17].
Few studies on this topic have been carried out in DRC. Data on children hospitalized in Lwiro hospital have been analysed aiming at exploring such relationship. The purpose of this study was to examine the association between nutritional indicators on admission and the risk of clinical malaria during the hospitalization.
Methods
The study has been carried out in Lwiro Paediatric Hospital (LPH). The LPH is a 60-bed hospital operating since 1960 under the control of the nutrition department within the DRC ministry of scientific research. The LPH is located in eastern DRC, in South Kivu, a province at 1 760 m of altitude, in the Katana health district. At the study time LPH was a reference centre for the management of malnutrition and other paediatric problems in the region, in spite of the presence of Katana reference hospital and several health centres which were operating in the Katana health district. The health team comprised two medical doctors, including a paediatrician, and about 10 nurses. Patients were referred to LPH either from community-based malnutrition unit component or from other medical facilities for further investigation and paediatric management of any health problems. Children with severe malnutrition, i.e. with nutritional oedemas and/or a Z score weight for height < - 3 were admitted in a program of therapeutic feeding based on F-75 and F-100 milks during hospitalization. These formulations are specifically conceived for the dietary treatment of severe malnourished patients and contain 75 Kcal/100 ml and 100 Kcal/100 ml for F75 and F100, respectively [18]. Their preparation and administration were carried out according to a standard protocol [18]. Children not fulfilling the admission criteria for therapeutic feeding received a nutritional complement based on UNIMIX, which is pre-cooked flour of maize (80 %) and soya (20 %) enriched with minerals and vitamins. Vitamin A, amoxicillin, mebendazol and zinc were administered in routine management procedures for severely malnourished children at the LPH. Admission and discharge in the therapeutic feeding program were carried out according to WHO criteria [18].
From 1986, patient data on hospitalization and follow-up at the LPH were collected on standardized forms.
Data on hospitalized children between January 2003 and November 2006 were used to examine the association between nutritional status on admission and malaria risk during hospitalization. Children with a malaria infection on admission were excluded from analysis. Malaria was defined as the first one of the only clinical episode over the length of hospitalization in child-days. The maximum length of follow up has been arbitrarily set for 30 days as the number of children living longer was extremely small. A clinical malaria case was defined as a child with fever (axillary temperature ≥ 38°C), without any other clinical sign of another infection and a thick blood film positive for malaria parasites, any density. A blood sample for parasitaemia was collected weekly or daily in case of fever, stained with Giemsa 3% for about 30 minutes and then read, with the microscopist examining at least 100 HPF before declaring the slide negative [19]. Weight, height and the middle upper arm circumference (MUAC) were collected on admission, 3 days later and then weekly according to standard anthropometrics procedures as defined by WHO [20]. The z scores (ZS) height for age (H/A) and weight for height (W/H) were computed with the software Epinut, version 3.3.2 (Center for Disease Control and Prevention, Atlanta). The H/A and W/H ZS, the MUAC and the presence of oedemas have been used to quantify the PEM degree. The cut offs were 115 and 125 mm for the MUAC and -3 and -2 for HAZ, WHZ and WAZ [18,21]. Acute malnutrition was defined as a WHZ ≤ -2 while chronic malnutrition as a ZS for HAZ ≤ -2 [18]. Proportions were compared by using either the χ² or the Fisher exact test. Poisson regression was used to quantify the association between PEM indicators and clinical malaria during hospitalization for both univariate and multivariate analysis. Incidence rate ratios (IRR) and their 95% confidence intervals (95%CI) were computed by using the group in which the incidence was the lowest as reference. Analysis were carried out by using the following software’s: Epi Info version 3.3.2, STATA / SE 10.0 and SPSS for Windows version 17.0. The significance threshold was fixed at 0.05.
Results
During the study period, 4 572 children were hospitalized, 46.3% (2 117/4 572) having malaria infection/clinical attack at admission. The latter, 21% (445/2 115) with oedemas (2 children with missing values) and 16% (279/1 742) severely emaciated (the ZS W/H was missing for 375 children), were excluded from the following analysis. The average number of days of hospitalization was 21 days (range: 0 - 151).
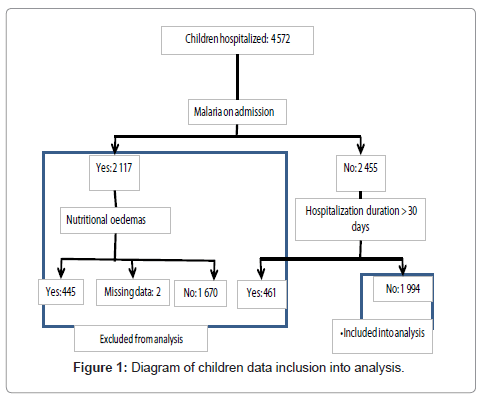
Among the 2 455 children without malaria on admission, those having been hospitalized for more than 30 days were excluded so that the analysis was carried out on 1 994 (81.4%) children. A diagram of children data inclusion in the analysis is detailed in Figure 1. Sociodemographics and nutritional characteristics of the children are shown in table 1. About 45% of them had edemas at admission and were included in the therapeutic feeding program while 70% were also chronically malnourished, i.e. ZS H/A ≤ -2 (Table 1).
| n | No* (%) | |
|---|---|---|
| Gender | 1 994 | |
| Male | 1 043 (52.3) | |
| Age (months) | 1 968 | |
| 0 - 11 | 479 (24.3) | |
| 12 - 23 | 393 (20.0) | |
| 24 - 35 | 313 (15.9) | |
| 36 - 59 | 373 (19,0) | |
| ≥ 60 | 410 (20,8) | |
| ZS H/A | 1 589 | |
| < -3 | 836 (52,6) | |
| -3 - < -2 | 273 (17,2) | |
| ≥ - 2 | 480 (30,2) | |
| ZS W/H | 1 576 | |
| < -3 | 349 (22,1) | |
| -3 - < -2 | 316 (20,1) | |
| ≥ - 2 | 911 (57,8) | |
| MUAC (mm) | 1935 | |
| < 115 | 495 (25,6) | |
| 115 - < 125 | 352 (18,2) | |
| ≥ 125 | 1 088 (56,2) | |
| Oedemas on admission | 1 991 | |
| Yes | 909 (45,7) |
No*: number
Table 1: Socio-demographic and nutritional characterictis of the cohort under surveillance.
Nutritional oedemas were significantly less frequent in the youngest age group (0-11 months) (15.4%), as compared to older children (12-23 months: 47.1%; 24-35 months: 55.1%, 36-59 months: 64.7%; ≥ 59 months: 56.3%) (p < 0.001). No difference between boys and girls was found.
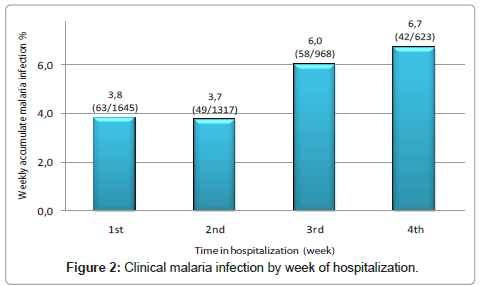
The clinical malaria proportion during hospitalization was 7.65 ‰ (228/29 803) child-days and varied significantly according to the week of hospitalization, with the third and fourth week having the highest proportion (Figure 2). Malaria varied significantly with age, with the youngest group having the lowest value, the 12-23 months old the highest and then decreasing steadily in the older age groups (Table 2). In addition, malaria was more frequent in those children who had, at the time of hospitalization, nutritional oedemas, a ZS W/H < -2 and a MUAC <115 mm (Table 2). In multivariate analysis, malaria remained significantly higher in children with nutritional oedemas and in those with a MUAC <115 mm, during hospitalization (Table 3).
| Risk factors | Incidence rate (‰ child-days) | IRR | (95% CI) | p |
|---|---|---|---|---|
| Age in months (n= 1 958) | 0,013 | |||
| 0 - 11 | 6,13 | 1 | ||
| 12 – 23 | 9,79 | 1,60 | (1,03 - 2,51) | |
| 24 - 35 | 9,20 | 1,50 | (0,94 - 2,42) | |
| 36 - 59 | 8,60 | 1,42 | (0,91 - 2,23) | |
| > 59 | 5,35 | 0,87 | (0,54 - 1,42) | |
| Sex (n=1 984) | 0,34 | |||
| Girls | 7,14 | 1,00 | ||
| Boys | 8,11 | 1,14 | (0,87 - 1,49) | |
| Oedemas at admission (n=1 981) | 0,020 | |||
| No | 6,30 | 1 | ||
| Yes | 8,67 | 1,38 | (1,04 - 1,83) | |
| ZS W/H (n=1 569) | 0,007 | |||
| ≥ -2 | 5,73 | 1 | ||
| - 3 - < - 2 | 8,95 | 1,56 | (1,06 - 2,29) | |
| < - 3 | 9,48 | 1,66 | (1,14 - 2,39) | |
| ZS H/A (n=1 583) | 0,09 | |||
| ≥ -2 | 6,84 | 1 | ||
| - 3 - < - 2 | 4,79 | 0,70 | (0,38 - 1,25) | |
| < - 3 | 8,05 | 1,18 | (0,82 - 1,72) | |
| MUAC in mm (n= 1 926) | < 0,001 | |||
| ≥ 125 | 6,47 | 1 | ||
| 115 - < 125 | 6,07 | 0,94 | (0,61 - 1,40) | |
| < 115 | 11,89 | 1,84 | (1,36 - 2,47) | |
Table 2: Clinical malaria infection during hospitalization by risk factors.
| IRR | (95% CI) | p | |
|---|---|---|---|
| Nutirtional oedemas | 0,005 | ||
| No | 1 | ||
| Yes | 1,66 | (1,16 -2,38) | |
| MUAC in mm | 0,002 | ||
| ≥ 125 | 1 | ||
| 115 - < 125 | 0,75 | 0,46 – 1,21 | |
| < 115 | 1,75 | 1,16 – 2,63 |
Sex, age and ZS H/A not significant
Table 3: Multivariate analysis of clinical malaria infection during hospitalization and several risk factors.
Among children who stayed at least 2 to 3 weeks, malaria risk remained significantly higher in malnourished children (tables not showed).
Discussion
The study, analyzing routine data of LPH, has shown that clinical malaria was more frequent in severely malnourished children requiring therapeutic feeding. If this hypothesis can be confirmed by subsequent study, during nutritional rehabilitation in malaria endemic area, severely malnourished children must be protected against malaria.
It is also important to mention in the present study, children found to have a malaria infection at the time of admission were excluded from analysis so that the proportion of malaria in the newly established cohort of non infected children could be measured during the hospitalization. The higher malaria proportion observed during the third and fourth week of follow up indicates that most infections were recently acquired, around or after admission.
However, this study has an important limitation requiring to be mentioned. The design of the study cannot permit to establish a causality relationship between malaria and the changing of nutritional status during therapeutic feeding. Further studies with ad hoc design must be carried out.
The frequent occurrence of malnutrition among children admitted in LPH is not only the consequence of being a referral facility for these cases but also of a real problem in the surrounding communities. Indeed, in 2001, a Multiple Indicators Cluster Survey reported that in South Kivu province, there were 47.6% children with a ZS H/A < -2 and 12.2% with a ZS W/H < -2 [22].
Information on the malaria risk in malnourished patients undergoing therapeutic feeding are scarce. In Nigeria, malaria was apparently suppressed in nomad and non nomad children during a famine period, only to be apparently reactivated by refeeding [23]. Nevertheless, more recently in the Gambia, clinical malaria was significantly observed more often among stunted children (defined as ZS H/A<-2), indicating that chronically malnourished children were at higher risk of malaria episodes [24]. These results differ from those obtained in LPH as in the latter clinical malaria was more frequent in children with severe acute malnutrition, as indicated by the presence of oedemas and the low MUAC values. It should be noticed that the two study populations were different as in the Gambia the cohort comprised children living in rural villages, representative of the local population, while in DRC this was constituted by hospitalized children, some of them with severe malnutrition and requiring therapeutic feeding. Therefore, the results obtained are not directly comparable and are not necessarily contradictory.
In Burkina Faso no association between the occurrence of clinical malaria and PEM was found; however, the latter was associated with a higher mortality risk [25]. It is important to underline that in this particular study, no case management of malnourished children was done. Moreover, malaria cases were identified by daily visits and this may have over- estimated the incidence of clinical malaria, possibly hiding any difference that may have existed.
The observation that clinical malaria was more frequent in malnourished children under therapeutic feeding could be explained by the provision of nutrients previously lacking and necessary for the development of parasites. This hypothesis is supported by several data obtained from the animal and the in vitro model. In mice reducing the proteinic food content resulted in a decreasing density of Plasmodium berghei [26]. In addition, adding a combination of amino acids to a diet based on casein increased the parasite density [27]. Adding human albumin to a P. falciparum culture was followed by its inclusion in the parasite and its disappearance after 12 hours, indicating its degradation by the parasite [28]. More recently, it has been shown that in P. falciparum parasitized red blood cell, proteins were phosphorilated [29] and that the parasite needs para-amino benzoic acid for its folate synthesis [30]. Nevertheless, it could be possible that the relationship between malnutrition, therapeutic feeding and malaria risk is more complex as children suffering from this status have multiple nutritional deficiencies.
Conclusion
Our study indicates that clinical malaria was more frequent in severely malnourished children requiring therapeutic feeding.
The results presented here have been obtained by analyzing routine data whose primary purpose was not to investigate the causal relationship between malaria and the nutritional status changing in hospitalized children suffering from PEM and undergoing therapeutic refeeding.
Nevertheless, our results suggest that the nutritional rehabilitation of these patients may increase their risk of clinical malaria. This should be confirmed by ad hoc studies designed to answer this question. In any case, in malaria endemic area, these patients should be protected against malaria, either with preventive measures such as insecticidetreated bed nets during the course of hospitalization or the systematic screening and treatment for the positive cases.
Acknowledgements
The authors would like to thank the Lwiro pediatric hospital staff for their high quality work despite the difficult conditions, including high insecurity in the east of the Democratic Republic of the Congo region.
They would also like to thank the “Van Buren foundation” and the Belgian “Commission Universitaire pour le Development (CUD)” for their financial support.
References
- World Health Organization (2009) Global estimates of malaria cases and deaths in 2008. World Malaria Report: 27.
- Roca-Feltrer A, Carneiro I, Armstrong Schellenberg JR (2008) Estimates of the burden of malaria morbidity in Africa in children under the age of 5 years. Trop Med Int Health 13: 771-783.
- Rowe AK, Rowe SY, Snow RW, Korenromp EL, Schellenberg JR, et al. (2006) The burden of malaria mortality among African children in the year 2000. Int J Epidemiol 35: 691-704.
- Nubé M, Sonneveld BG (2005) The geographical distribution of underweight children in Africa. Bull World Health Organ 83: 764-770.
- Unicef (2010) Progress for children. Achieving the MDGs with equity: 14.
- Ministère du Plan RDC, Measure DHS Macro International, Ministère de la Santé RDC (2008) Enquête démographique et de santé EDS RDC 2007. Rapport final: 139: 153-162.
- World Health Organization (2008) Profiles, 30 high-burden countries. World Malaria Report:66 – 68.
- Verhoef H, West CE, Veenemans J, Beguin Y, Kok FJ (2002) Stunting may determine the severity of malaria-associated anemia in African children. Pediatrics 110: e48.
- Deen JL, Walraven GE, von Seidlein L (2002) Increased risk for malaria in chronically malnourished children under 5 years of age in rural Gambia. J Trop Pediatr 48: 78-83.
- Friedman JF, Kwena AM, Mirel LB, Kariuki SK, Terlouw DJ, et al. (2005) Malaria and nutritionnal status among pre-school children: results from cross-sectionnal surveys in western Kenya. Am J Trop Med Hyg 73: 698-704.
- Hendrickse RG, Hasan AH, Olumide LO, Akinkunmi A (1971) Malaria in early childhood. An investigation of five hundred seriously ill children in whom a "clinical" diagnosis of malaria was made on admission to the children's emergency room at University College Hospital, Ibadan. Ann Trop Med Parasitol 65: 1-20.
- Genton B, Al-Yaman F, Ginny M, Taraika J, Alpers MP (1998) Relation of anthropometry to malaria morbidity and immunity in Papua New Guinean Children. Am J Clin Nutr 68: 734-741.
- Snow RW, Byass P, Shenton FC, Greenwood BM (1991) The relationship between anthropometric measurements and measurements of iron status and susceptibility to malaria in Gambian children. Trans R Soc Trop Med Hyg 85: 584-589.
- Tshikuka JG, Gray-Donald K, Scott M, Olela KN (1997) Relationship of childhood protein-energy malnutrition and parasite infections in an urban African setting. Trop Med Int Health 2: 374-382.
- Mitangala Ndeba P, Hennart P, D'Alessandro U, Donnen P, Porignon D, et al. (2008) Protein-energy malnutrition and malaria-related morbidity in children under 59 months in the Kivu region of the Democratic Republic of the Congo. Med Trop (Mars) 68: 51-57.
- Fishman S, Caulfield L, de Onis M et al. (2004) Malnutrition and the global burden of disease: underweight. Comparative Quantification of Health Risks: The Global and Regional Burden of Disease due to 25 Selected Major Risk Factors. Cambridge: World Health Organization.
- Caulfield LE, Richard SA, Black RE (2004) Undernutrition as an underlying cause of malaria morbidity and mortality in children less than five years old. Am J Trop Med Hyg 71: S55-S63.
- WHO (1999) Management of severe malnutrition: a manual for physicians and other senior health workers. Geneva, World Health Organization.
- Organisation Mondiale de la Santé (1982) Manuel des techniques de base pour le laboratoire médical : Coloration de giemsa (gouttes épaisses et étalements minces). Organisation mondiale de la santé : 193-195.
- Organisation Mondiale de la Santé OMS (1995) Utilisation et interprétation de l’anthropométrie. Rapport d’un comité OMS d’experts, Organisation mondiale de la santé, Genève 854 :473-475.
- WHO,UNICEF (2009) Joint statement. WHO child growth and the identification of severe acute malnutrition in infants and children. Geneva, New York.
- Ministère du plan et de la reconstruction RDC, Unicef et USAID (2002) Enquête nationale sur la situation des enfants et des femmes MICS 2/2001. Rapport d’analyse, Kinshasa, République Démocratique du Congo.
- Murray MJ, Murray AB, Murray NJ, Murray MB (1978) Diet and cerebral malaria: the effect of famine and refeeding. Am J Clin Nutr 31: 57-61.
- Deen JL, Walraven GE, von Seidlein L (2002) Increased risk for malaria in chronically malnourished children under 5 years of age in rural Gambia. J Trop Pediatr 48: 78-83.
- Muller O, Garenne M, Kouyate B, Becher H (2003) The association between protein-energy malnutrition, malaria morbidity and all-cause mortality in West African children. Trop Med Int Health 8: 507-511.
- Edirisinghe JS, Fern EB, Targett GA (1981) The influence of dietary protein on the development of malaria. Ann Trop Paediatr 1: 87-91.
- Fern EB, Edirisinghe JS, Targett GA (1984) Increased severity of malaria infection in rats fed supplementary amino acids. Trans R Soc Trop Med Hyg 78: 839-841.
- El Tahir A, Malhotra P, Chauhan VS (2003) Uptake of proteins and degradation of human serum albumin by Plasmodium falciparum – infected human erythrocytes. Malar J 2: 11.
- Wu Y, Nelson MM, Quaile A, Xia D, Wastling JM, et al. (2009) Identification of phosphorylated proteins in erythrocytes infected by the human malaria parasite Plasmodium falciparum. Malar J 18: 105.
- Wang P, Wang Q, Sims PF, Hyde JE (2007) Characterisation of exogenous folate transport in Plasmodium falciparum. Mol Biochem Parasitol 154: 40-51.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 14977
- [From(publication date):
specialissue-2012 - Nov 21, 2025] - Breakdown by view type
- HTML page views : 10263
- PDF downloads : 4714