Research Article Open Access
Aspects of Common Traditional Medical Practices Applied for Under-Five Children in Ethiopia, Oromia Region, Eastern-Harargie District, Dadar Woreda, 2011 G.C
Elias Ahmed Sadik1*, Tesfaye Gobena1 and Bizatu Mengistu1
Department of graduate studies, Haramaya University, Ethiopia
- *Corresponding Author:
- Elias Ahmed Sadik
Haramaya University, Dire Dawa, Ethiopia
E-mail: mensurelias@gmail.com
Received date: June 19, 2013; Accepted date: July 29, 2013; Published date: August 02, 2013
Citation: Sadik EA, Gobena T, Mengistu B (2013) Aspects of Common Traditional Medical Practices Applied for Under-Five Children in Ethiopia, Oromia Region, Eastern-Harargie District, Dadar Woreda, 2011 G.C. J Community Med Health Educ 3:237. doi:10.4172/2161-0711.1000237
Copyright: © 2013 Sadik EA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Traditional medical practices (TMPs) are widely used in Ethiopia. Among these, some of them may be harmful and others can be useful. The type and degree of the practices with their risks and benefits vary from place to place in the country requiring the need for researches. Thus, this study was conducted to investigate aspects of common TMPs applied for under-five children. Objectives: To identify the major pushing and pulling factors for the use of common traditional health practices for under-five children in the area, during, 2011 G.C. To rule out the health hazards of invasive traditional health practices which were applied as alternative options for under-five children. To point out the contribution of the most common traditional health practices applied for under-five children to the achievement of MDG 4. A cross-sectional study was conducted in Dadar woreda from January to April 2011. Data as collected mainly by using qualitative technique from 24 FGDs participants and 12 in-depth interview respondents using guiding questions and interview questionnaires. Data were analyzed by using SPSS v16 software. According to the study result, Uvulectomy, tonsillectomy, cauterization, milk tooth extraction, spiritual healing and herbal medicine provision are commonly used as a therapeutic purpose. Culture, availability of practitioners, relief response, cost and distance were reported as the main reasons for use of TMPs. This study result has reminded us of the fact that practicing invasive traditional practices was abusing the health rights of children and hindering the country from achieving MDG 4. Generally, some TMPs were harmful while others were useful from health science perspective. For example, “Huddufor” TMP that was identified by this study, is more harmful because of three reasons: 1) Insertion of green stick into anus is more stressful, 2) It repeatedly ulcerates anal region and causes bleeding, 3) The site is prone to develop infection and prolapsed rectal sphincter. Though it has been practiced as a healing practice was found to be a killing practice for children. On the other hand, oral rehydration solution (honey, water, lemon and salt) used by herbalist to treat diarrhea and Spiritual healer’s advices on personal and environmental hygiene to prevent evil attack need to be strengthened, while non-invasive practices were somewhat contributing positively. Finally, continuous and sustainable health education, integration of HEWs, Traditional practitioners, and religious leaders; Banning and Broadcasting information about HTHPs, Strong political leadership, community mobilization and involvement as well as further cross sectional to determine perception of the communities toward use of HTHPs and analytical studies for safety and efficacy of important medicinal plants for conservation are recommended.
Introduction
Traditional medical practice (TMP) is defined as “the sum total of all the knowledge and practices, used in diagnosis, prevention and elimination of physical, mental or social imbalance and relying exclusively on practical experience and observation handed down from generation to generation” [1]. TMPs have been practiced on children as well as adults since time immemorial worldwide. The traditional health practice is mainly practiced by traditional practitioners at community level.
In Ethiopia, Traditional Medicine (TM) is a part of the national heritage. Policies and mandates have clearly been given to different government ministries and authorities to support the issue of traditional medicine with license. However, there are several gaps at the policy level and only a very limited number of efforts have been made in implementation. To develop proper guidelines for implementation, evidence-based data at community level are required [2].
There are a number of TMPs that reflect the diversity of Ethiopian cultures. Traditional medical practices related to surgery are bonesetting, uvulectomy, bleeding by puncture, cupping, cauterization, scarification and tooth extraction. Others are provision of mineral substances, medicinal plants and animal products. There may also be many unrecognized traditional medical practices in different communities which may influence the health of community in different ways. This indicates that region-specific studies are important [3].
Some studies have revealed that Ethiopians use TM due to the cultural acceptability of healers and lack of access to modern health facilities [4]. However, the current Ethiopian health care system is a primary health care system focused and access is available. Nevertheless, both rural and urban populations continue to use traditional medicine. The reasons behind this are not yet clear.
Although TM plays an important role in Ethiopian society, knowledge about the extent and characteristics of traditional medical practices is limited. The national health system has ignored studying therapeutic potentials as well as adverse effect. All types and their determinants have also not been thoroughly studied scientifically at the community level. One of the mandates of Ethiopian Health and Nutrition Research Institute is also conducting research on traditional medicine [5,6].
From all insights described above, the reader can understand that issues of TMPs have public health importance. For instance, certain practices have not been given critical attention. One of these is the “Huddufor” traditional practice which results in rectal ulceration and bleeding in children. It has been practiced in Harargie Zones of Oromia region over a century though it has never been studied before [7].
Although many TMPs have been analyzed for their risks and benefits, certain traditional practices have not yet been recognized in different localities. On the other hand, despite modern health service expansion and awareness creation efforts made to avoid HTP, certain malpractices have still being performed on children for a curative purpose in the area. Hence, the investigation of different TMPs used for children under five years of age in different localities was found to be very important. Both traditional medicinal practices and child health were priority issues of the country.
Therefore, this study focused on the most common local TMPs used for children under five years of age in Dadar woreda and involved child care providers from households, community leaders and traditional practitioners as well as health professionals in the locality. Thus, this study considered answering unclear questions related to TMPs:
1. How the existing most common TMPs are influencing the health of under-five children and MDG 4 achievement of in the country?
2. Why TMPs are being practiced on under-five children?
General Objective
To investigate aspects of the existing most common TMPs applied for under-five children and related factors in Eastern Harargie District, Dadar woreda.
Specific Objectives
a. To identify the major pushing and pulling factors for the use of common traditional health practices for under-five children in the area, during, 2011 G.C.
b. To rule out the health hazards of invasive TMPs which were applied as alternative options for under-five children during, 2011 G.C.
c. To point out the contribution of the most common TMPs applied for under-five children to the achievement of MDG 4 during, 2011 G.C.
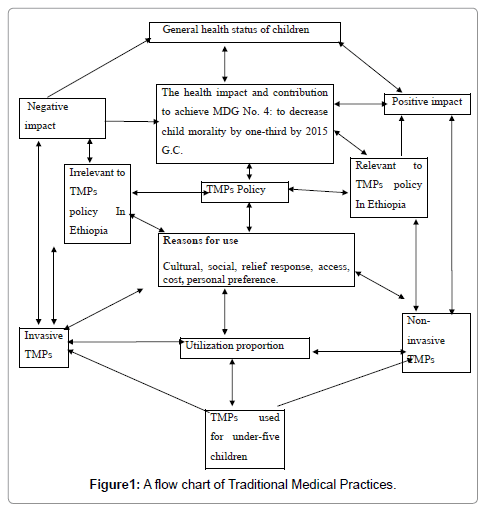
Based on the existing evidences of TMPs and observations from practical experiences the following Conceptual Framework was constructed (Figure 1).
Review of Literature
Overview of TMPs
TMPs have been practiced on children as well as adults since immemorial time worldwide. The TM has mainly been practiced by traditional practitioners at community level [8]. Europeans and North Americans have become open to accepting traditional medicine of Asia starting in the late 20th century. The new art and science of “Integrative Medicine” has emerged. Traditional healing and indigenous medicine have been brought into this philosophy and practice to integrate with modern health services so as to adopt to western countries [9].
Many traditional practices have been studied and described as either harmful or useful. For example Pygeum (Prunus africana) is used in traditional African medicine. The bark is made into tea in traditional African practice. Whereas elsewhere in the world it is sold in the form powders, tinctures, and pills. This drug was developed to modern medicine and used to increase and ease urination, to treat diarrhea and reduce inflammation as well as cholesterol deposits [10]. In such a way, some of the traditional medicines could be resources for a country if properly investigated and utilized.
There was evidence that certain plants had high medicinal value. For example there were aloe plant species in the world. Majority of them were used as sources of medicine in different countries of the world. Many of these Aloe species were grown and used for production of medicine in South Africa. Similarly, Henna plant was mentioned as a holly plant that has been used in the treatment of different human ailments [11].
In Ethiopia, a brief explanation about the nature of traditional medicine has also been given in the book of “Ethiopian herbal medicine” which was published currently in the year 2010. It described that many traditional medicinal plants found in Ethiopia were found to be useful and need to be conserved as a natural resources of the country [11].
In contrast, certain TMPs related to surgery were described as Harmful Traditional Health Practices. Some of these were: uvulectomy, bleeding by puncture, cupping, cauterization, scarification and milk tooth extraction. Others are provision of mineral substances and medicinal plants and animal products that were not supported for safety and efficacy. There might also be many unrecognized TMPs that could influence the health of community in different ways [12]. Similarly, a study conducted in western Ethiopia revealed that Harmful Traditional Health Practices like butter feeding and an uvulectomy practice were affecting the health of children under the age of five years.
According to the study conducted in Ethiopia in 2006, the risks of certain TMPs like an uvulectomy practice, tonsillectomy for their contribution to the transmission of HIV/AIDS (World Bank, 2006). Similarly, according to a study conducted in Lusaka by national research team, saliva or seminal fluid that was used as a treatment in the health care for children was found to be risky. The survey indicated that the use of such traditional medicine has risks of infectious disease transmission [13].
Thus, the issue of traditional practice had become important. The FMOH policy objective was to identify risks and benefits so as to halt those that could enhance transmission of HIV/AIDS as well as other health hazards and to promote those that could have health benefits for the community [2]. The existing situation of TM may differ from place to place as per cultural diversity in Ethiopia. Thus, the government of Ethiopia emphasized the importance of conducting area specific research on the aspects of TMPs and willingness to support [14].
What is the extent of traditional medical practices utilization?
The prevalence of use Traditional Medicine in certain developed countries like Canada 70%, Belgium 31%, USA 42%, Australia 48% and Franc 49% was demonstrated [15,16]. Similarly, the prevalence of TMPs use in certain developing countries like Rwanda 70%, Benin 70%, India 70%, Tanzania 60%, Uganda 60% and Ethiopia 90% was also shown [17].
According to survey conducted in Africa, up to 80% of the population uses traditional medicine for primary health care. Hence, for such a wide use, traditional medical practices should be considered as an important issue [18].
According to a population-based survey conducted in Wolayta, 90% of population uses TM in Ethiopia. As a result, issue of TM was seriously taken into account [19].
According to the study conducted on the use of anti-malaria plant known as Arthimesia Annua, in Arbaminch district the prevalence of plant users was found to be 95.5% among malaria cases [20].
Population based study conducted in all regions of Ethiopia, indicated occurrences of some harmful traditional health practices in Ethiopia as follows: uvulectomy 82.5%, tonsillectomy 54.6%, milk tooth extraction 86.6%, eyelid incision, 33%, arms vein puncture, 54.2%, scalp vein puncture 54.2%, and cauterization 51.5%. The highest proportion was reported from the Oromia region [21].
According to a study conducted in northern Ethiopia during 2005, the prevalence rates of uvulectomy and milk teeth extraction were 89% and 58% respectively. The study also indicated as the level education of mother increased the use of HTHPs decreased [22].
Why a wide use of traditional medical practices throughout the world?
Some of the reasons for wide use of Traditional Medicine worldwide were: Acceptability, Availability and Affordability. Need for alternative option, frequent resistance of certain chronic diseases against modern medicine. The local people have been seeking for their treatment even in preference to modern medications and also in connection with the community’s belief that they would not get better medications for some of the diseases in modern health services.
For most African people, all sickness is connected with the spirit. It could be a mental problem or physical problem. It is also believed that much illness in societies is caused by fear. So people look first for spiritual healing in their own culture. That is why traditional medical practice is considered as an option of primary health care in different countries [23].
Similarly, in many Ethiopians’ perceptions, Health is seen as a ‘gift of God’ or ‘the will of God’. They believe that their religion helps them to keep healthy. According to their perceptions, the devils considered to be the cause of a number of diseases, while God is believed to provide the healing. These perceptions are related to the belief that supernatural forces are involved in causation of disease and treatment. That is why they use spiritual healing practice in their localities [24].
For centuries Ethiopian people have been heavily relied upon TM for their primary health care. Because of their cultural experience they continued using TM in different part of the country [12].
Curing with any medical system may work because of three different factors. First, a cure may be successful. The second reason is that a cure may reduce unpleasant symptoms such as headaches and coughs. The third reason is that a cure may work because it is a placebo. For example, a doctor could give a harmless sugar pill and tell the patient that it is a powerful medicine. This placebo may actually make him feel better and even help him recover from a disease [25].
In Ethiopian traditional medicine, Religious practices play a large part in the healing process. Holy water (called ‘tsebel’ in Amharic) and praying for Orthodox Christians or ‘zemzem’ and praying in the case of Moslems were frequently used for a wide variety of illnesses. Ethiopians believe that holy water cures when it is drunk or bathed in [26].
The Ethiopian people’s reliance on TM was also reflected by the fact that Ethiopians living in developed countries continued using them. This showed that Faith was often embedded in the wider belief system and became an integral and important part of many people’s lives. For example, a number of herbs, traditional medical devices used by Ethiopians were found in the United Kingdom [27].
Some studies have revealed that Ethiopians use traditional medicine due to lack of access to modern health facilities. However, the current Ethiopian health care system is a primary health care system focused and access is available more than ever. But, both rural and urban populations continue to use traditional medicine. The reasons behind this were found to be the cultural acceptability of TMPs.
In Ethiopia, the reasons for use of TM were due to cultural acceptability, low cost and availability of traditional practitioners in the nearby [28]. In case of affordability; TM was not only relatively cheaper than modern medicine, but also payable in kind according to the wealth of the client [12,29].
Uvulectomy is commonly practiced on children. This is because of traditional beliefs that an elongated uvula is the cause of every problem in the throat. It is practiced by traditional healers using a pair of nonsterile scissors or sickle knife [30].
Different cultural and religious elements connected with the use of TM in Ethiopia were also described as some of the reasons for use of Traditional Medicine. For instance, there were three traditional cultural influences operating in Ethiopia. The traditional Oromo thinking, Kallu, the orthodox Coptic Church and Islamic teaching which look after disorders that was supposed to be caused by evil spirits using reputation and herbal remedies [31,32,34].
The result of the study conducted in north-west Ethiopia indicated that because of disease burden like abdominal cramp with strong crying in children people first contact traditional healers for their first line care. The major child health problem among under-five was intestinal parasites infection mainly Hook worm, S. stercoralis, T. tricuria, E. vermicularis, H. nana and S. mansoni. Severity of disease manifestation these double or triple infection was one of the reasons to use the nearby health practices. Some of these parasites could cause anal itching due to auto-infection or movement of certain parasite around the sphincter [35].
On the other hand, a study conducted in Arbaminch on antimalarial medicinal plants showed that the relief response from signs and symptoms of disease the major reasons that created high level utilization of TM in the area [20].
Another study also revealed that some of the plants in Ethiopia were found to be the best for the treatment of dermatological disorders. The health outcome as a result of certain medicinal plants was also the reason for the preference of TMP [33].
Certain other reasons have been listed for the practicing and preference of traditional practices in Ethiopia. Among these are lack of other options, distance from health service sectors, high cost of pharmaceutical drugs, and lack of knowledge and the perceptions of the community in accepting traditional practices as the best option [34].
Similarly, for evidence of inaccessibility of health services in the country, another study which was conducted on assessment of physician to population ratio in three regions (Amhara, Oromia and SNNPR regional states) in 2008 indicated the insufficiency of modern health professionals in Ethiopia. According to this study, the physician to population ratio in Amhara, Oromia and SNNPR regional states were computed to be 1:280,000, 1:220,000, and 1:230,000, respectively. While the physician to population ratio WHO standard for developing countries is 1:10,000. This is a huge gap that could be one of the reasons for use of TMPs in the country [35]. According to WHO 2005 report, the ratio of TM practitioners to population was 1:200 while that of modern medicine practitioner was 1:20,000. This showed that Traditional Medicine practitioners were more widely available than modern medicine practitioners (WHO, 2005).
Traditional health practitioners were most often the first line of care providers. They were involved in community based care, health education, counseling and relief of certain symptomatic conditions. They have got acceptance and received respect in the community [36].
Because of cultural and long term experience, Traditional practitioners were supposed to be gateways to community health activities (to provide and/or receive culture-specific information and channeling specific health promotional messages to the community at large). Traditional healers are resources to the enhancement health care in Ethiopia and could not be underestimated.
Traditional Medicine Policy
Issue of TMs promotion was started after 1978 primary health care delivery strategy adoption in Ethiopia. Thus, Ethiopia gave emphasis to the role of TM and incorporated the system in the Health and Drug policy with Code of Ethics of TM. The policy of 1993 emphasized the need to develop beneficial aspects of TMs and evaluation. One of the Mandates of EHNRIs was to conduct research on traditional medicine to document important information at community level.
WHO also has been collaborating with Ethiopia in the area of TM since the late 70s. It has also been supporting the research work in TM by providing funds for procurement for laboratory equipment and supplies. By covering costs of training and studies, it continued to support TM development in Ethiopia. The strategy provided a firm work for action for WHO and its partners. The specific objectives of the strategy were to support member countries to:
1. Integrate TM with National health care systems as appropriate by developing and implementing national TM Policy and programs.
2. To promote the safety, efficacy and quality of TM by expanding the knowledge base on TM, and by providing guidance on regulatory and quality assurance standards.
3. To increase availability and affordability of TM for the poor populations.
4. To promote appropriate therapeutic use of TMs by providers and users. The strategy was for adoption and implementation at regional and country level [15,16].
The fifth African Traditional Medicine Day, under the theme of ”Research and Development of Traditional medicine” in WHO of African region, Aug. 31, 2007; supported the TM policy of Ethiopia [37,38]. On August 31, 2009, African traditional medicine Day was celebrated under the Theme “Traditional medicine and patient safety”. During the celebration member states urged to conduct advocacy and educational programs. The MOH of Ethiopia recognized the important role of traditional health systems was stated in its Health and Drug [39].
Health is a fundamental human right. Access to health care which includes access to essential drugs is a prerequisite for releasing the rights. WHO has estimated that half of the population in Africa lack access to essential drugs in the poorer area. Thus, TM has been used to fill this gap particularly in the developing country [14,15]. World Health Organization further planned to develop TM in order to address issue of policy, safety, efficacy, quality access and rational use of TM in the country. World Health Organization country office also clearly described that evidences that support claims of TM in the country were limited [38].
According to the United Nations MDG report, improvement of child health had to be seen seriously from different aspects in developing countries. The intention was to reduce the under-five mortality rate by two thirds by the year 2015. Cultural values and beliefs need to be respected and understood, to appropriately use them within any caring or curing processes [39]. Cultural conditions need to be considered to provide culturally congruent, meaningful, and beneficial health care to the people. Thus, the negative and positive elements of TMPs were some of the cultural issues that determine the health of under-five children [37].
From a human right perspective, HTHP is discouraged, particularly when performed on infants and children. Children are dependent on adults. Children cannot make decisions regarding their health. Children are not able to fight against the violation of their health rights. They are not able to decide on what is good and conducive to their health. Because of this reason the international human rights constitution states that performing any malpractice on children is a violation of human rights. Parents’ right should not override the health rights of children [40].
The National Health right law has also stated that no person’s life should be put at risk or endangered by reason of a lack of access to health care services and/or information, counseling or services related to sexual or reproductive health. Thus, all persons have the right to be free from any medical intervention that may negatively affect their health [41].
According to Ethiopian Traditional Medicine policy: Code of Ethics in relation with job competence: part 2, Article 2, herbs given by the practitioners should be recognized and tested for their safeties for getting license. Practitioners would only be allowed after having been formally registered to do so. The policy also prohibited practicing any invasive practice that could affect a person physically, mentally, emotionally and psychologically under Code of Ethics in relation with job competence: part 3, Article 3.4. The policy also strongly stated in Code of ethics article 3.1: giving due attention to the development of beneficial aspect of TM as one of the health priorities [42].
Woreda based health sector planning also focused on innovative research activities to meet diverse needs of child and adolescent people, in the context of Ethiopian priorities and culture. The objective is to increase the understanding of the socio-cultural factors associated with health and health related issues at community level. TMP is one of these components [43].
Generally, Cultural diversity among population of Ethiopia was one of the indications for the importance of area specific TMP studies. Thus, according to the Proclamation of 1999, Article: 2 sub-Article: 6, the health policy strongly support the research on TM [44].
Perspectives of traditional medicine
TM could play an important role in the growing economic importance in many countries of the world as a domestic resource of the countries. Furthermore, Traditional Medicine was found to be the property of the community and nations that should be fully respected and properly practiced. For example, tropical plants like Chamomela (khammona), the black seed or Habbatu-sowda (nigelia sativa), henna, aloe juice or powder, olive oil, onion, garlic (Allium sativum), lemon, papaya, cucumber and edible mushroom were mentioned for their medicinal value [45].
According to a study conducted in Ethiopia, cessation of the natural resources (medicinal plants) from the surface of the earth due to certain reasons was described. The reasons were: deforestation, migration, urbanization and lack of conservation of natural resources. As a result, the study also recommended the importance of conservation of medicinal plants in the country [26].
Certain study result also described that there are good TMPs as well as bad TMPs which are not safe and efficacious from health professionals’ perspective. A study result conducted in Ethiopia in 2007 and 2010 explained that without investigation of beneficial aspects of TM and non-beneficial ones, there would not be an effective promotion of TM in the country [46,47]. In contrast, certain TMPs incorporate some harmful practices and beliefs. For example many Traditional practitioners have been practicing HTHPs to make many out of it even after informed. This shows that personal benefits have been over-riding the health rights of children in different areas of the country [48].
For this matter, WHO in Ethiopia signifies the need for undertaking scientific research to generate evidence for the safety, efficacy and quality of traditional medicinal products and practices in the country [36,41].
Furthermore, despite the advancement of health service technology and Information Education Communication (IEC) Programs, certain malpractices have been performed on children as therapeutic means in different localities. The basic reasons for performing HTP on this defenseless segment of the community were not clear. Thus, the reasons for the practices need to be addressed by studies.
All the above information showed that the issues of TM had public health importance their effects and counter effects. Based on the above given insights, the study focused mainly on identifying the prevalence and reasons for use of TMPs in Soka locality of Dadar woreda.
Materials and Methods
Study area and period
Study was conducted in Dadar woreda of Eastern Harargie District. The woreda was randomly selected.
Study design
A cross sectional study was used with qualitative data collection methods.
Populations
Source population: included community leaders, health service providers, and traditional practitioners in the area.
Sampling
A total of 36 members participated. A total 24 Community leaders and elders participated in FGDs different 6 traditional practitioners and 6 health workers participated in in-depth interviews from each woreda.
Sampling technique
Purposive sampling method was used to get the right persons for answering the questions for the study at the beginning. Then, snow ball sampling method was used in the process.
Data collection
Data were collected by FGDs, a group discussion and in-depth interviews.
Data collection instruments
FGD guides, tape recorder, note books, observation checklists and mobile were used.
Data collectors
There were six data collectors that were involved Health officer, Nurses and Environmental health professional and health extension workers (who were not working in the study area).
Study variable
The use of common types of TMPs.
Quality Control
Detail orientation was given to the participants about the study before data collection procedure was stared. Translations of data collection instruments into local language were done. Supervisions of data collection activities were properly done throughout data collection periods.
Data processing and analysis
Data cleaning, data transferring, transcribing and translating were carried out immediately after daily data collection activities accomplishment. Finally data were analyzed by manual and SPSS software analysis.
Ethical Consideration
The study was approved by the Haramaya University College of Health Sciences Institutional Research Ethics review committee. The letters of cooperation were written from SGS office to the concerned officials of E/Harargie zone, Dadar woreda and Soka locality about the research project. Additionally, letters were written from local administrative office of kebeles and given to the data collectors and researcher. Each participant of the study was informed about confidentiality. Each participant of the study agreed to participate voluntarily. All participants of the study declared their willingness to participate and approved by signing consents. Generally, the study participants were voluntarily participated in the study.
Results
According to this study result, the existing TMPs were Uvulectomy (waan laagaa), Huddufor traditional practices, milk tooth extraction (Daawo), Spiritual healing, use of herbal medicine, incision on the butock, giving butter to the newborn, cupping and cauterization (Gube). Among these, the most common TMPs were Uvulectomy (waan laagaa), Huddufor traditional practices, milk tooth extraction (Daawo), Spiritual healing, and use of herbal medicine.
For the reasons, one of the participants said: “It is culture, income, cost, relief from disease condition of intestinal parasites and protection from hemorrhoid (Buroo)”.
All the participants in FGDs mentioned the goodness of Spiritual healing and plant as well as animal product medicine and also commented importance of further studies need to improve the use of such TMPs. One of respondent said: “Huddufor” practice can treat all gastro-intestinal problems of under-five children which are manifested by itching around anus and eye infection”.
Concerning health risk, two of the participants said: “invasive practices can transmit HIV because of using unclean materials and techniques”. Others said: “either boiled or new materials are used and their contribution to HIV transmission is unlikely”. From the female side one of the respondents said: “I came across with blind practitioners that inserted the stick into the vaginal opening of the female child and severely injured her”. Another one said: “that was due to blindness”.
During in-depth interview, Uvulectomy practitioners explained that they had learnt it from their fathers. One of the practitioners was “Sheka” (a religious leader). His benefit was twenty-five birr per individual. He said that the benefit to the patient was relief from vomiting specially for newborns and treats disease of the throat for others. According to these practitioners, there was no risk to the babies except some “Injuries to other parts of the mouth of children that could sometimes occur due to poor handling of the mother”. Concerning the reasons of the practice, they said: “It is source of income for us curing of disease for children”.
Fortunately, the procedure was observed as a uvula was grasped by a string passing through a loop and snared into the loop. Then, by using a metal with curved blade at its tip; it was cut and put on the head of the newborn.
According to the practitioner that belonged to milk tooth extraction, benefit to the practitioner was Ten birr per individual and risk to the children was lack of eruption of permanent teeth during their latter life rarely. He said: “chronic diarrhea that could occur due to the worm grown at the base of milk teeth is cured by this practice”. It was also observed that the soft root of the tooth was shown to the mother as a diarrhea causing worm by the practitioner for advertisement of this practice. It was said that the practice was performed by inserting the tip of small knife into the gum and the tooth was extracted.
According to the practitioners that belonged to “Huddufor” traditional practice, the Benefits to the practitioners were 3-5 birr. Benefit to the patient was relief from anal itching. Risk to the practitioners was contamination with blood and stool. But they said that there was no risk to the children. He said that disease problems believed to be treated by the practice were general abdominal pain, poor appetite and anal itching including eye infection. In addition it was also believed to prevent hemorrhoid (Buroo). According to the responses of the practitioners, reasons for the practice were to serve the users and to get money.
“Huddufor” traditional practice was defined by all participants as: “an insertion of the green stick prepared from a local plant known as “Dergu” into the anus of under-five children and stirring either clockwise or anti- clock-wise direction several times that induce passing of stool followed by rectal bleeding. This practice has been performed on most children starting from the third month of age regularly for the minimum of 6-10 times before completion of five years both as a therapeutic and prophylactic purpose. The frequency of the procedure has been determined by the practitioner that is it could be monthly, quarterly or semi-annually.
Finally as a sign of completion of “Huddufor” traditional practice preventive procedures by doing 4-6 incisions on the buttock of children at the end of the five years of their ages. By chance, “Huddufor” practice was practically observed as it was causing severe bleeding, serious injury, prolapsed rectal sphincter and stress with strong crying, restlessness and profuse sweating of children. Among the above mentioned TMPs, this might be new for the readers of this paper who have not exposure to Eastern Ethiopia, regardless of ethnicity, regions and religions.
Additionally, the video show that was recorded by one of the data collectors during the procedure using his mobile was attached for evidence to visualize the health hazards of the practice on the children. One can imagine and answer the question: “Is it a killing practice or a healing practice for under-five children?”
According to Spiritual healing practitioners’ response, Spiritual healing has been applied by religious leaders to prevent or to treat the problem believed to be caused by evil spirit by reciting certain verses from the wholly book. Disease problems were manifested by sudden wakening up of children from sleeping, strong crying and refusal of breast feeding as well as running away from mothers. He also said that mothers were advised for proper personal and environmental hygiene to prevent an attack of evil spirit.
According to Herbal medicine provider’s response, his knowledge was basically Religious institution. He had a book that is used as a guideline. Disease problems treated were diarrhea skin rashes, wounds, throat infection, abdominal worms, eye infection, earache and malnutrition. Medicinal plants used: Eucalyptus leaves, Chamomela, the black seed or Habbatu-sowda (nigelia sativa), henna, aloe juice or powder, olive oil, onion, garlic (Allium sativum), lemon, papaya, cucumber and edible mushroom. Among animal products that were frequently used along with plant products: honey, egg, milk and liver were mentioned. The routes of administration used were: oral, nasal (inhalation and sniffing) and external application. Finally he suggested disappearance of certain medicinal plants from time to time in the country as a limitation and recommended importance of conservation of medicinal plants were recommended.
According to health professionals response, Culture, social influence like peer push, cost and lack of awareness about were explained as the reasons for use. They said: “Uvulectomy (waan laagaa), Huddufor traditional practices, milk tooth extraction are negatively affecting the health of children obviously”.
The woreda Health Officer (Ato Abdi Monammed Yuya) mentioned that “Huddufor” traditional practice has been practiced in Eastern and Western Harargie Districts of Oromia region over a century. Simlarly, Aliyie Yuya (Vice Head of Eastern-Harargie Health Office) described as this “Huddufor” traditional practice is commonly practiced, not only in Harargie Districts, but also in the regions of Somali, Harari, and Dire Dawa and not give attention.
A health worker who was working on private sector said “We are advising people not to do “Huddufor” traditional practice and giving them paracetamol suppository as an alternative solution to sooth the dry itching anal area of the anus”.
Discussion
Among the five most commonly used TMPs three of them were invasive practices while the other two were non-invasive ones. There has not been any information about “Huddufor” traditional practice documented before because “Huddufor” was not generally studied before.
This study result came up with the most neglected and locally deep rooted harmful traditional medical practice known as “Huddufor” practice. Thus, identifying something which affects health of children basically important for the Health Planning of the country. The parents’ need and practitioners benefit are over-riding the health rights of children.
Additionally, this study pointed out what had been affecting the child health that was relevant with the national policy that stated the importance of conducting area specific research on the aspects of TM [39,49].
Medicinal substances mentioned by Herbal and other natural product provider like edible mush-room for eye disease, aloe plant for throat infection, henna leaves for skin diseases, exactly in agreement other sources of knowledge [10,50,12].
Limitation of the Study
Lack of previous study documents on certain traditional practices especially “huddufor” and lack of documents related to the topic.
The Challenge
The challenge faced was refusal of certain key informants to respond, even after signing consent.
Summary
Uvulectomy, tonsillectomy, cauterization, milk tooth extraction, spiritual healing and herbal medicine provision were commonly used as a therapeutic purpose. TMPs going on in the area were of two categories. Some TMPs were harmful while others were useful from health science perspective.
“Huddufor” TMP which was identified by this study, is more harmful because of three reasons: 1) Insertion of green stick into anus is more stressful, 2) It repeatedly ulcerates anal region and causes bleeding, and 3) The site is prone to develop infection and prolapsed rectal sphincter.
HTHPs which have been practiced as healing practices were found to be killing practices for children. Children are dependent on their parents. They cannot fight for their health rights. Performing any stressful and invasive health practice on children is violation of child health rights. The harmful ones had serious health hazards for children and could facilitate the transmission of HIV/AIDS. Giving acetaminophen suppository for anal itching is as an alternative solution is another concomitant abuse of children.
On the other hand, oral rehydration solution (honey, water, lemon and salt) used by herbalist to treat diarrhea and Spiritual healer’s advices on personal and environmental hygiene to prevent evil attack need to be strengthened.
Culture, availability of practitioners, relief response, cost peer pressure, family advice, lack of alternative options, lack of knowledge and distance were reported as the main reasons for use of TMPs.
Conclusion
This study has reminded us of the fact that there are still many people who lack the appropriate knowledge regarding the ways of transmission of HIV/AIDS and in particular, given the present situation in which HIV/AIDS is a serious health problem of the country, the issue of HTHPs has to be addressed properly. All HTHPs were killing practices for children due to their serious health hazards.
Certainly, these HTHPs are strongly hindering back our country from achieving MDG 4 by 2015 G.C. The complications of invasive TMPs coupled with use of unsterilized tools for the children who cannot decide for their health are really dangerous and need urgent public health attention. Lack of knowledge and misunderstanding were implications for the burden of HTHPs.
Deworming would be the best solution for the treatment of intestinal parasites. The cause of anal itching which was one of the pushing factors to use this practice is as a result of the most endemic intestinal parasites that is one of top five diseases of under-five children in the area. The relief from anal itching is due to damage of nerve endings in the skin and mucous membrane.
On the other hand, certain practices were found to have beneficial aspects. The use of alloy plant fluid which was advised to be sniffed through nostrils as an alternative solution for avoidance of uvulectomy in the book of medicine of the Prophet (PBOABUH) was the best religious teaching that must be adopted.
Recommendation
Calling for the urgent public health communities’ attention at local, regional, national and Global levels for the avoidance of HTHPs for the better health of under-five children. Banning and broadcasting information about HTHPs through different local media centers in local language are recommended. Training of HEWs, Traditional practitioners, as well as religious leaders and involvement in the struggle against HTHPs and health education activities in the local community. Strong political leadership by the local government and community mobilization are needed to be strengthened for the proper implementation of TM policies of the state. Further studies of medicinal plants their conservation is recommended.
Similarly, a mixture of honey, common salt, water and lemon used for diarrhea and vomiting is directly concordant with components of composition ORS which is globally used in modern medicine for the same purpose. Such useful TMPs need to be strengthened. Gradual cessation of certain medicinal plants and importance of conservation was strongly supported by other study results [4,47].
The teaching of hygienic by spiritual healer was something that was strongly in agreement with modern health teachings. The study has realized the existence of use of already recognized HTHPs and another newly recognized one.
References
- WHO (2001) Legal Status of Traditional Medicine and Complementary/Alternative Medicine: A Worldwide Review. Geneva.
- Federal Democratic Republic of Ethiopia (2003) Health and Health Related Indicators.
- Yimer S, Bjune G, Alene G (2005) Diagnostic and treatment delay among pulmonary tuberculosis patients in Ethiopia: a cross sectional study. BMC Infect Dis 5: 112.
- Bahiru TW (2006) Impacts of Urbanization on the Traditional Medicine of Ethiopia. 8: 45-50
- FMOH (2006) Ethiopian Federal Ministry of Health. Ethiopian traditional medicine.
- EHNRI (2006) www.ehnri.org. Accessed on Aug 2010.
- Adem Y, Muchae A (2008) Prevalence of intestinal parasies in Metema District Hospital. North-West Ethiopia. Ethio J Health Biomed Sci 2: 121.
- Griffiths M (2010) Traditional and Alternative Health Care Practices: Oxford J. University Press, London.
- World Bank (2008) Organizing African Traditional Medicine.
- Encarta (2009) Encarta year book of 2009. Traditionally used medicinal plants.
- Fulas F (2010) Ethiopian herbal medicine.
- Addis G, Abebe D, Urga K (2001) A survey of traditional medicinal plants in shirka, Arsi Zone, Ethiopia. Ethiop Pharm J 19: 30-47.
- Wojcicki JM, Kankasa C, Mitchell C, Wood C (2007) Traditional practices and exposure to bodily fluids in Lusaka, Zambia. Trop Med Int Health 12: 150-155.
- Urga K, Asefa A, Gudina M (2003) TM in Ethiopia. Proceeding of a national workshop held in Addis Ababa. During June 30- July 2, 2003. EHNRI, Addis Ababa, Ethiopia.
- WHO (2002) Regional strategy for traditional medicine in the Western Pacific Region. WHO, Geneva.
- WHO (2002) World Health Organization. Press Conference on WHO’s TM strategy. Geneva.
- EHNRI (Ethiopian Health Nutrition Research Institute) (2004) Traditional medicine in Ethiopia: Proceeding of a national workshop held in Addis Ababa, Ethiopia. June 30-July 2, 2003.
- Leonard KL (2008) African Traditional Healers. The economics of healing. World Bank, Washington, DC.
- Dikasso D, Urga K, Addis G, Tadele A (2002) The attitude of modern health workers towards traditional health care system in Wolayita Zone. J Ethiop Med Pract 4: 92-95.
- Tiruneh G, Kebede Y, Yigzaw T (2006) Use of the plants Artemisia as a natural anti malarial herb in Arbaminch. Ethiopian Journal of Health and Biomedical Sciences: University of Gondar, Ethiopia 2: 75-76.
- Jeppson A, Tesfu M (2003) Traditional Surgical practices in Ethiopia. Ethio J Healt Dev 17: 30-40.
- Alene DG (2005) Prevalence of HTHPs among under-five children. Dembia district northwest Ethiopia. EthioJ. Health Biomed Sci 2: 85-86.
- Mbiti J (2010) General manifestations of African-Religiosity.
- Addis Tribune (2005) Some Aspects of Traditional Medicine in Ethiopian.
- Shekhar S, Thornicroft G, Knapp M, Whitefield H (2007) Resources for mental health scarcity, inequity, and inefficiency. The Lancet 370: 878-879.
- Addis G, Abebe D, Genebo T, Urga K (2002) Perceptions and practices of modern and traditional health practitioners about traditional medicine in Shirka District, Arsi Zone, Ethiopia. Ethiopian Journal of Health Development.16: 19–29.
- Vickers A (2000) Complementary medicine recent advances. BMJ 321: 683.
- Gedif T, Hahn HJ (2002) Epidemiology of herbal drugs use in Addis Ababa, Ethiopia. Pharmacoepidemiol Drug Saf 11: 587-591.
- Giday M, Teklehaymanot T, Animut A, Mekonnen Y (2007) Medicinal plants of the Shinasha, Agew-awi and Amhara peoples in northwest Ethiopia. J Ethnopharmacol 110: 516-525.
- Tshifularo M (2005) Traditional uvulectomy and post-tonsillectomy hemorrhage.
- Jacobsson L, Merdasa F (1991) Traditional perceptions and treatment of mental disorders in western Ethiopia. Acta Psychiatr Scand 84: 475-481.
- Omura S (20030 Traditional Medical Practices, Oromia, Ethiopia, Kenya.
- Gebre-Mariam T, Neubert R, Schmidt PC, Wutzler P, Schmidtke M (2006) Antiviral activities of some Ethiopian medicinal plants used for the treatment of dermatological disorders. J Ethnopharmacol 104: 182-187.
- Oromo E, Roba T (2010) Ethiopia Traditional Medicine & Oromo-cultural profile#section-8 and 10.
- Berhan Y (2008) Medical doctors profile in Ethiopia: production, attrition and retention. In memory of 100-years Ethiopian modern medicine & the new Ethiopian millennium. Ethiop Med J 46 Suppl 1: 1-77.
- WHO (2007) Integration Fifth African Traditional Medicine seminar presentation. Addis Ababa, the development of traditional medicine in a result oriented manner.
- Kassaye KD, Amberbir A, Getachew B, Mussema Y (2006) A historical over view of traditional medicine practices and plicies in Ethiopia. Ethiopian J.Health Dev 20: 127-134.
- WHO (2008) Traditional medicines (Fact Sheet No.134).
- United Nations (UN), Millennium Development Goal (MDG) Report (2006) Efforts made in Reducing Child Mortality in the World.
- Paralegals (2008) The legal concern of women and child rights Training Manual. USAID in collaboration with women and child rights affair office Ethiopia 1:33-34.
- FMOJ, Federal Democratic Republic of Ethiopia (FDRE), Ministry of Justice (MOJ) (2005) Proclamation No. 414/2004 which became law in 2005.
- FMOH (2002) Government policy on TM in Ethiopia.
- FDRE (2009) Federal Democratic Republic of Ethiopia (FDRE). Woreda based Health Sector Planning (WHSP) training manual 1:23-25.
- Feleke, Urge (2006) Ethiopian traditional medicine revised policy. Drug Administration and Control Authority.
- Al-Jauziyah IQ (2005) Healing with the Medicine of the Prophet (Peace be upon him).
- Wondimu T, Asfaw Z, Kelbessa E (2007) Ethnobotanical study of medicinal plants around 'Dheeraa' town, Arsi Zone, Ethiopia. J Ethnopharmacol 112: 152-161.
- Yigzaw Kebede (2010) How far have we gone in understanding TM in Ethiopia? University of Gonder. Ethiop. J Health Biomed Sci 2: 73-74.
- Kavanagh PL, Adams WG, Wang CJ (2009) Quality indicators and quality assessment in child health. Arch Dis Child 94: 458-463.
- WHO (2009) Fifth African traditional medicine Day celebrated.
- Afr TM institute (2009) August 31, 2009, Day for African traditional medicine.
--
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 17699
- [From(publication date):
November-2013 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 12550
- PDF downloads : 5149