Research Article Open Access
Attitudes and Beliefs of Consumers of Herbal Medicines in Riyadh, Saudi Arabia
Amal K Suleiman*
Clinical Pharmacy Department, Princess Nora Bint Abdulrahman University, Saudi Arabia
- *Corresponding Author:
- Amal K. Suleiman
Assistant Professor, Clinical Pharmacy Department
Princess Nora bint Abdulrahman University, P.O. Box 84428
Riyadh 11671, Saudi Arabia
Tel: +966 565 315 541
E-mail: albarqok@yahoo.com
Received date: January 07, 2014; Accepted date: January 22, 2014; Published date: January 24, 2014
Citation: Suleiman AK (2014) Attitudes and Beliefs of Consumers of Herbal Medicines in Riyadh, Saudi Arabia. J Community Med Health Educ 4: 269. doi: 10.4172/2161-0711.1000269
Copyright: © 2014 Suleiman AK. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Background: Herbal medicines are commonly used in Saudi Arabia alongside conventional drug therapy. However, special attention must be paid when using such medicines and supplements with other drugs. Objective: This study was designed to evaluate the consumer awareness surrounding herbal remedies and the safety of herbal dietary supplements, as well as the sources of recommendation for their use and common beliefs regarding the combining herbals and drugs during therapy. Materials and methods: A self-administered questionnaire was used to capture data from 420 participants that purchased herbal medicines and/or herbal dietary supplements based on convenience sampling method from seven private pharmacies in Riyadh during 2013. The questionnaire included four parts: the socio-demographic characteristics of the consumer, the source of recommendation for the use of the purchased herbal products, the consumer’s attitude towards the safety of herbal remedies and herbal dietary supplements and their combination with conventional drugs, and assessment of the purchased herbal products. The data from each of the returned questionnaire were coded and entered into (SPSS) version 15.0 software which was used for statistical analysis. Response rate was 70%. The majority of participants were highly educated. Result: The study results show that 91.1% of the participants did not consult or take advice from a pharmacist or physician prior to purchasing herbal remedies for concurrent use alongside conventional medication. The study shows 8.8% used herbal medicines or herbal dietary supplements following advice from a physician or pharmacist, 66.2% of them on their friends or relatives, while 24.9% was based on the independent internet research, advertisements, etc. According to the study results, 81.2% believed that herbal medicines and herbal dietary supplements are harmless; however, 49.5% of participants acknowledged that combining herbal remedies and conventional drugs may be unsafe. Conclusion: This study demonstrates that public awareness regarding the use of herbal medicines and supplements, especially alongside other medication, is lacking. It is the responsibility of pharmacists and physicians to provide patients with comprehensive advice regarding the use of herbal medicines and herbal dietary supplements to ensure their safe use.
Keywords
Herbal medicines; Herbal dietary supplements; Conventional drugs; Riyadh; Consumer awareness
Introduction
Herbal medicine is used as the primary source of healthcare for approximately 75-80% of the world population and its use is particularly widespread in the developing countries, where it is considered more culturally acceptable, less dangerous and a more natural form of medicine that is compatible with the human body. Herbal products are defined as “herbal preparations produced by subjecting herbal materials to extraction, fractionation, purification concentration, or other physical or biological processes. They may be produced for immediate consumption or as the basis for herbal products. Herbal products may contain excipients or inert ingredients, in addition to the active ingredients they are generally produced in larger quantities for the purpose of retail sales” [1]. However, there is no specific definition or classification for herbal medicines. This is not surprising given their diversity as herbal medicines are chemically rich preparations of, essentially, any plant material.
‘Complementary medicine’ can be utilized to identify a range of pharmaceutical-type preparations, inclusive HMs, homoeopathic remedies, essential oils and dietary supplements [2]. This statement was corroborated by Samojlik et al. [3], who additionally found that HMs are used in the modern day for health maintenance, the treatment or prevention of minor ailments and some chronic diseases, and they are often taken in addition to conventional medicine in the more serious and/or chronic conditions. However, complementary medicine, including herbal remedies, is certainly not a modern day phenomenon and has historically been used in the pharmacological treatment of disease [4], when it may have more commonly been known as traditional folk healing.
Much of the population in developing countries still relies on traditional medicine practitioners and their collection of medicinal plants to meet all manner of healthcare needs. In developed countries modern medicine may exist alongside more traditional practices, with HM maintaining its popularity for historical and cultural reasons. Interestingly, the last few years have seen a substantial increase in the use of HMs in the developed world. In this regard, Cavaliere et al. [5] found that, in the USA alone, 4.8 billion dollars was spent on various HMs and dietary supplements. However, in the USA most herbal products are marketed as dietary supplements and are thus not regulated in the same way as drugs since supplements do not require pre-approval on the basis of, for example, efficacy. The out of pocket expenditure associated with the use of herbal medicines was estimated to amount to £31 million in the United Kingdom [6], £1 billion in Germany [7].
Another important issue arises when the terminology, regulatory status and categorization of herbal products is considered. More specifically, in the USA herbs can be defined as drugs, foods or dietary supplements. The Dietary Supplement Health and Education Act of 1994 (DSHEA) defined a dietary supplement as a substance intended to supplement the diet that is not represented by a conventional food group. Herbs and other botanicals and their extracts or concentrates were specifically mentioned as being dietary supplements.
Samojlik et al. [3] found that, in almost all European Union (EU) member states, HMs are considered medicinal products and include plants, parts of plants and plant preparations. In the majority of cases the HMs are presented with therapeutic or medical claims. Furthermore, in some cases, the same herb may be simultaneously available as a drug, herbal product and food supplement, making the regulation of herbal products somewhat complex. Potentially hazardous plants are controlled and are designated as prescriptiononly medicines (POMs) and others are subject to dose and route of administration restrictions; however, the duration of treatment with these herbs is not controlled. Other herbs can be obtained only from a pharmacy under the supervision of a pharmacist [8].
Cooperman et al. [9] have previously concluded that the safety, quality, and efficacy of HMs and herbal dietary supplements (HDS) (i.e., herbal medicines with added vitamins or minerals) are a result of their active ingredients, but these products can contain other active ingredients that have unexpected consequences. Furthermore, Bozin et al. [10] found that the chemical composition of medicinal herbs, and the derived HMs and HDS, count on several biological factors (e.g., the part of the plant used, the stage of growth at the point of harvest and the growth conditions). Accordingly, Samojlik et al. [3] proposed that all herbal products must be described as complex pharmaceutical products. Moreover, Williamson et al. [11] showed that, worldwide, around 80% of HM consumers rely on the advice of friends regarding the use of such remedies and only 25% consulted their physician prior to the administration of HMs to their children.
In Saudi Arabia the registration of medicinal products with the Ministry of Health is obligatory, as is the registration of products that make medicinal claims or contain active ingredients that may exhibit medicinal effects, such as herbal preparations, health and food supplements, medicated cosmetics, antiseptics, and medical devices [12]. The use of herbal remedies is very common in Saudi Arabia is no exception to it. Anecdotally, it is thought that herbal products are popular as a result of a widespread belief that the preparations are natural and therefore safe [13]. Traditional medicine in Saudi Arabia is based on herbal remedies and spiritual healing and is widely used across the country, both as a commodity and as part of homemade remedies.
In 1940 the use of allopathic medicine in large Saudi Arabian cities began. Since then, health authorities have invested heavily in developing sophisticated hospitals. Based on the Legal Status of Traditional and Complementary/Alternative Medicine worldwide review [1], the population of Saudi Arabia today enjoys excellent health facilities. Although there was some governmental resistance to the use of complementary/alternative medicine (CAM) up until the 1990s, the demand for access to traditional healthcare allowed for some professionals who had trained abroad to begin practice in Saudi Arabia. The most commonly requested therapies are acupuncture, homeopathy and nutritional products. In fact, in Saudi Arabia herbal remedy is freely available to all residents through herbal remedy shops or from retail outlets. The only outlet that is under the ministry of health (MOH) control is pharmacies. Though substantial proportions of herbal medicines are registered with the MOH, a large number of unregistered herbal products is also dispensed from a wide range of outlets, other than pharmacies.
Recently, assessed therapeutic use and prevalence of herbal remedies in the treatment of conditions affecting children in Taif city [14]. This study revealed that a reasonable proportion of the respondents used herbs to treat their children. Over half of the parents that responded (58.0%) had used herbs to treat their children in the four months prior to completing the questionnaire and 70.3% had used herbs to treat their children at some point in the past. In another study done by Jazieh et al. [15], which was conducted in the oncology department at King Abdulaziz Medical City for National Guards, Riyadh, it was found that 90.5% (n=453) of adults used some form of CAM as part of their cancer treatment. This study also found that 386 patients (85.2%) used dietary supplements, including: Zamzam water (59.8%), honey (54.3%), black seed (35.1%) and water over which the Quran had been recited (29.8%), as well as other remedies. Only 18% of the respondents discussed CAM use with their physician prior to use, compared to 68% who discussed it with religious clergy leaders (Sheikhs). Another notable practice in Saudi Arabia is the increased prevalence of self-medication, along with a concomitant use of herbal and conventional medicines [13]. This is an area of great concern due to its potential for drug–herb interactions [16].
Based on the relevant literature, it can be deduced that a significant number of consumers of HMs and HDS have a positive opinion with regards to self-medication and the use of herbal products [17]. However, in spite of this, interactions between HMs or HDS and conventional drugs can still occur. These interactions may result in an increase or decrease of the pharmacological activity of the herbs and/ or drugs and may consequently lead to toxic effects [3]. Indeed, a great number of interactions between conventional medicines and different HMs and HDS have been confirmed [17]. Furthermore, it is important to note that herbal products may also cause adverse drug reactions or have adverse effects themselves.
Despite the fact that, several studies were done to measure public interest toward the use of herbal products [18], the consumers’ awareness of herbal remedies, the safety of herbal dietary supplements, their attitude towards combining herbals and drugs have not been adequately addressed. To our knowledge nobody investigated the consumers’ awareness of herbal remedies, their attitude towards combining herbals and drugs, and the source of recommendations for their use in Saudi Arabia, therefore, the present study attempts to investigate the consumer awareness with regards to the safety of herbal products, the attitudes towards the combination of HMs and HDS with conventional drugs, and the motivation for the use of herbal products.
Materials and Methods
This study was conducted in seven private pharmacies located in different socioeconomic regions of Riyadh, within an area of 3580 km2 and population of 6,167,626. Based on the rule < of < thumb, sample size was determined with 420 subjects having 95% confidence intervals, and a margin of error of ± 5%. A validated structured questionnaire was used for the data collection from subject who voluntarily agreed to participate and who purchased HMs and/or HDS using a convenience sample method over a three month period from 25 August to 20 November 2013 from 10 am to 6 pm. The researchers used a prevalidated pre piloted questionnaire adopted from Samojlik et al. [3]. The questionnaire was translated into Arabic, modified to be applicable to Saudi Arabians and then translated back into English to ensure translation equivalency and appropriateness. The questionnaire was piloted on a convenience sample of the target sample (n=20) to obtain the Cronbach’s α coefficient, which is a measure of the reliability of survey questions. The data resulting from the pilot study were excluded from the final analysis. The Cronbach’s α coefficient was found to be 0.871, which is satisfactory considering that 0.70 is the lower limit cut-off value [19]. Following our pilot study, we made additional modifications to the questionnaire to clarify the language. The questionnaire was approved by the Department of Clinical Pharmacy, Faculty of Pharmacy, Princess Nora University.
The questionnaire consisted of four parts as follows: socialdemographic data (age, sex and the educational level of the participants); the attitudes of the participants towards the safety of HMs and HDS; the sources of recommendation for the use of the purchased HMs and HDS and consumer attitudes towards the need to consult a pharmacist or physician prior to HM use during treatment with conventional drugs; finally, consumers were asked to provide information on the HMs or HDS that they had purchased. In addition, participants were asked if they had ever experienced any side effects from the use of HMs or HDS. Microsoft Office Excel 2010 was used to statistically evaluate the data and it was then loaded into SPSS (version 15.0) for descriptive statistics; a chi-squared test was used to differentiate between groups of participants where the values were considered significant (p=0.05).
Results
Out of 420 questionnaires that were distributed, a total of 308 questionnaires were returned. However, fourteen respondents did not meet the inclusion criteria and were subsequently excluded, giving a net total of 294 participants. Although the response rate was 70%, the total number of collected questionnaires was above the target sample. The reasons for non-participation were, amongst other things, a lack of interest and a lack of time to complete the survey, as well as no stated reason. The demographic details of the participants and the survey settings are summarized in Table 1.
| A | Gender | Age (years) | Total | |||
|---|---|---|---|---|---|---|
| 18–25 | 26–40 | 41–60 | 61 and over | |||
| Male | 15 | 59 | 18 | 13 | 105 | |
| Female | 44 | 97 | 29 | 19 | 189 | |
| B | Education level | Age (years) | Total | |||
| 18–25 | 26–40 | 41–60 | 61 and over | |||
| School | 14 | 21 | 17 | 24 | 76 | |
| Bachelor’s degree | 31 | 97 | 19 | 8 | 155 | |
| Master’s degree | 14 | 38 | 11 | 0 | 63 | |
| Ph.D. | 0 | 0 | 0 | 0 | 0 | |
Table 1: Demographic data for the survey participants (n = 294), ranked according to (A) sex and age, and (B) education level and age.
In Table 1, part (A) it can be clearly seen that females were the major respondents (n=189, 64.3%) and 97 of these females were aged 26–40 years. The smallest group of consumers were those aged 61 and over (n=32, 11.0 %). In Table 1, part (B) the respondents are categorized according to their educational background. The majority of respondents (n=218, 74.1%) were educated to bachelor’s degree level or higher and 135 of these respondents (46.0%) were aged 26-40 years.
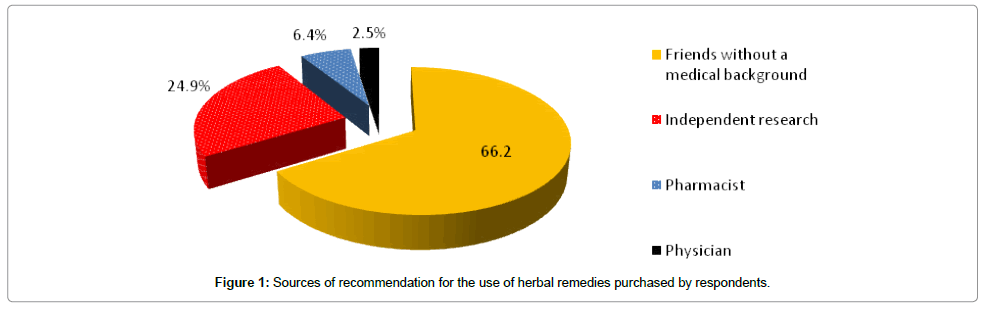
As can be seen in Figure 1, the majority of participants (n=267, 91.1%) did not consult or take advice from a pharmacist or physician prior to purchasing the HM or HDS with regards to their concurrent use with conventional therapy. Interestingly, consumer decisions on the use of HMs or HDS was based on the advice of friends, relatives, independent internet research, advertisements, etc. The collected data revealed that only nineteen (6.4%) consumers purchased HMs on the advice of a pharmacist and seven (2.5%) consumers HMs or HDS following a recommendation from their physician.
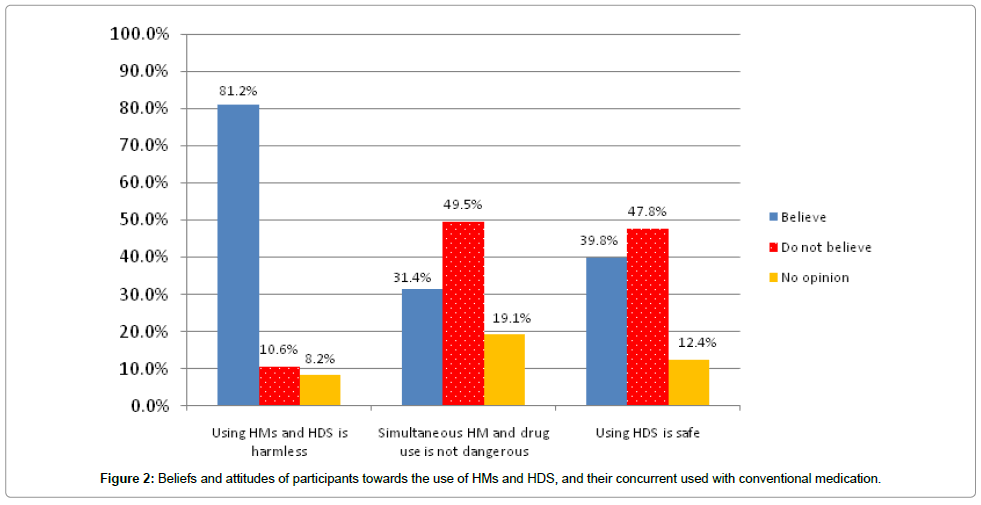
The predominant HMs or HDS purchased by participants in this study were based on cranberry (Vaccinium oxycoccos) or garlic (Allium sativum), and the frequency of use and the dosage varied with the age group (Table 2). Datura stramonium, Commiphora molmol, Boswellia carteri, Trigonella foenum-graecum, Camellia sinensis (green tea) and Nigella sativa were also popular choices. The majority of respondents (n=239, 81.2%) believed that HMs and HDS are harmless, while 31 participants (10.6%) believed that their use is dangerous. While 146 participants (49.5%) considered that the concurrent use of HMs or HDS and conventional medicine is not safe, 31.4% believed this treatment approach is harmless (n=92) and 19.1% had no opinion (n=56). In general, 47.8% of respondents believed that HMs are not completely safe (n=141), 39.8% (n=117) believed they are safe and 12.4% (n=36) had no opinion (Figure 2).
| Age group | Herbal medicine | Therapeutic activity/indication |
|---|---|---|
| 18–25 | Datura stramonium | Antispasmodic |
| Commiphora molmol | Amenorrhea, dysmenorrhea | |
| Boswellia carteri | Coughs, anti-diarrhea | |
| Trigonella foenum-graecum | Stimulate milk flow, anti-fatigue, menstrual cramps | |
| Camellia sinensis | Antvioxidant | |
| Ocimum basilicum | Antifungal | |
| Allium sativum | Hypolipemic, antiplatelet agent | |
| Vaccinium oxycoccos | Urinary antiseptic | |
| Foeniculum vulgare | Anti-inflammatory, antiseptic, antispasmodic | |
| Eugenia caryophyllata | Coughs and colds, headaches, menstrual cramps | |
| Cimicifuga racemosa | Hormonal support | |
| 26–40 | Boswellia carteri | Coughs, anti-diarrhea |
| Trigonella foenum-gaecum | Stimulate milk flow, anti-fatigue, menstrual cramps | |
| Nigella sativa | Headaches, general fatigue, indigestion, cardiac conditions, insomnia. | |
| Vaccinium oxycoccus | Urinary antiseptic | |
| Camellia sinensis | Antioxidant | |
| Zingiber officinale | Colds and coughs | |
| Ferula asafoetida | Digestive problems, whooping cough, respiratory conditions | |
| Datura stramonium | Asthma, coughs, bronchitis, early balding | |
| Cimicifuga racemosa | Hormonal support | |
| Allium sativum | Hypolipemic, antiplatelet agent | |
| 41–60 | Nigella sativa | Headaches, general fatigue, indigestion, cardiac conditions, insomnia. |
| Zingiber officinale | Colds and coughs | |
| Acacia | Anti-cancer, anti-tumor | |
| Vaccinium oxycoccos | Urinary antiseptic | |
| Allium sativum | Hypolipemic, antiplatelet agent | |
| Arnica montana | Natural pain relief | |
| Astragalus membranaceus | Anemia, diabetes, fatigue or lack of appetite after chemotherapy, kidney disease | |
| 61 and over | Commiphora molmol | Rheumatic, arthritis |
| Allium sativum | Hypolipemic, antiplatelet agent | |
| Acacia | Anti-cancer, anti-tumor | |
| Arnica montana | Natural pain relief | |
| Medicago sativa | High cholesterol, kidney and bladder problems, prostate problems, asthma, arthritis | |
| Astragalus membranaceus | Anemia, diabetes, fatigue or lack of appetite after chemotherapy, kidney disease |
Table 2: The most frequently purchased herbal medicines, ranked via age group (n = 294).
Out of all the participants, 212 (72.2%) avoided the simultaneous use of HMs and HDS with conventional drugs or over-the-counter products; however, 55 participants (18.7%) acknowledged that they have previously used herbal products concomitantly with one or more prescribed drugs and 27 participants (9.1%) had combined HMs with over-the-counter products.
Discussion
The use of herbal remedies is very common among our participants in Riyadh city the capital of Saudi Arabia. The study reveals that herbal medicinal herbal products are popular as a result of a widespread belief that the preparations are natural and therefore safe. This finding is also consistent with the previous survey report, which revealed that Saudi nationals consider herbal products are more effective and safer for use than conventional medicine in different aspects [13,16].
Additionally the current study revealed that middle-aged women that are more highly educated more frequently take HMs and HDS, which is concurrent with the findings of Picking et al. [20], and Kennedy [21]. This increased use emphasizes the need for the improved education of practitioners in alternative therapies [5,22]. This study found that only 8.9% of participants had consulted a pharmacist or physician prior to the simultaneous use of herbal products and conventional drugs; this may be due to the fear of practitioner disapproval [10]. Previously, consumer surveys have found that fear is an obstacle that discourages patients from discussing the use of herbal products with their pharmacist or physician [11,17]. That said, it is interesting to note that previous research has also found that patients are encouraged to used herbal remedies by many pharmacists and physicians [23]. One of the main roles of pharmacists is indeed to counsel the patients regarding their medications and it is all the more important for them to develop these skills to reinforce their existing role as the primary information provider to consumers [13]. There is also an urgent need for the concerned regulatory bodies to identify a reliable source of drug information pertaining to herbal medications. This may be achieved by establishing drug information centers. It is no doubt that these efforts will facilitate provision of an enhanced and a comprehensive pharmaceutical care in Saudi Arabia [13].
Our study found that the majority of respondents (91.1%) used HMs or HDS following their own independent research or following the recommendations of friends with no medical background. This is unusually high as previous research has indicated that approximately 52% or fewer respondents take herbal products without consulting a professional [3,5,22]. It is possible that the increased availability of such remedies and the sometimes aggressive advertising campaigns have contributed to an increased number of consumers using HMs and HDS without previous consultation with a physician or pharmacist [11]. Appropriate educational activities may improve knowledge and awareness regarding herbal remedies [24].
In agreement with the above, this study also revealed that 81.2% of participants considered the use of HMs and HDS harmless, which fits with the prevalent attitude that ‘natural’ remedies are both beneficial and ‘risk-free’. The word ‘natural’ is commonly associated with purity and safety and the absence of chemicals and/or preservatives. Similarly, Yilmaz et al. [17] found that approximately 33% of herbal product consumers believed that ‘herbals are healthy’ and that additional benefit is gained if they are combined with other medicines. This is consistent with an American study by Kennedy [21], which found consumers frequently combine herbs with conventional drugs. Over 50% of participants believed that herbal remedies combined with conventional treatment would have a beneficial or additive effect. Furthermore, in a study focused on consumers of herbal products in Jamaica, found that 13% believed herbs and drugs ‘work well together’. These findings may suggest that the majority of consumers use herbs as complementary therapies to conventional medication rather than a straight alternative [20].
The study showed that cranberry and garlic were found to be the most popular products regardless of the age group. Those aged 18-25 predominantly believed that cranberries and cranberry juice help to prevent urinary tract infections (UTIs) and this was the major reason for the consumption of herbal products containing cranberry in this age group, as well as the beneficial effects of the antioxidants that these berries contain. These finding are supported by Samojlik et al. [3], who found that cranberry, followed by garlic, are the most popular HMs used by those aged 18–25. Meanwhile, in our study it was found that those aged 26-40 predominantly used herbal products to improve metabolism and digestive function to facilitate weight loss.
Limitations of the Study
This study has a number of limitations that must be acknowledged. First, it may not be possible to extrapolate the results to the general population since the sample size was selected following a convenient sampling approach and the response rate was 70%. In addition, the study was conducted only in Riyadh and so does not necessarily reflect the attitudes of consumers in other Saudi Arabian cities. Second, bias cannot be completely excluded since the selected participants were those that used HMs or HDS. Consequently, the attitudes and opinions of those that do not use these products have been neglected. Future research should consider these issues and extend the survey to other cities and a wider variety of participants.
Conclusion
This study demonstrates the need for increased public awareness regarding the usage of HMs and HDS. While the use of HMs as a primary course of treatment is certainly feasible, and even recommended in some instances if the hazard–benefit rate is favorable to conventional medications, it should be respected that HMs are not free from adverse effects and may not be suitable for all patients. In particular, special care should be taken for the treatment of children, women during pregnancy, the elderly or patients with chronic conditions. Pharmacists and physicians are required to provide patients with comprehensive advice and information regarding the use of HMs or HDS, as well as the risks of combining them with conventional drugs. Of course, this makes it necessary for healthcare providers to be familiar with HMs and HDS and easy access to information, research and medical studies relating to the use of HMs should be provided. In addition, pharmacists and physicians should be encouraged to routinely ask patients about their use of HMs and HDS. In the UK, herbs used to be exempt from licensing but could be sold as food supplements, but new EU legislation in April 2011 means that herbal products must now be either licensed or registered.
The demand for herbal products is growing and it is recommended that herbal medicine be included in the education of pharmacy and medical students so that they become informed of the risks and benefits of HM use, correct dosage and administration protocols, and possible adverse effects, particularly in combination with conventional drugs. As for consumers, education about the use of HMs and HDS, especially in combination with conventional drugs, is essential to reduce the risk of adverse interactions. Diverse managed by the Ministry of Health or universities should be launched with the cooperation of local communities.
Acknowledgements
The author is grateful to the pharmacies owners. Our appreciations are extended to the pharmacists who helped in distributing and collecting the questionnaires. We also thank Dr. Abbas Albarq for his unconditional support, and the faculty of the pharmaceutics department in Princess Nora University for their constructive discussions and opinions.
References
- Legal Status of Traditional Medicine and Complementary/Alternative Medicine: a Worldwide Review (2001) World Health Organization, Geneva.
- Capasso F, Gaginella T, Grandolini G, Izo A (2003) Physiotherapy: A Quick Reference To Herbal Medicine, Berlin: Springer; ISBN 3: 52-56.
- Samojlik I, Mijatovic V, Gavaric N, Krstin S, Božin B (2013) Consumers' attitude towards the use and safety of herbal medicines and herbal dietary supplements in Serbia. Int J Clin Pharm 35: 835-840.
- Schulz V, Hänsel R, Tyler E (2001) Rational Phytotherapy. A Physician’s Guide to Herbal Medicine, 4th Ed., Berlin, Springer 1-9.
- Cavaliere C, Rea P, Lynch E, Blumenthal M (2009) Herbal supplement sales experience slight increase in 2008. Herbal Gram 82: 58-61.
- Thomas KJ, Nicholl JP, Coleman P (2001) Use and expenditure on complementary medicine in England: a population based survey. Complement Ther Med 9: 2-11.
- Marstedt G, Moebius S (2000) Inanspruchnahme altemativer Methooen in der Meclizin. Gesundheitserstartung des Bunds 9: 1-37.
- Mason P (2007) Dietary supplements 3rdedn
- Cooperman T, Obermeyer W, Webb D (2003) Consumer- Lab.com’s guide to buying vitamins and minerals: what’s really in the bottle?
- Bozin B, Mimica-Dukic N, Bogavac M, Suvajdzic L, Simin N, et al. (2008) Chemical composition, antioxidant and antibacterial properties of Achillea collina Becker ex Heimerl s.l. and A. pannonica Scheele essential oils. Molecules 13: 2058-2068.
- Williamson E, Driver S, Baxter K (2009) Stockley’s herbal medicines interactions. London: Pharmaceutical Press. 1-432.
- Zhang X (1998) Regulatory Situation of Herbal Medicines. A Worldwide Review.
- Al-Arifi MN (2013) Availability and needs of herbal medicinal information resources at community pharmacy, Riyadh region, Saudi Arabia. Saudi Pharm J 21: 351-360.
- El-Mawla A, Albarrag A, Abdallah M (2013) Herbal medicine use in a group Taif children, Saudi Arabia. Scope Med Journal 3: 41-44.
- Jazieh AR, Al Sudairy R, Abulkhair O, Alaskar A, Al Safi F, et al. (2012) Use of complementary and alternative medicine by patients with cancer in Saudi Arabia. J Altern Complement Med 18: 1045-1049.
- AlBraik FA, Rutter PM, Brown D (2008) A cross-sectional survey of herbal remedy taking by United Arab Emirate (UAE) citizens in Abu Dhabi. Pharmacoepidemiol Drug Saf 17: 725-732.
- Yilmaz MB, Yontar OC, Turgut OO, Yilmaz A, Yalta K, et al. (2007) Herbals in cardiovascular practice: are physicians neglecting anything? Int J Cardiol 122: 48-51.
- Natural Medicines Comprehensive Database
- Abbas N, Suleiman A, Almualla A (2013) Using structural equation modeling for beginner. Jordan, Amma Ithraa.
- Picking D, Younger N, Mitchell S, Delgoda R (2011) The prevalence of herbal medicine home use and concomitant use with pharmaceutical medicines in Jamaica. J Ethnopharmacol 137: 305-311.
- Kennedy J (2005) Herb and supplement use in the US adult population. Clin Ther 27: 1847-1858.
- Venn S, Meadows R, Arber S (2013) Gender differences in approaches to self-management of poor sleep in later life. Soc Sci Med 79: 117-123.
- Ambrose ET, Samuels S (2004) Perception and use of herbals among students and their practitioners in a university setting. J Am Acad Nurse Pract 16: 166-173.
- Shields KM, McQueen CE, Bryant PJ (2004) National survey of dietary supplement resources at drug information centers. J Am Pharm Assoc (2003) 44: 36-40.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 22655
- [From(publication date):
March-2014 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 17573
- PDF downloads : 5082