Cholera Outbreaks in Urban Bangladesh In 2011
Received: 12-Jun-2013 / Accepted Date: 28-Jun-2013 / Published Date: 02-Jul-2013 DOI: 10.4172/2161-1165.1000126
Abstract
Background:
In 2011, a multidisciplinary team investigated two diarrhoea outbreaks affecting urban Bangladeshi communities from the districts of Bogra and Kishorganj to identify etiology, pathways of transmission, and factors contributing to these outbreaks.
Methods:
We defined case-patients with severe diarrhoea as residents from affected communities admitted with ≥3 loose stools per day. We listed case-patients, interviewed and examined them, and collected rectal swabs. We visited the affected communities to explore the water and sanitation infrastructure. We tested the microbial load of water samples from selected case household taps, tube wells, and pump stations. We conducted anthropological investigations to understand community perceptions regarding the outbreaks.
Results:
We identified 21 case-patients from Bogra and 84 from Kishorganj. The median age in Bogra was 23 years, and 21 years in Kishorganj. There were no reported deaths. We isolated Vibrio in 29% (5/17) of rectal swabs from Bogra and in 40% (8/20) from Kishorganj. We found Vibrio in 1/8 tap water samples from Bogra and in both of the samples from Kishorganj. We did not find Vibrio in water samples from pumps or tube wells in either outbreak. Ground water extracted through deep tube wells was supplied intermittently through interconnected pipes without treatment in both areas. We found leakages in the water pipes in Bogra, and in Kishorganj water pipes passed through open sewers.
Conclusion:
The rapid onset of severe diarrhoea predominantly affecting adults and the isolation of cholera in rectal swabs confirmed that these outbreaks were caused by Vibrio cholerae. The detection of Vibrio in water samples organisms from taps but not from pumps or tube wells, suggested contamination within the pipes. Safe water provision is difficult in municipalities where supply is intermittent, and where pipes commonly leak. Research to develop and evaluate water purification strategies could identify appropriate approaches for ensuring safe drinking water in resourcepoor cities.
Keywords: Cholera, Outbreak, Urban, Bangladesh
160181Introduction
Vibrio cholera is responsible for approximately three to five million cases and an estimated 1,20,000 deaths per annum worldwide [1-3]. Cholera remains a major public health problem in many low income countries with poor access to safe water and proper sanitation, including Bangladesh [2,4]. Reports of cholera from Bangladesh have been commonly published in the scientific literature. However, cholera cases from Bangladesh were not reported to the World Health Organization until very recently [5-11]. Expert estimates suggest an occurrence of 4,50,000-1,000,000 cases of cholera in Bangladesh each year [3,8].
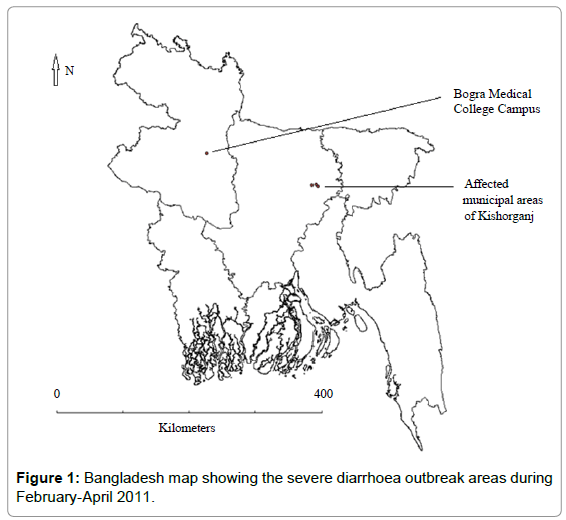
In 2011, a multidisciplinary team of epidemiologists, physicians, and anthropologists from the Institute of Epidemiology, Disease Control and Research (IEDCR) of the Government of the People’s Republic of Bangladesh (GoB), and the International Centre for Diarrheal Disease Research, Bangladesh (icddr,b) investigated two reported outbreaks of severe diarrhoea affecting urban communities in two districts of Bangladesh (Figure 1). The objectives of the outbreak investigations were to identify the etiology, determine the modes of transmission, explore the underlying factors, including environmental and socio-cultural contexts that contributed to these outbreaks, and to suggest control and prevention measures.
Methods
Outbreak reporting and investigations
On February 14, 2011, several national newspapers reported an outbreak of severe diarrhoea that led to the hospitalization of more than 20 patients in the government tertiary-care hospital in the northwestern district of Bogra. The outbreak affected medical and nursing students, faculty members, clinical and administrative staff and their family members living in hostels and households within the large campus of the teaching hospital and nursing college on the city outskirts. On April 18, 2011, newspapers reported a similar outbreak affecting the residents of three municipal wards within the catchment of the Kishoganj District Hospital, the government secondary-care hospital, located in the urban sub-district of Kishorganj District in northeast Bangladesh. Both outbreaks were reported in several local and national newspapers and the local health authorities requested assistance from IEDCR to determine the causes to better respond to these outbreaks. Within 24 hours of receiving the request, the collaborative team from IEDCR and icddr,b traveled to the outbreak site and collected epidemiological, environmental, and anthropological information.
Epidemiological investigation
During both outbreak investigations, the team collected preliminary information from the district health managers (i.e. civil surgeons) regarding general socioeconomic status, sources of drinking water and sanitation facilities of residents of the affected communities. The team conducted field investigation in Bogra on February 15-16, 2011, and in Kishorganj on April 19-20, 2011. To determine the clinical features and investigate possible etiology, team physicians interviewed the caregivers and the admitted diarrhoea patients with the earliest date of onset of illness. The team also conducted group discussions with health officials including the resident medical officers, nurses and paramedics providing care to affected patients to understand the nature of the illness.
The team identified and listed case-patients with severe diarrhoea defined as any resident from the affected areas with three or more loose stools in 24 hours and admitted to the hospital in the three days prior to the reporting of the outbreaks from Bogra on February 14, 2011 and from Kishorganj on April 18, 2011. The team used a pretested standardized case investigation form to collect clinical histories and exposure information from all case-patients admitted during the two-days of field investigation in either outbreak. Team physicians examined the case-patients and recorded their clinical signs. The health workers from the affected municipalities looked for additional severe acute diarrhoea cases or deaths in the communities by household visits and reported them to the civil surgeon. The team requested the civil surgeon to report to IEDCR any additional diarrhoea admissions and/ or deaths on a daily basis for one week after the field investigation.
Laboratory investigation
Medical technologists in the team collected rectal swabs in bacterial transport media from case-patients who consented to provide a sample. Rectal swabs were cultured and tested for Vibrio cholerae subtypes, Shigella spp., and Salmonella spp. in IEDCR’s Microbiology Laboratory using established methods [12-14]. The isolates were tested for susceptibility to commonly prescribed antibiotics using the agar disk diffusion method [15,16].
Environmental investigation
The team conducted unstructured interviews with purposively selected health workers, local leaders, and the chief engineers of the Department of Public Health Engineering (DPHE) from the affected districts to collect information regarding the local water supply and sanitation. The local health workers identified all the case-patients’ households that had at least three additional members suffering from diarrhoea. During both outbreaks, field investigators visited these casepatients’ households and collected water samples from household taps. Among these households that had a shallow tube well, field investigators collected water samples from household tube wells. In either outbreak area, water samples were also collected from the municipal pump and the central pumping station to test for Vibrio cholerae subtypes and indicator bacteria including total coliforms, faecal coliforms, Salmonella, Shigella, Pseudomonas spp., and Aeromonas spp. All water samples were stored in a cool box maintained at 4-8°C. The samples were transported within 24 hours of collection and analyzed in icddr,b’s Environmental Microbiology Laboratory.
Anthropological investigation
To understand the community perceptions regarding the cause of the outbreak and to explore community practices regarding sources and usage of water, the team visited the hospital campus in Bogra and the affected wards in Kishorganj. In Bogra, the team conducted a group discussion with 12 community residents, and team members talked to seven community residents in Kishorganj to explore their perceptions regarding the cause and the transmission of illness. In both outbreak areas, team members visited those case-patient households identified by the local health workers to have three additional members suffering from diarrhoea. The team also conducted open discussions with members in these households to learn about their perceptions regarding cause of the outbreak and preventive measures including water purification strategies. To learn about their healthcare seeking behavior, the team conducted in-depth interviews with four casepatients including the index case-patient in either outbreak. To learn about the healthcare providers’ perceptions regarding the cause of outbreak and gaps in clinical management, the team interviewed three key informants from either hospital including the principal, head of the department, and the registrar of the Department of Medicine from the hospital in Bogra, and the civil surgeon, the resident medical officer and the senior staff nurse in Kishorganj.
Data analysis
We analyzed quantitative data by using SPSS version 12.0 and generated descriptive statistics to calculate frequencies. We reviewed the qualitative data to identify common themes and developed a code list using the identified themes. We summarized coded data according to the objectives of the investigations.
Ethical considerations
We obtained informed oral consent from adult respondents and guardians and assent from children respondents 11–17 years of age. This investigation was exempted from review by an independent human subjects committee since it was an emergency response investigation. The investigation was conducted in response to an outbreak that was approved by and conducted in collaboration with the Ministry of Health and Family Welfare.
Results
Descriptive findings
The team identified 21 case-patients admitted from February 11–14, 2011, to the tertiary-care hospital in Bogra, and 84 casepatients admitted to the secondary-care hospital from April 15–19, 2011, in Kishorganj. Among these, 38% (8/22) from Bogra and 52% (44/84) from Kishorganj were males. The median age was 23 years (Interquartile range, IQR: 18–35 years) in Bogra and 21 years (IQR, 15–33 years) in Kishorganj. There were no reported deaths.
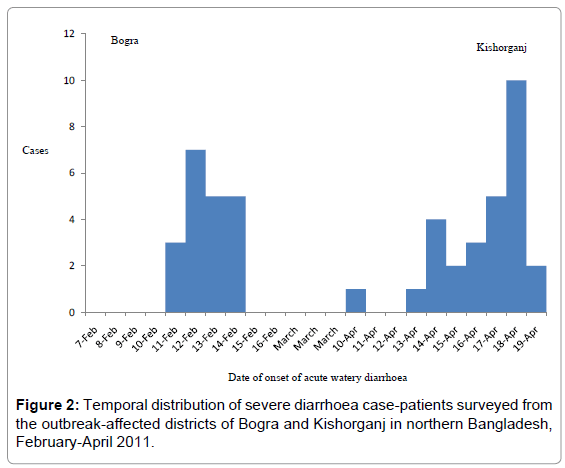
We surveyed 20 case-patients admitted to the hospital in Bogra during the field investigation from February 15-16, 2011 and 28 casepatients admitted to the hospital in Kishorganj from April 19-20, 2011 (Figure 2). Ninety percent (18/20) of the case-patients from Bogra and 79% (22/28) of the case-patients from Kishorganj were admitted to the hospital within 24 hours of onset of symptoms. Almost all interviewed cases reported sudden onset of acute watery diarrhoea that later became mixed with mucous. Based on the diarrhoea treatment guideline of the World Health Organization (WHO), the attending physician classified 29% of case-patients from Bogra and 25% of casepatients from Kishorganj as having ‘severe dehydration’ at the time of admission. In Bogra, 3 out of the 20 surveyed case-patients (15%) reported no urination for at least 12 hours and two out of 20 (10%) reported scanty urination. According to hospital records, 5 out of 20 case-patients (25%) in Bogra had developed features of acute renal failure, characterized by a raised serum creatinine level, no urination for 12 hours or scanty urination, and high serum potassium level, within 24 hours of admission (Table 1). However, physicians reported that all 5 case-patients with features of acute renal failure had improved on their renal function after infusion of intravenous rehydration solution and antibiotics.
| Variables | Number of case-patients in Bogra, (%) N=20 | Number of case-patients in Kishorganj, (%) N=28 |
|---|---|---|
| Clinical presentations | ||
| Acute watery diarrhoea (passage of ≥3 loose stools per day) | 19 (95) | 28 (100) |
| Passing watery stools continuously in first 24 hours | 12 (60) | 14 (50) |
| Abdominal cramps | 5 (25) | 11 (39) |
| Vomiting | 11 (55) | 21 (75) |
| Severe dehydration | 5 (25) | 8 (29) |
| Some dehydration | 11 (55) | 15 (53) |
| No dehydration | 4 (20) | 5 (18) |
| No urination for 12 hours | 3 (15) | 0 (0) |
| Scanty urination | 2 (10) | 2 (7) |
| Acute renal failure (Raised serum creatinine, anuria or oliguria and hyperkalaemia) | 5 (25) | 0 (0) |
| Additional features | ||
| Had at least one other household member affected with similar features | 11 (55) | 19 (68) |
| Two or more household members affected | 6 (30) | 12 (43) |
| Clinical management | ||
| Rehydration with intravenous cholera saline infusion | 16 (80) | 23 (82) |
| Rehydration with oral rehydration salts | 4 (20) | 5 (18) |
| Received at least one antibiotic within 24 hours of illness onset | 18 (90) | 23 (82) |
| Received ≥2 antibiotics in the course of therapy | 11 (55) | 12 (43) |
| Clinical outcome | ||
| Death | 0 (0) | 0 (0) |
| Water use practice | ||
| Drank only municipal tap water | 10 (50) | 9 (32) |
| Drank only tube well water | 5 (25) | 14 (50) |
| Drank both tap and tube well water | 5 (25) | 5 (18) |
| Used tap water for washing foods and utensils, and cooking | 20 (100) | 15 (54) |
| Boiled or chemically purified drinking water | 0 (0) | 1 (4) |
Table 1: Clinical presentation, management, clinical outcome and water use practice of case-patients admitted with severe acute diarrhoea in Shaheed Ziaur Rahman Medical College Hospital, Bogra, February and Kishorganj District Hospital, April 2011.
Laboratory findings
Vibrio cholerae Ogawa was isolated from 29% (5/17) of the rectal swab samples collected from Bogra and from 40% (8/20) rectal swab samples collected from Kishorganj. All the Vibrio cholerae samples from Bogra were resistant to nitrofurantoin, tetracycline, nalidixic acid, erythromycin, ampicillin and ceftriaxone but sensitive to ciprofloxacin, azythromycin and doxycycline. The Vibrio cholerae samples from Kishorganj were fully resistant to tetracycline and nalidixic acid but highly sensitive to nitrofurantion, ciprofloxacin, azithromycin, ampicillin, cefuroxime, ceftriaxone and doxycycline, and moderately sensitive to erythromycin.
Environmental findings
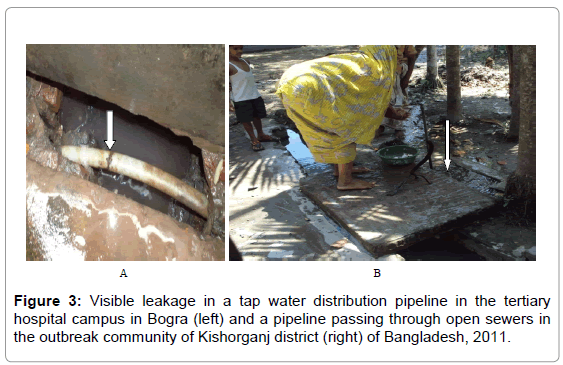
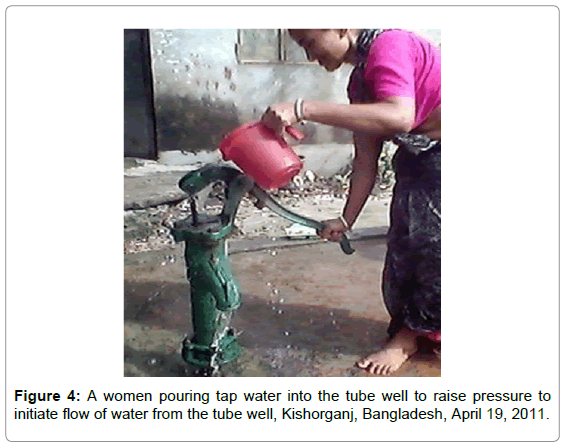
In both outbreak affected districts, ground water was extracted from deep tube wells installed by the Department of Public Health Engineering under the Ministry of Health and Family Welfare of the government. The deep tube well in the central pump station, the municipal pumps and the distribution pipes were maintained by the municipal authority under the Ministry of Local Government and Rural Development. In both districts, extracted ground water was not treated and was distributed to households through an interconnected piped system. Tap water was supplied intermittently for about one and a half hours three times daily. Key informants in Bogra reported that the hospital compound was built on more than 400 acres of land that included a 500-bed hospital, medical and nursing colleges, students and faculty hostels, staff quarters, mosques, and a primary school. The hospital compound had a separate pump station that supplied water to the hospital compound through an interconnected piped system. According to the principal of the tertiary-care hospital in Bogra, the pipes had recently developed several leakages. Key informants in Kishorganj reported that the municipality had recently repaired the pump that supplied the affected communities, which had not been functioning for about three months. Following the repair operation, the municipality neither cleaned the pipes nor treated the water. Field investigators observed visible leaks in a pipe in Bogra (Figure 3A). The team did not find any visible leaks in the pipes in Kishorganj, however the pipes and tube wells were in close proximity to toilets and sewers. Moreover, the water pipes passed through open sewers in some areas (Figure 3B). During the summer season, the water table in Kishorganj often lowered, greatly reducing the water supply from the tube wells. Community residents reported frequently having to pour 2-3 litres of municipal tap water into the tube wells to raise pressure and initiate water flow (Figure 4).
We isolated Vibrio cholerae O1 (Ogawa) from one of the eight tap water samples that were collected from Bogra. In Kishorganj, we isolated Vibrio cholerae O1 (Ogawa) from both the municipal tap water samples. We did not find cholera organisms in the water samples from the central pump stations, municipal pumps or the tube wells in either outbreak sites. Total coliforms were isolated from six of the nine water samples and faecal coliforms were isolated from five out of the nine tap water samples (Table 2).
| Points of water collection from Bogra (B) and Kishorganj (K) | Number of samples exceeding the maximum allowable limits1,(Range of organisms) | ||||||
|---|---|---|---|---|---|---|---|
| Total coliforms | Faecal coliforms | Vibrio cholerae | Aeromonas spp. | Pseudomonas spp. | Salmonella/Shigella Spp. | ||
| Tube well | B (N=2) |
1 (0-500) | 1 (0-1000) | 0 (0) | Not done2 | Not done2 | Not done2 |
| K (N=2) |
2; (0-2000) | 2 (0-1000) | 0 (0) | 2 (1) | ; (1) | 0 (0) | |
| Tap | B (N=8) |
8 (4-60000) | 6 (0-32000) | 1 (V. Cholerae 01 Ogawa) | Not done2 | Not done2 | Not done2 |
| K (N=2) |
2 (130-176000) | 2 (147-77000) | 2 (V. Cholerae 01 Ogawa) | 2 (1) | 1 (1) | 0 (0) | |
| Municipal pump | B N=1) |
1 (5) | 0 (0) | 0 (0) | 1 (1) | 0 (0) | 0 (0) |
| K (N=1) |
1 (8) | 0 (0) | 0 (0) | 1 (1) | 0 (0) | 0 (0) | |
| Central pump | B | Not done2 | Not done2 | Not done2 | Not done2 | Not done2 | Not done2 |
| K N=1) |
1 (252) | 1 (105) | 0 (0) | 1 (1) | 1 (1) | 0 (0) | |
1Maximum allowable limit by World Health Organization’s Guideline is 0 CFU/100 ml for the following organisms: (Total coliforms, faecal coliforms, Vibrio cholerae, Aeromonas spp., Salmonella spp., Shigella spp., Pseudomonas spp.)
2Not done: the quantity of samples were insufficient for these tests
Table 2: Bacteriological test results of water samples collected from various sources from diarrhoea outbreak affected communities in Bogra and Kishorganj districts of Bangladesh during February and April 2011.
Anthropological findings
Perceptions of cause and transmission of illness: The physicians, hospital staff and the community residents in Bogra perceived drinking water contamination as the source of the diarrhoea outbreak. Five community residents perceived the visible leaks in the pipes to be primarily responsible for water contamination. Perceptions of community residents regarding the cause of the illness outbreak in Kishorganj included a recent heat wave (4/7) and an increased number of flies in households following insecticide spraying of the open sewers by the municipality (3/7). Two case-patients and 4/9 members from affected households perceived that the dirty and smelly water from the taps of the recently repaired municipal pump could have caused the illness. One household member, who was a municipal worker, further explained that the common municipal pump for the three affected wards in Kishorganj was repaired one week before the outbreak as it had not been functional for the preceding three months.
Perceptions on drinking water purification: All community residents from both outbreaks knew about the water purification strategies including boiling and chlorination. However, none of them regarded it necessary to actually boil or chemically purify drinking water.
One community resident from Bogra expressed, “There is no need to boil or add chlorine to the tap water since the taps only supply the ground water pulled out by the deep tube wells, and we all know that the ground water is always pure and has no germs.”
Three out of the seven community residents and 2/9 household members from Kishorganj felt that the drinking water became dead (stale) and tasteless after boiling. Two elderly household members from Kishorganj expressed their dislike regarding chemical purification of drinking water as chlorinated water tasted bitter.
Healthcare seeking behaviour: All eight case-patients reported that they had tried oral rehydration saline solution at home to manage the illness initially. However, all case-patients from Bogra Kishorganj sought medical care when their clinical conditions did not improve within a day.
Physicians’ concerns regarding cholera management and response: When asked regarding the five case-patients who developed features of acute renal failure within 24 hours of admission, the tertiary hospital physicians explained that the cases of acute renal failure probably resulted from reduced body fluids and consequent hypovolemic shock in those rapidly dehydrating case-patients. They explained that the rate of rehydration with intravenous fluid was insufficient to rehydrate the fluid lost due to the continuous watery stools. To ensure appropriate management of the case-patients, the hospital physicians expressed the need for regular re-orientation or training on the management guidelines for severe acute watery diarrhoea, including cholera. Physicians also reported a shortage of necessary antibiotics and rice-based oral rehydration salts. However, oral rehydration salts and intravenous saline solution were available in the hospitals.
Discussion
The sudden onset of severe watery diarrhoea predominantly affecting adults and the isolation of pathogenic strains of cholera organisms in 29% of the collected rectal swab samples from Bogra and in 40% of the rectal swab samples from Kishorganj confirm that both outbreaks were caused by Vibrio cholerae. The sudden outbreak of severe diarrhoea among the residents living in a tertiary hospital campus with a common water supply system that had visible leakages in the pipes suggested contaminated water was the source of the outbreak in Bogra. The occurrence of cholera among the residents of three municipal wards with a common municipal pump and interconnected water pipes that passed through sewers also suggested water was the most likely source in Kishorganj. In addition, the heat wave possibly increased the concentration of cholera organisms in the aquatic environments of Kishorganj since high environmental temperatures can promote growth and multiplication of Vibrio cholerae [17,18]. The detection of cholera organisms in the water samples collected from household taps but not from the pump stations and tube wells suggests that contamination occurred within the pipes in both outbreaks. Investigation reports of two recent cholera outbreaks detected in urban communities of two Bangladeshi districts with similar water supply system also implicated contaminated piped water as the outbreak source [19-21].
Although half of the affected case-patients surveyed from Bogra and one-third of the case-patients from Kishorganj reported drinking tube well water exclusively, all case-patients from Bogra and more than half (54%) of the case-patients from Kishorganj reported using municipal tap water for household and personal purposes including washing foods, washing utensils and bathing. Moreover, water contaminated with cholera organisms can cross-contaminate fruits, vegetables, semicooked and other raw foods [22]. In addition, household tube well water may also get contaminated with cholera organisms from tap water while priming the pump for drawing water from the tube wells.
The public health burden of cholera is significant in developing countries including Bangladesh [2]. Cholera is a notifiable disease under the International Health Regulations [23]. Yet, only five cholera outbreaks have been investigated and reported during the last five years through the governmental system in Bangladesh [20]. In contrast, several publications in international and national journals including the quarterly publication, Health and Science Bulletin of icddr,b have frequently reported thousands of cholera cases from the two icddr,b hospitals in Dhaka and Matlab [19,24-30]. Unlike several previous cholera outbreaks we found no deaths during these outbreaks [19,20]. The close proximity of the affected areas to hospitals and the majority of the case-patients seeking health care from hospital practitioners likely facilitated prompt and appropriate management. This assisted the recovery of cholera affected patients and resulted in no associated mortality. On the other hand, our hospital-based case finding efforts may have failed to detect deaths due to cholera within the communities.
Diarrhoeal diseases cause significant mortality and morbidity in the country [27]. The World Health Organization recommends chlorination of piped water and boiling or chemical treatment of drinking water at home for prevention of outbreaks of enteric infections in urban Bangladeshi communities [31-33]. However, the piped water was not chemically treated nor was the drinking water boiled and/or chemically purified at home during both outbreaks despite the knowledge of community residents about drinking water purification strategies. This prevailing low risk perception in Bangladeshi communities regarding water safety might translate into less pressure on governmental authorities to address water purification issues, which, in turn puts communities at ongoing risk for outbreaks of water borne illnesses.
There are several limitations in these investigations. The estimated burden of cholera cases detected in these outbreaks is likely an underestimate. Since we did not conduct a house-to-house search in either outbreak community, we might have failed to detect milder cases and deaths related to cholera within the communities. Moreover, in approximately half of the identified case-patients, two or more family members also suffered similar symptoms. This suggested that the total community burden of cholera was likely to have been greater than only the hospitalized case-patients. Systematically conducted houseto- house surveys to estimate mortality rates associated with epidemic transmission of cholera, along with verbal autopsies and identification of risk factors for deaths would help determine the true public health impact of cholera outbreaks.
Within the health sector, the successful containment and control of cholera outbreaks require an integrated approach including prompt outbreak investigation, adequate laboratory facilities for isolation and detection of microbial resistance, availability of rehydration solutions and antibiotics, and adequately trained professionals at all levels of healthcare. Given the large population of approximately 160 million exposed to an increasing risk of cholera due to poor sanitation and water hygiene infrastructure, and limited access to healthcare, mass vaccination should be explored to prevent cases of cholera and deaths in Bangladesh. Several randomized controlled trials have shown that the modified killed-whole-cell oral vaccine is compliant with WHO standards and can provide protection against clinically significant cholera in endemic settings [34-37]. However, the protection against cholera is incomplete and persists for up to two years following a single dose of vaccine, and for three to four years with an annual booster thereby requiring repeated vaccination [38]. Beyond the health sector, the Department of Public Health Engineering and municipal authorities should avoid placing water distribution pipes near sewerage lines and consider chlorination of piped water before delivery to households.
Averting cholera transmission ultimately requires providing safe drinking water to city dwellers through a well maintained water and sanitary infrastructure. However, safe water delivery is difficult in cities where water supply is intermittent and pipelines commonly leak. Cholera prevention needs to reach beyond the health sector in order to improve water and sanitary infrastructure. This will require collaborative actions by many departments within and outside of the health sector which may be difficult to achieve in a resource-poor setting. Collaborative multi-disciplinary research should explore and evaluate new approaches to providing microbiologically safe drinking water in smaller municipalities with intermittent water supply. In addition to seeking innovative solutions, known water purification strategies such as chlorination targeted after risky contexts for contamination including pipeline repair operations may also provide feasible, low-cost solutions. Improved surveillance for cholera by the government health sector could detect outbreaks more frequently. The cholera outbreak investigation reports should be shared with different stakeholders including the local government, water and sanitation authorities, the media, and international agencies dealing with the health of the people. This could help focus more attention on steps that need to be taken outside of the health sector to reduce the burden of cholera in Bangladesh.
Acknowledgements
This investigation was funded by the United States Centers for Disease Control and Prevention (CDC) and the Government of Bangladesh. icddr,b acknowledges with gratitude the commitment of the Government of Bangladesh and CDC to the centre’s research efforts. The authors would like to thank all the study participants for their contribution. We are also grateful to the principal and the director of Shaheed Ziaur Rahman Medical College Hospital, and the civil surgeons of Bogra and Kishorganj districts for their support in conducting the field investigations. Diana DiazGranados and James Heffelfinger deserve special thanks for their contributions in reviewing the manuscript.
Funding
This investigation was funded by the Centers for Disease Control and Prevention (CDC), Atlanta, Georgia, USA and the Government of the People’s Republic of Bangladesh. icddr,b acknowledges with gratitude the commitment of the Government of Bangladesh and the CDC to its research efforts.
Ethical Approval
This investigation was conducted in response to an outbreak and was approved by and conducted in collaboration with the Government of the People’s Republic of Bangladesh. As this investigation was an emergency response, the activity was not reviewed by an independent human subjects committee. However, verbal informed consent was sought from all participants.
Poster presentation at the 61st ASTMH annual meeting and winner of Travel Award
Name of conference: Poster Number # 753 at the 61st Annual Meeting of the American Society of Tropical Medicine and Hygiene (ASTMH), November 11-15, 2012, Marriot Marquis and Hilton Hotel, Atlanta, Georgia, USA. The first author also won a Bill and Melinda Gates Foundation funded Travel Award for this abstract.
References
- Ali M, Lopez AL, You YA, Kim YE, Sah B, et al. (2012) The global burden of cholera. Bull World Health Organ 90: 209-218A.
- Sánchez J, Holmgren J (2005) Virulence factors, pathogenesis and vaccine protection in cholera and ETEC diarrhea. Curr Opin Immunol 17: 388-398.
- Hashizume M, Armstrong B, Hajat S, Wagatsuma Y, Faruque AS, et al. (2008) The effect of rainfall on the incidence of cholera in Bangladesh. Epidemiology 19: 103-110.
- Hashizume M, Faruque AS, Terao T, Yunus M, Streatfield K, et al. (2011) The Indian Ocean dipole and cholera incidence in Bangladesh: a time-series analysis. Environ Health Perspect 119: 239-244.
- Hashizume M, Faruque AS, Wagatsuma Y, Hayashi T, Armstrong B (2010) Cholera in Bangladesh: climatic components of seasonal variation. Epidemiology 21: 706-710.
- Rahman, M (2011) Cholera burden in Bangladesh, in Introduction to cholera vaccine,Bangladesh. Sasakawa Auditorium, Dhaka.
- Keusch GT, Fontaine O, Bhargava A, Boschi-Pinto C, Bhutta ZA, et al. (2006) Diarrheal Diseases.
- Koelle K, Rodó X, Pascual M, Yunus M, Mostafa G (2005) Refractory periods and climate forcing in cholera dynamics. Nature 436: 696-700.
- Lipp EK, Huq A, Colwell RR (2002) Effects of global climate on infectious disease: the cholera model. Clin Microbiol Rev 15: 757-770.
- Hanumanthappa AR, Rajagopal V (2001) Rapid diagnosis of cholera by coagglutination test. Indian J Pathol Microbiol 44: 123-124.
- Qadri F, Azim T, Chowdhury A, Hossain J, Sack RB, et al. (1994) Production, characterization, and application of monoclonal antibodies to Vibrio cholerae O139 synonym Bengal. Clin Diagn Lab Immunol 1: 51-54.
- Rahman M, Sack DA, Mahmood S, Hossain A (1987) Rapid diagnosis of cholera by coagglutination test using 4-h fecal enrichment cultures. J Clin Microbiol 25: 2204-2206.
- Murray, P., et al., eds. Antibacterial susceptibility tests: dilution and disk diffusion methods. 7 ed. Manual of clinical microbiology, ed. J. Jorgensen, J. Turnidge, and J. Washington. 1999, ASM Press: Washington, DC. 1526-1543.
- Perilla MJ (2003) Bacterial Agents of Enteric Diseases of Public Health Concern: Vibrio cholerae identification and antimicrobial susceptibility testing. World Health Organization: Department of Communicable Disease Surveillance and Response: Geneva. 141-159.
- Hashizume M, Armstrong B, Hajat S, Wagatsuma Y, Faruque AS, et al. (2007) Association between climate variability and hospital visits for non-cholera diarrhoea in Bangladesh: effects and vulnerable groups. Int J Epidemiol 36: 1030-1037.
- Huq A, Sack RB, Nizam A, Longini IM, Nair GB, et al. (2005) Critical factors influencing the occurrence of Vibrio cholerae in the environment of Bangladesh. Appl Environ Microbiol 71: 4645-4654.
- icddrb, (2010) Cholera outbreak in Pabna. Health and Science Bulletin 8: 6-11.
- Sur D, Sarkar BL, Manna B, Deen J, Datta S, et al. (2006) Epidemiological, microbiological & electron microscopic study of a cholera outbreak in a Kolkata slum community. Indian J Med Res 123: 31-36.
- WHO (2011) Water-related diseases: cholera. Water Sanitation and Health (WSH)
- MÃnguez Gonzalo M (2007) [The New International Health Regulations (2005 IHR)]. Rev Esp Salud Publica 81: 239-246.
- Clemens JD, Harris JR, Sack DA, Chakraborty J, Ahmed F, et al. (1988) Field trial of oral cholera vaccines in Bangladesh: results of one year of follow-up. J Infect Dis 158: 60-69.
- Clemens JD, Sack DA, Harris JR, Van Loon F, Chakraborty J, et al. (1990) Field trial of oral cholera vaccines in Bangladesh: results from three-year follow-up. Lancet 335: 270-273.
- Glass RI, Becker S, Huq MI, Stoll BJ, Khan MU, et al. (1982) Endemic cholera in rural Bangladesh, 1966-1980. Am J Epidemiol 116: 959-970.
- Icddrb (2002) Trends in aetiologies for diarrhoeal diseases. Health and Science Bulletin. 1: 12-15.
- Sack RB, Siddique AK, Longini IM Jr, Nizam A, Yunus M, et al. (2003) A 4-year study of the epidemiology of Vibrio cholerae in four rural areas of Bangladesh. J Infect Dis 187: 96-101.
- van Loon FP, Clemens JD, Chakraborty J, Rao MR, Kay BA, et al. (1996) Field trial of inactivated oral cholera vaccines in Bangladesh: results from 5 years of follow-up. Vaccine 14: 162-166.
- Galal-Gorchev H, Ozolins G, Bonnefoy X (1993) Revision of the WHO guidelines for drinking water quality. Ann Ist Super Sanita 29: 335-345.
- Gorchev HG, Ozolins G (1984) WHO guidelines for drinking-water quality. WHO Chron 38: 104-108.
- Malloy CD, Marr JS (2001) Evolution of the Control of Communicable Diseases Manual: 1917 to 2000. J Public Health Manag Pract 7: 97-104.
- Graves P, Deeks J, Demicheli V, Pratt M, Jefferson T (2000) Vaccines for preventing cholera. Cochrane Database Syst Rev 4: CD000974.
- Sinclair D, Abba K, Zaman K, Qadri F, Graves PM (2011) Oral vaccines for preventing cholera. Cochrane Database Syst Rev : CD008603.
- Sur D, Lopez AL, Kanungo S, Paisley A, Manna B, et al. (2009) Efficacy and safety of a modified killed-whole-cell oral cholera vaccine in India: an interim analysis of a cluster-randomised, double-blind, placebo-controlled trial. Lancet 374: 1694-1702.
- Graves P, Deeks J, Demicheli V, Pratt M, Jefferson T (2000) Vaccines for preventing cholera. Cochrane Database Syst Rev 2: CD000974.
- Graves PM, Deeks JJ, Demicheli V, Jefferson T (2010) Vaccines for preventing cholera: killed whole cell or other subunit vaccines (injected). Cochrane Database Syst Rev : CD000974.
Citation: Haque F, Hossain MJ, Kundu SK, Naser AM, Rahman M, et al. (2013) Cholera Outbreaks in Urban Bangladesh In 2011. Epidemiol 3:126. DOI: 10.4172/2161-1165.1000126
Copyright: © 2013 Haque F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 16330
- [From(publication date): 6-2013 - Mar 31, 2025]
- Breakdown by view type
- HTML page views: 11526
- PDF downloads: 4804