Research Article Open Access
Clinical Experience on Bioactive Glass S53P4 in Reconstructive Surgery in the Upper Extremity Showing Bone Remodelling, Vascularization, Cartilage Repair and Antibacterial Properties of S53P4
Lindfors NC*Helsinki University Central Hospital, Department of Orthopaedic and Hand Surgery, Helsinki University, Helsinki, Finland
- Corresponding Author:
- Lindfors
Töölö Hospital, Topeliuksenkatu 5
00260 Helsinki, Finland
E-mail: nina.c.lindfors@hus.fi
Received date: July 04, 2011; Accepted date: August 10, 2011; Published date: August 12, 2011
Citation: Lindfors NC (2011) Clinical Experience on Bioactive Glass S53P4 in Reconstructive Surgery in the Upper Extremity Showing Bone Remodelling, Vascularization, Cartilage Repair and Antibacterial Properties of S53P4. J Biotechnol Biomaterial 1:111. doi:10.4172/2155-952X.1000111
Copyright: © 2011 Lindfors NC. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Biotechnology & Biomaterials
Abstract
Bioactive glass (BAG) S53P4 is a bone bonding, osteoconductive and osteostimulative bone substitute with proven antibac-terial properties. In this paper, several clinical aspects using BAG S53P4 in reconstructive surgery in the upper extremity is presented, demonstrating bone remodelling, vascularization, cartilage repair and antibacterial properties of BAG S53P4. In a prospective, randomized, long-term study, BAG S53P4 was compared to autograft bone, in nine patients, in treatment of benign bone tumours in the hand. No radiological difference between the two groups was observed at 18 months. No material-related adverse effects were observed at the 14-year long-term follow-up. In the BAG group, a thickened cortex was observed on CT. MRI revealed that the bone marrow was mainly or partly fatty. BAG S53P4 was used in treatment of an intra-articular condylar open fracture in a child. In a re-operation, it was observed that the treated region was vascularized at three months, which was histopathologically confirmed. The vascularized bone substitute mass had supported the injured cartilage. An angulation of the proximal interphalangeal joint was observed but this did not affect the use of the hand. The finger was painless and stable. Finally, BAG S53P4 was used in treatment of an infected comminuted olecranon fracture. The patient had sustained a fistular formation to a previously used bone substitute. The pathogen causing the infection was S epidermidis. In a re-operation BAG S53P4 was used as bone substitute. No re-infection was observed during a six-month follow-up.
Keywords
Bioactive glass; Bone substitute; Osteostimulative; Antibacterial; Osteomyelitis; Osteoconductive
Introduction
Autogenous bone (AB) with its osteoinductive potential has been the golden standard for filling defects in reconstructive surgery. However, disadvantages including donor-site morbidity and increased operative time associated with the harvesting procedure, usually at the iliac crest, have lead to the development of synthetic bone substitutes. Many bone substitutes are currently available on the market, including ceramics, bioactive glasses (BAGs), demineralized bone matrix, allograft bone and bone morphogenetic proteins. Opening of the iliac crest in handtumour surgery can, therefore, today be considered as an exaggerated procedure.
Bone substitutes differ not only in behaviour i.e. in resorption-rate, mechanical strength and bone forming capacity, but also on molecular and cellular bases. Biomaterials designed to stimulate specific cellular responses, as BAG S53P4 used in this study, are called third-generation biomaterials [1]. BAGs are osteoconducting bone substitutes with bone-bonding properties. The bioactive process leading to proliferation of osteoblasts, observed at the surface of the glass with subse-quent bone bonding, has been described as a sequence of reactions in the glass and at its surface. The bioactive process starts with a rapid exchange of Na+ in the glass with H+ and H3O+ from the surrounding tissue, leading to the formation of silanol (SiOH) groups at the glass surface. After repolymerization, a SiO2-rich layer is formed. Due to migration of Ca2+ and PO4 3- groups to the surface and cystallization, a CaO-P2O5 hydroxyapatite (HA) layer is formed on top of the Si-rich layer. Finally, cell interactions with the HA layer on the glass subsequently initiate the bone-forming pathway [2-6].
BAGs also have other qualities which are beneficial in bone reconstruction surgery. They are known to have antibacterial properties, observed in vitro for all clinically important aerobic and anaerobic bacteria tested, as well as very resistant bac-teria [7,8]. The antibacterial quality of BAGs is caused by the dissolution reactions at the glass surface, leading to an elevated PH and osmotic effects around the glass granule. BAGs are also known to stimulate the release of angiogenic growth factors and to promote angiogenesis, which is essential for bone formation [9].
In optimizing the outcome of a surgical procedure in which bone substitutes are planned to be used, it is imperative that the surgeon has a thorough understanding of the short and long-term behaviour of the material. This paper presents several aspects on BAG S53P4 used in reconstructive surgery in the upper extremity; a long-term follow-up on BAG S53P4 as bone substitute in bone tumour surgery in the hand, in treatment of a bone and cartilage condylar defect in an index finger, in a child and additionally, in the treatment of osteomyelitis in the ulna
Patients and Methods
Long-term follow-up on BAG S53P4 in benign bone tumour surgery in the hand
Nine patients (four females, five males) with a radiologically diagnosed benign bone tumour in the hand participated in a prospective, randomized, study during 1993-1995. The tumours were found either after a pathological fracture (n = 6) or on X-rays taken because of local pain (n = 3). All pathological fractures were treated conservatively with an immobilization cast, before any bone-filling operation was performed. The tumours were located in the proximal phalanx of the finger (n = 6), in the middle phalanx of the finger (n = 1), and in the distal phalanx of the finger (n = 2). The mean age of the patients was 39 (range 33 - 50) years.
The patients were randomized into one of two groups, BAG or AB. In the BAG group, BAG S53P4 with a composition of 53 wt-% SiO2, 23 wt-% Na2O, 20 wt-% CaO and 4 wt-% P0O5 (manufactured currently as BonAlive® by Bonalive Biomaterials Ltd., Turku, Finland) was used as a bone graft substitute (five patients). BAG S53P4 gained European approval for orthopaedic use as a bone graft substitute in 2006. In the AB group, AB harvested from the iliac crest was used (four patients).
In the operation the cavitary defect was opened by detaching the cortical lid. A biopsy was then taken to confirm the pre-operative clinical and radiological diagnosis. The tumour was meticulously removed, and the inner wall of the cavity was refreshed, using bone drills. The cavity was filled with either 1 – 2-mm BAG granules or AB.
The type of tumour as classified by histopathological examination was an enchondroma (n = 8) and an epidermal cyst (n = 1). The primary follow-up scheme included visits at the outpatient department at 2 weeks and at 3, 8, 12, 18, 24 and 36 months. The volume of the cavity was estimated both on X-rays and computerized tomographic (CT) scans by measuring three orthogonal diameters for an ellipsoidal model.
The patients were asked to participate in a long-term 14-year (range 13 – 15 years) follow-up and were re-examined at the outpatient department. Range of motion (ROM) of the metacarpophalangeal (MCP) joint, the proximal interphalangeal (PIP) joint and the distal interphalangeal (DIP) joint were measured. The grip strength of both hands (Jamar Hand dynamometer®, J.A. Preston Corp., Jackson, MI, USA) was recorded. The Semmes-Weinstein monofilament test was used for sensory evaluation of the operated finger. The subjective functional and cosmetic results were graded as excellent, good, fair or poor, according to the patients´ subjective feelings of the treatment.
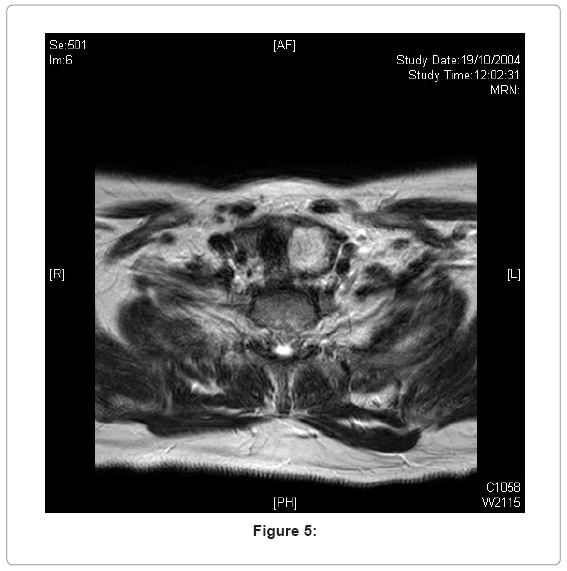
X-rays and magnetic resonance imaging (MRI) scans were performed for evaluation of the treated bone region. In the BAG group, CT scans were performed as well. The MRI examinations were performed in a 1.5-T scanner (Intera Achiera, Philips Medical Systems, Best, The Netherlands). Axial and coronal T1-weighted sequences, axial proton density and T2-weighted fat suppression sequence, coronal proton density and sagittal intermediate- weighted fat suppression sequence were included. Gadolinium was not used.
The CT examinations were performed in a four-slice helical CT scanner (HiSpeed QX/i, General Electric Co., Milwaukee, WI, USA). The treated region was scanned in the axial plane and reconstructed in three orthogonal planes on a workstation (GE Advantage AW 3,06 sdc workstation). The slice widths and intervals of 1.25/0.625 mm were used.
The study was conducted in accordance with ethics principles originating in the latest version of the Declaration of Helsinki, applicable regulatory requirements including standards of the International Organization of Standardization, and adherence to Finnish law and regulations. The local ethics committee approved the study protocol, and patient-informed consent was obtained. The clinical study, use of the clinical report form and statistical evaluation were performed according to the Good Clinical Practice standard.
Patient A: BAG S53P4 used in treatment of an injury in the indexfinger in a child. A six-year-old child sustained an open fracture injury from a circular saw, on her left index finger, on the dorsal side of the PIP joint. The extensor was injured, the flexors and the neurovascular bundles were intact. The injury resulted in a large bone defect on the distal proximal phalange, as well as cartilage defects on both sides of the PIP joint. In the primary op-eration the bone defect of the proximal phalange was filled with BAG S53P4. The finger was supported with a K-wire, and the extensor was reconstructed. Only 1/5 of the proximal cartilage was left on the radial side and, therefore, a piece of the volar plate was placed in the joint space, to ensure that no glass granules could migrate into the joint-space. After one month the K-wire was removed and mobilisation of the stiff finger was started. However, on X-ray it was revealed that the bone substitute had not supported the ulnar condyle and an ulnar angulation of 50 degrees was observed, in the painful finger.
Several treatment options were considered; amputation, artrodesis with subsequent loss of growth of the middle phalange or a tranplantation of a piece of a phalange from a toe. During the second operation it was, however, observed that the bone substitute was fully vascularized and small pieces of cartilage, which had been seen in the primary operation had grown into a connected cartilageous tissue, supported by the BAG. BAG granules were incorporated in a partly mineralized smooth tissue mass. In order to avoid artrodesis and the risk of disturbance of the growth of the finger, a correction os-teotomy to correct the angulation of the cartilage was performed. To support the bone, K-wires partly drilled through the bone substitute-mass were used. A small piece from the mass of the bone substitute was taken for histopathological ex-amination. Six weeks later the K-wires were removed.
Patient B: BAG-S53P4 in treatment of osteomyelitis in the ulna. A 45-year-old male sustained a comminuted olecranon fracture and a proximal radial fracture in 2010, due to a fall. On the ulnar side a locking- compression-plate was used, as well as a bone substitute (Norian®) for filling the bone defect. A hemi-arthroplasty using a R-Head prosthesis was performed on the radial side.
Postoperatively an infection with a fistular formation to the bone substitute, revealed by fistulography, was observed. The pathogen causing the infection was S epidermidis. A re-operation was performed, the bone substitute was removed and the cavitary bone defect was filled with gentamicin beads (Septopal®). One month later the gentamicin beads were removed and the cavitary bone defect was filled with BAG S53P4 granules. Two months later the patients sustained another ulnar fracture, which was treated using a plate.
Results of the long-term follow-up
Seven patients (three in the BAG group, four in the AB group) completed the long-term follow-up. The BAG S53P4 was well tolerated. No material-related adverse effects were observed during 14 years.
The functional outcome is shown in Table 1. In the BAG group, the mean MCP flexion was 75°, the mean PIP flexion 85° and the mean DIP flexion 80°, and in the AB group 77°, 92° and 70° respectively. No extension deficit was observed in any of the groups. The grip strength in the treated hand was 100%, compared to the untreated hand, in both groups. The Semmes-Weinstein monofilament test was normal in both groups (3.61). The subjective evaluation of the treatment was excellent (n = 2), and fair (n = 1) in the BAG group, and excellent (n = 3), and good (n = 1) in the AB group. One patient in the BAG group graded the postoperative outcome as fair, due to a post-operatively missed fracture, and one patient in the AB group graded the postoperative outcome as good, because the patient had suffered from long-lasting post-operative pain in the finger. A residue cyst was observed at two years and the patient underwent a re-operation, in which AB was used.
| Nr | Bone substitute | Flexion MP | Flexion PIP |
Flexion DIP | Extension deficit |
Grip strength (kg) oper |
Grip strength (kg) nonoper |
Filament sensation |
|---|---|---|---|---|---|---|---|---|
| 1 | BAG | 100 | 100 | 90 | 0 | 30 | 30 | 3.61 |
| 2 | BAG | 70 | 100 | 70 | 0 | 28 | 26 | 3.61 |
| 3 | BAG | 54 | 54 | NA | 0 | 20 | 22 | 3.61 |
| 4 | AB | 90 | 100 | 50 | 0 | 85 | 85 | 3.61 |
| 5 | AB | 90 | 90 | 90 | 0 | NA | NA | 3.61 |
| 6 | AB | 90 | 100 | 60 | 0 | 46 | 44 | 3.61 |
| 7 | AB | 40 | 80 | 0 | 80 | 80 | 3.61 |
Table 1: Clinical outcome of treatment. BAG = bioactive glass S53P4, AB = autogenous bone.
Radiological findings of the long-term follow-up
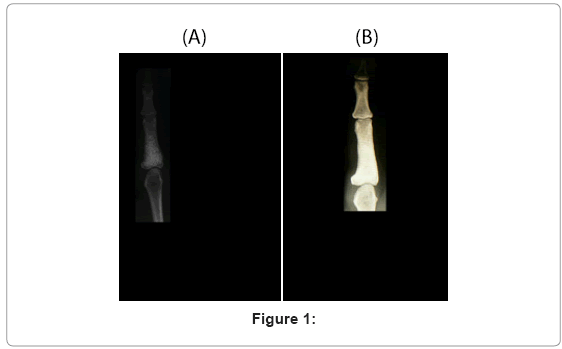
The radiological long-term outcome is visualized in Figure 1.
The filled cavitary defects began to remodel earlier in the AB group than in the BAG group. In the AB group the filled cavities were not measurable on X-rays at 12 months. In the BAG group, evaluation on both X-rays and CT scans revealed that the filled cavities began to diminish after 12 months. No difference between the two groups could be observed at 18 months. The measured volumes of the bone cavities evaluated on X-rays are shown in Table 2. A thickened cortex mean of 2.3 (SD 0.35) mm, was observed on X-rays after eight months in the BAG group, compared with the adjacent normal cortex mean of 1.3 (SD 0.10) mm. The 14-year follow-up revealed that the thickened cortex remained, which was observed on X-rays, CT and MRI.
| Months | BG (cm3) / SD | AB (cm3) / SD |
| 0 | 1.1 / 0.7 | 2.3 / 0 |
| 1 | 1.1 / 0.6 | 1.3 / 1.1 |
| 3 | 1.1 / 0.6 | 0 / 0 |
| 8 | 0.9 / 0.5 | 0 / 0.1 |
| 12 | 0.9 / 0 | 0 / 0 |
| 18 | 0.1 / 0 | 0 / 0 |
| 24 | 0.1 / 0.1 | 0 / 0.1 |
| 36 | 0 / 0 | 0 / 0 |
Table 2: Mean preoperative / volume at 11-year follow-up of bone cavity evaluated from X-ray.
In the BAG group, the treated cavity had a dense, sclerotic appearance on X-rays. CT density measurements revealed a mean of 708.7 (SD 469.9) Hounsfield units (HU) for the treated cavity in the BAG group and a mean of -10.7 HU (SD 58.4) for normal bone in an untreated finger. In one patient, remnants of glass surrounded by bone were also observed. The bone marrow in the BAG group appeared mainly fatty on MRI in two patients, and partly fatty or partly sclerotic in one patient. In two patients focal low-signal areas, probably due to remnants of glass granules, were observed.
In the AB group the treated area appeared normal on X-rays, and on MRI the bone marrow was mainly fatty.
Results of patient A: Seven months after the re-operation the child was re-examined at the outpatient department. The child was using the index finger in normal living. The PIP joint was painless and stable in all directions. A very good pinch-grip between the thumb and the index finger was observed and the child was able to pick-up small toys without any problem. An extension deficit of 10 degrees and an active flexion of 10 degrees were detected. In a grip position, the pulp of the index finger remained 2 cm from the distal crease of the hand. An ulnar deviation of the finger of 28 degrees was observed. However, the angulation of the finger did not affect the functional outcome of the hand and therefore, no further treat-ments were planned.
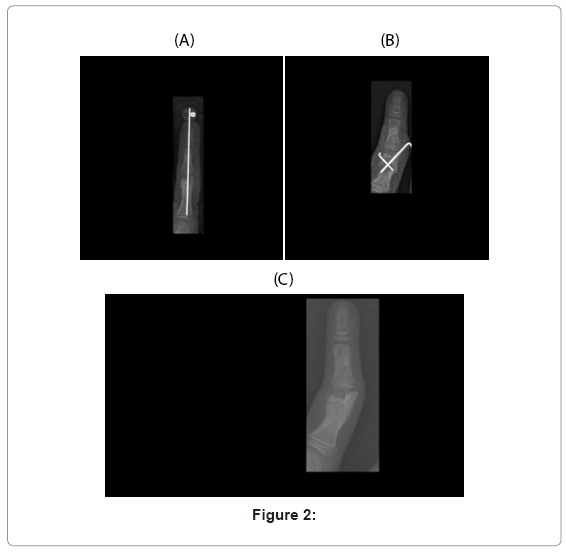
Bone remodellation was observed on X-rays in the treated region of the condyle. BAG S53P4 granules were still visible, mainly in the region of the subchondral bone (Figure 2). The histological examination revealed no inflammatory cell reac-tions. Vascularized fibrotic tissue surrounding BAG granules was observed.
Results of patient B: The patient was examined at the outpatient department one month postoperatively. No re-infection was observed.
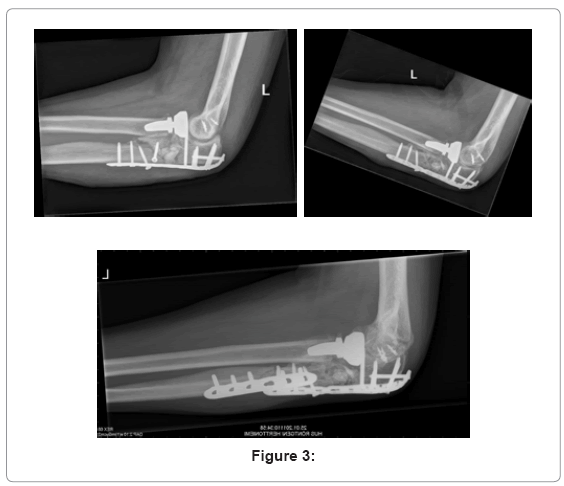
Four months later the fractures had healed. An extension deficit of 25 degrees and a flexion of 110 degrees of the elbow were measured. Pronation was 70 degrees and supination 60 degrees. On X-rays, it was observed that the treated region had started to remodel. A smoothening of the shape of the BAG granules was seen, as well as new bone formation between the granules (Figure 3).
Discussion
BAG S53P4 has gained popularity especially in craniomaxillary surgery [10]. It has also been used in several orthopaedic applications, such as a filling material in benign bone tumour surgery and in treatment of osteomyelitis [11,12].
BAG S53P4, classified as a third-generation bone substitute, is a biomaterial designed to stimulate specific cellular re-sponses. Osteostimulation describes a biological response that involves activation and stimulation of various cell types and cell phases. This process is more active than osteoconduction and anticipates a more rapid tissue response at molecular and cellular levels. Attachment, proliferation and differentiation of osteoblasts have been observed rapidly after implantation, as well as colonization of osteoprogenitor cells, at the surface of BAGs. Up-regulation or activation of families of genes, such as growth factors and cytokines, cell surface antigens and receptors, and signal transduction molecules increase 2-6-fold by ionic dissolution products of BAGs.
Although BAGs affect the bone-forming process in a positive manner, the remodellation of the treated region has been observed to be slower in BAG filled defects, compared to autograft filled defects. In a 3-year follow-up the remodelling of bone with subsequent disappearance of the filled cavitary bone defect was seen earlier in AB filled defects, than in defects filled with BAG. At 18 months the filled cavities in both groups were almost comparable on X-rays, and at 24 months no difference in cavity volume between the two groups could any longer be observed [11]. In the BAG group, the region of the filled cavity appeared dense on X-rays and CT scans. This long-term follow-up shows that the appearance of the filled cavity seen on X-rays and CT scans after three years remains in both groups. A weakness in this long-term study is, however, the small number of patients. This is explained by the fact that the study was conducted more than ten years before the product was available on the market.
Bone substitutes differ in resorption-rates. Calcium-sulphate i.e. is known to have a high resorption-rate, as other bone substitutes, such as HA will have a longer lifespan. Histological observations on an osteoconductive HA ceramic, used in tibial plateau surgery, revealed that the material due to its porosity, was incorporated in bone. No biodegradation was, however, histologically observed [13], showing the difficulty in evaluating bone formation on X-rays and on CT scans. In this study, MRI revealed that the bone marrow in the BAG group was fatty or partly fatty, resembling the appearance of the filled cavity in the AB group.
Bone mineral density (BMD) measurements have been used in evaluating bone formation using BAG S53P4 in – vitro and in – vivo. In a clinical follow-up study on frontal sinus obliteration using BAG S53P4 as bone graft subtitute, a significant de-crease in the level of Hounsfield units (HU) was observed during the first year after implantation. A stabilization at a level of 808.9 ± 86.2 HU was noted at 48 months [14]. This is in accordance with the mean value (708.7 HU) obtained for BAG filled defects in this study and experimentally obtained HU levels in a rabbit spinal fusion model [15].
As in this study, enchondromas are the most common bone tumours in the hand. Most often they are treated with curettage and bone grafting. Recent studies have indicated that especially small bone tumours can be treated without augmentation, and that sufficient bone strength can be achieved without bone substitutes [16]. However, in Olliers ´ disease, patients suffer from multiple enchondromas, which may increase the amount of bone substitute needed.
Depending on the aetiology of the bone tumour, recurrences are also seen after bone tumour surgery. Recurrence rates of 30% to 66% for aneurysmal bone cysts (ABCs) have been reported, most likely observed within two years after primary treatment [17]. BAG S53P4 has been successfully used as a bone substitute in treatment of a recurrent ABC in the proximal phalanx of the finger in a 3-year-old child. The filled cavity appeared dense on X-ray and no sign of recurrence was ob-served. Interestingly, the growth of the phalanx was not disturbed by the bone substitute, as the severely enlarged phalanx remodelled to a normal shape during a two-year follow-up [18]. The slow dissolution of the BAG combined with its osteo-conductive and osteostimulatory qualities were considered to be beneficial in the treatment, since BAG mechanically may prevent the formation of a recurrent cyst.
The chemical reactions at the surface of the BAG release soluble Si, Ca, P and Na ions, giving rise to both intracellular and extracellular responses [1]. Vascularization plays a significant role in the bone tissuehealing process. During the re-operation of the injured finger, it was observed that the bone defect, which had been filled with BAG S53P4 was fully vas-cularized at three months. BAG S53P4 granules were incorporated in a smooth mass. The small injured pieces of cartilage tissue had remodelled to a connected tissue on top of the BAG S53P4 granules. The small piece of tissue obtained for histo-logical examination at the outer part of the defect, showed that the tissue consisted of vascularizited fibrous tissue. This is in accordance with previous observations in an in – vivo model for frontal sinus and calvarian bone defect obliteration with BAG-S53P4 and HA. Vascularization and new bone formation occur more rapidly in defects filled with BAG S53P4 than in HA-filled defects, and the initial fibrous tissue formation that is related to a considerable amount of blood vessels, is also more rapid in BAG S53P4-filled defects [14].
BAG 45S5 Bioglass™ also stimulates release of angiogenic growth factors and promotes angiogenesis, which has been de-scribed in several studies. Increases in tubular branching and formation of complex networks of interconnected tubules have been observed after addition of a fibroblast-conditioned medium, produced in the presence of 45S5 Bioglass™ [9]. Soluble products of 45S5 Bioglass™ that induce endothelial cell proliferation and up-regulation of vascular endothelial growth factor (VEGF) production indicate that 45S5 Bioglass™ possesses a proangiogenic potential [19], and a material-dependent angiogenetic response in the presence of a BAG coating with significantly enhanced mitogenic stimulation of endothelial cells and an additive effect of VEGF release, has also been demonstrated in an in - vivo rat criticalsize defect model [20].
It is obvious that a treated region with BAG is rapidly vascularized. The mineralization and remodellation of the treated region, however, takes a longer time. Treated bone defects, especially those involving cortical and subchondral defects, therefore, need to be supported to achieve mechanical strength. The alignment of the treated injured finger, would proba-bly have been better, if the supporting K-wires, used in the re-operation, would not have been removed already after six weeks. This is in accordance with the good functional and radiological long-term results, observed for load-bearing lateral tibial plateau fractures treated with BAG-S53P4 and stabilizing plates [21]. Despite the angulation of the finger, a good functional and subjective outcome was, however, achieved and an arthrodesis of the PIP joint could be prevented, at least for the moment, giving the chance to the finger to grow in length. As the granules will slowly be resorbed during the re-modelling process, it is also imperative that the amount of BAG granules used to support the subchondral defect, is suffi-cient.
The cartilage repair on the BAG granules is interesting. Hyaline cartilage repair has been reported to occur on the surface of solid and porous BAG cones [22,23]. In an in - vivo cartilage model using an injectable composite of BAG-S53P4 and poly(e-caprolactone-co-D,Llactade) as thermoplastic carrier, new cartilage tissue covering the implant was observed in 82% of the defects filled with BAG 70% liquid. The authors conclusion was that the influence of BAG is an important stimulating factor for regeneration of cartilage tissue observed in the study [24]. This phenomenon needs further investigation, and a study on BAG and its effect on cartilage repair have been conducted.
Bacterial colonization is promoted by the ability of the bacteria to produce protein-specific adhesins on the surfaces of the implanted material. The subsequent bacterial induced formation of biofilms, makes treatment with antimicrobial agents difficult and, therefore, synthetic bone grafts are generally not recommended in treatment of osteomyelitis. The initial leaching of alkali and alkaline earth ions at the surface of the glass, leads to a rapid increase in pH around the glass. The high PH and the subsequent osmotic effect caused by dissolution of the glass have been suggested to partly explain the antibacterial properties observed for BAGs [25]. Comparing the in - vitro bactericidal effect, on 29 clinically important bac-teria, including methicillin resistant Staphylococcus aureus (MRSA), for several BAGs, BAG S53P4 has been shown to be the most effective, possessing the fastest killing or bacterial growth inhibitory effect [8]. In a multi-centre study, BAG S53P4 was used in the treatment of osteomyelitis with good or excellent results, i.e. patients that had been treated with long-lasting therapies responded well to the treatment [12]. The antibacterial and vascular promoting properties observed for BAG S53P4 may, therefore, be beneficial especially in primary treatment of severely injured patients, with a high risk of receiving a postoperative infection.
In conclusion BAG S53P4, compared to AB, is a safe and well-tolerated bone substitute showing comparably good long-term results in the hand. BAG S53P4, belonging to the group of third-generation bone substitutes, has proven bone bonding, osteostimulating and angiogenetic stimulating properties that are beneficial in bone reconstructive surgery. Since BAG S53P4 does not disturb the growth of bone in the hand in children it can, if needed, safely be used in treatment of bone tumours in children as well as in adults. The antibacterial properties observed exclusively in BAGs and the promising results using BAG S53P4 in treatment of osteomyelitis, also make BAG S53P4 a good material of choice in other applications in bone reconstructive surgery.
References
- Hench LL, Thompson I (2010) Twenty-first century challenges for biomaterials. J R Soc Interface 4: 5379-5391.
- Hench LL, Paschall HA (1973) Direct chemical bond of bioactive glass-ceramic materials to bone and muscle. J Biomed Mater Res Symp 4: 25-42.
- Hench LL, Wilson J (1984) Surface active biomaterials. Science 226: 630-635.
- Hench LL (1988) Bioactive ceramics. Ann N Y Acad Sci 523: 54-71.
- Andersson ÖH, Karlsson KH, Kangasniemi K (1990) Calcium phosphate formation at the surface of bioactive glass in vivo. J Non Cryst Solids 119: 290-296.
- Andersson ÖH, Kangasniemi I (1991) Calcium phosphate formation at the surface of bioactive glass in vitro. J Biomed Mater Res 24: 1019-1030.
- Leppäranta O, Vaahtio M, Peltola T, Zhang D, Hupa L, et al. (2008) Antibacterial effect of bioactive glasses on clinically important anaerobic bacteria in vitro. J Mater Sci: Mater Med 19: 547-51.
- Munukka E, Leppäranta O, Korkeamäki M, Vaahto M, Peltola T, et al. (2008) Bactericidal effects of bioactive glasses on clinically important aerobic bacteria. J Mater Sci Mater Res 19: 27-32.
- Day RM (2005) Bioactive glass stimulates the secretion of angiogenetic growth factors and angiogenesis in vitro. Tissue Eng 11: 768-777.
- Peltola MJ, Suonpää J, Aitasalo K, Määttänen H, Andersson Ö, et al. (2000) Clinical follow-up model for clinical frontal sinus obliteration with bioactive glass (S53P4). K Biomed Mater Res 58: 54-60.
- Lindfors NC, Heikkilä JT, Koski I, Mattila K, Aho J (2009) Bioactive glass and autogenous bone as bone graft substitutes in benign bone tumours. J Biomed Mater Res Appl Biomater 90:131-136.
- Lindfors NC, Hyvönen P, Nyyssönen M, Kirjavainen M, Kankare J, et al. (2010) Bioactive glass S53P4 as bone graft substi-tute in treatment of osteomyelitis. Bone 47: 212-218.
- Jubel A, Andermahr J, Mairhofer J, Prokop A, Hahn U, et al. (2004). Die anwendung des injizierbaren knochenzement Norian SRS bei tibiakopffrakture. Orthopäde 8: 919-927.
- Peltola MJ, Aitasalo KMJ, Suonpää JTK, Tli-Urpo A, Laippala PJ (2001) In vivo model for frontal sinus and calvarian bone defect obliteration with bioactive glass S53P4 and hydroxyapatite. J Biomed Mater Res Appl Biomater 58: 261- 269.
- Lindfors NC, Tallroth K, Aho AJ (2002) Bioactive glass as bone substitute for spinal fusion in rabbit. J Biomed Mater Res 63: 237-244.
- Hirn M, de Silva U, Sidharthan S, Grimer RJ, Abudu A, et al. (2009) Bone defects following curettage do not necessarily need augmentation. A retrospective study of 146 patients. Acta Orthop 80: 4-8.
- Athanasian EA (2004) Aneurysmal bone cyst and giant cell tumor of bone of the hand and distal radius. Hand Clinics 20: 269-281.
- Lindfors NC (2009) Treatment of a recurrent aneurysmal bone cyst with bioactive glass in a child allows for good re-modelling and growth. Bone 45: 398-400.
- Leu A, Leach LK (2008) Proangiogenic potential of a collagen/bioactive substrate. Phar Res 25: 1222-1229.
- Leach JK, Kaigler D, Wang Z, Krebsbach PH, Moonley DJ (2006) Coating of VEGF-releasing scaffolds with bioactive glass for angiogenesis and bone regeneration. Biomaterials 27: 3249-3255.
- Heikkilä JT, Kukkonen J, Aho AJ, Moisander S, Kyyrönen T, et al. (2011) Bioactive glass granules: a suitable bone substi-tute material in operative treatment of depressed tibial plateau fracture: a prospective, randomized 1 year followup. J mat Sci - mat Med 22: 1073-1080.
- Suominen E, Aho AJ, Vedel E, Kangasniemi I, Uusipaikka E, et al. (1996) Subchondral bone and cartilage repair with bio-active glasses, hydroxyapatite, and hydroxyapatite-glass composite. J Biomed Mater Res 32: 543-551.
- Ylänen HO, Helminen T, Helminen A, Rantakokko J, Karlsson KH, et al. (1999) Porous bioactive glass matrix in reconstruc-tion of articular osteochondral defects. Ann Chir Gyn 88: 237-245.
- Aho AJ, Tirri T, Kukkonen J, Strandberg N, Rich J, et al. (2004) Injectable bioactive glass/biodegradable polymer composite for bone and cartilage reconstruction: Concept and experimental outcome with thermoplastic composites of poly (e-caprolactone-co-D,L-lactide) and bioactive glass S53P4. J Mater Sci: Mater Med 15: 1165-1173.
- Stoor P, Söderling E, Salonen JI (1998) Antibacterial effects of a bioactive glass paste on oral microorganisms. Acta Odontol Scand 56: 161-165.
Relevant Topics
- Agricultural biotechnology
- Animal biotechnology
- Applied Biotechnology
- Biocatalysis
- Biofabrication
- Biomaterial implants
- Biomaterial-Based Drug Delivery Systems
- Bioprinting of Tissue Constructs
- Biotechnology applications
- Cardiovascular biomaterials
- CRISPR-Cas9 in Biotechnology
- Nano biotechnology
- Smart Biomaterials
- White/industrial biotechnology
Recommended Journals
Article Tools
Article Usage
- Total views: 16102
- [From(publication date):
August-2011 - Mar 31, 2025] - Breakdown by view type
- HTML page views : 11379
- PDF downloads : 4723