Application of Estimation and Projection Package and Spectrum to the Context of Australia's HIV Epidemic
Received: 10-Nov-2011 / Accepted Date: 07-Jan-2012 / Published Date: 15-Jan-2012 DOI: 10.4172/2161-1165.1000111
Abstract
Objectives: Understanding and monitoring the HIV epidemic is essential for developing and evaluating public health responses. The Joint United Nations Programme on AIDS (UNAIDS) Estimation and Projection Package (EPP) and Spectrum have become a standard tool to interpret HIV surveillance systems in many settings, particularly in low- and middle-income countries where surveillance data is often based on serial cross-sectional prevalence studies and not on notifications. EPP has not previously been used to evaluate the HIV epidemic in Australia. We derived best HIV estimates using EPP and assumptions that reflect the current understanding of HIV epidemiology in Australia and compared derived estimates with independent estimates and estimates from mathematical models using backprojections method.
Methods: The epidemic curves for different population groups (i.e., men who have sex with men, injecting drug users, and low-risk population) generated by EPP were combined with antiretroviral therapy (ART) data into a demographic projection model, Spectrum to determine the consequences of the HIV epidemic in Australia.
Results: The overall pattern of the HIV epidemic was consistent with both independent estimates and backprojection modelling estimates. However, the number of HIV-infected females, AIDS-related deaths, and the number in need of ART estimated by EPP were approximately 3.7 times, 20 times, and 6.3 times, respectively higher than independent estimates based on our current surveillance system. EPP estimates of new HIV infections were, however, half the number of independent and back-projection estimates.
Conclusions: These findings suggest that customized tools that are tailored to the unique epidemiology and surveillance mechanisms in each setting are required to enable effective programmatic response and policy.
Keywords: Antiretroviral therapy; HIV/AIDS; Modelling; Surveillance; Transmission risk
158893Introduction
Monitoring the HIV epidemic is essential for assessing the impact of effective HIV prevention interventions, determining public health priorities, and estimating current and future health care needs. Incidence is the best measure for monitoring infections, however, it is difficult to obtain accurate estimates over time [1]. Generally, there are four approaches for estimating HIV incidence, each with its strengths and weaknesses: longitudinal cohort studies; laboratory biomarkers to identify recent infections on cross-sectional samples; repeated cross-sectional measures of HIV prevalence using information about cohort mortality rates or survival after infection [1]; and mathematical modelling of serial cross-sectional data on HIV prevalence or backprojection modelling techniques using surveillance data [2,3]. Although direct longitudinal follow-up of individuals, through cohort studies, provides the most unbiased estimate of HIV incidence compared with the indirect approaches currently available, there are several drawbacks, including the time, expense, and logistic difficulty to conduct them [3]. Thus, trends in HIV prevalence among young adults and groups with high-risk behaviours are used as a proxy measure for incidence trends among adults in generalized and concentrated/lowlevel epidemics, respectively [4].
In Australia, trends in the HIV epidemic have been monitored since 1981 through the notification of AIDS diagnoses, and since 1985 through notification of cases of newly diagnosed HIV infection [5]. Since 1991, further surveillance has been supplemented by national notification of HIV diagnoses with evidence of newly acquired HIV infection, defined as new HIV diagnoses with either evidence of a previous negative test or a diagnosis of primary HIV infection or an indeterminate western blot within 12 months of HIV diagnosis [5-7]. HIV incidence likely peaked in the early to mid 1980s [7] in Australia, but both HIV prevalence (~0.12% in 2008) and annual diagnosed cases (995 in 2008) have remained low compared with many similar settings [8]. To complement Australia’s HIV notification system, surveillance activities include monitoring HIV prevalence among population groups at higher risk such as men who have sex with men (MSM) and injecting drug users (IDUs) as well as low-risk population (e.g., blood donors, antenatal and general heterosexual populations) [8]. Surveillance data [8] and other published literature [7,9,10], have shown that MSM account for more than 70% of newly diagnosed HIV infections in Australia, and that transmission occurs less frequently via other routes such as injecting drug use or heterosexual contact.
Understanding as much of the epidemiological trends of HIV epidemics as possible is essential for developing and evaluating public health responses. Following the recognition of HIV/AIDS in the early 1980s, uncertainty about the present and future magnitude of HIV infection led to the development of many models to estimate current and future numbers of HIV infections and AIDS cases [11]. The Joint United Nations Programme on AIDS (UNAIDS) Estimation and Projection Package (EPP) was first released in late 2001 as a recent tool to assist national programs for use in making national estimates and short-term projections of HIV epidemic in respective countries [12,13]. This generic software package was developed for use in all countries for the purposes of evaluating available surveillance data, producing national ‘consensus’ estimates of the extent of the epidemic, and providing standardized indicators for international reporting. EPP has undergone improvements, and adapting over time as understanding of national epidemics improved [13,14]. Recent versions of EPP allow users to define a national epidemic in terms of a locally relevant set of geographic and population group sub-epidemics to address epidemic complexity more realistically than has been possible in the past [13,15]. EPP has become a standard tool to interpret HIV surveillance systems in many settings, particularly in low- and middle-income countries where surveillance data is often based on serial cross-sectional prevalence studies and not on notifications [16]. EPP has not previously been used to evaluate the HIV epidemic in Australia. Our objectives of this study were to derive best HIV estimates using EPP and assumptions that reflect the current understanding of HIV epidemiology in Australia and to compare derived estimates with independent estimates and estimates from mathematical models using back-projections method.
Methods
Analytic overview of Estimation and Projection Package Model to estimate HIV epidemic in Australia
EPP was used to estimate and project adult HIV prevalence and incidence from surveillance and other pertinent data, with application of appropriate adjustment and calibration procedures [17]. As stated above, transmission of HIV in Australia is primarily through sexual contact between men, and relatively small number of cases are attributed to injecting drug use (~3%), or to heterosexual contact (~23%) [8]. Our study population for EPP therefore consisted of MSM, IDUs, and low-risk population (e.g., general heterosexual population). The input data included population size estimates, HIV seroprevalence data, and antiretroviral therapy (ART) data from several relevant data sources (see details below and Appendix Tables A1-A3) [8,18,19]. EPP 2009 was then used to fit a simple epidemic model (an epidemic curve) to the data using a maximum likelihood method [13]. The model, described in detail elsewhere [12,15,20], includes four parameters (Appendix Table A4): r, the force of infection where a large r will cause HIV prevalence to increase rapidly, while a small value will cause it to increase slowly; f0, the initial fraction of the population at risk of infection, which determines the peak level of the epidemic curve; t0, the start year of the HIV epidemic; and φ, which specifies the behavioural response of the population to the epidemic to influence the rate of decline of the epidemic trajectory from the peak [12,20]. Essentially, using the EPP tool involves tuning these four parameters, such that the underlying statistical function produces a curve that matches available data as best as possible.
The epidemic curves for each of the sub-epidemics (for the different population groups) generated by EPP were then combined with ART data into a demographic projection model, Spectrum Version 3.46, to determine the consequences of the HIV epidemic, including HIV prevalence, the number of new HIV infections, AIDS-related deaths, and future ART needs [17]. Median estimates with lower and upper plausible limits of the HIV epidemic in Australia were generated.
Data sources
For MSM, population size estimates were derived from the Australian Study of Health and Relationships, the Australian Gay Community Periodic Surveys, HIV Futures, the Health in Men cohort study, the Australian National HIV and AIDS Registries, and the Australian Household Census. The data was available for 2001 [18]. HIV prevalence data for this population was derived from the Australian Gay Community Periodic Surveys [19], a self-reported HIV serostatus available for the period between 1998-2006. The Gay Community Periodic Surveys are repeated cross-sectional community-based surveys about the sexual- and HIV-related behaviours of homosexually active men in each of the mainland Australian capital cities, and in some regional areas of Queensland, using an anonymous self-complete questionnaire, with response rates of around 70%. We believe that selfreported HIV prevalence is accurate since there were only 0.5% of HIVnegative gay men recruited in a large Health in Men Study incorrectly believed that they were HIV-negative [21]. HIV prevalence among MSM increased from close to 0% in 1980 to ~10% by 1990 with most of the increase occurring around 1983-85 [7]. HIV prevalence among Australian MSM has remained between 10-15% since 1990 [19].
For IDUs, population size estimates and HIV prevalence data were available for the period 1995-2009 from the Australian Needle and Syringe Program Surveys [22-24]. These surveys monitor HIV and hepatitis C antibody prevalence among IDUs in Australia as well as their behavioural indices of risk [25]. Each year, all clients attending selected Needle and Syringe Program during the designated survey period are invited to complete a brief, anonymous questionnaire and to provide a capillary blood sample for HIV and hepatitis C virus antibody testing [22,25]. HIV prevalence among IDUs increased from 0% in 1980 to about 1% by 1985, and a peak around 1995 (2.1%) [7].
For the general low-risk population, the population size was the remainder of the total population (i.e., total Australian population minus MSM and IDU populations). HIV prevalence among low-risk general population was based on the general female HIV prevalence, and was calculated by a multiplication of the number of people living with HIV with the percentage of female diagnosed with HIV divided by the total female population [8]. HIV prevalence among the low risk population was well under 0.01% until 2003 and then increased to 0.014% by 2008.
The number of adults receiving first- and second-line ART for all sub-populations were obtained from the Australian HIV Observational Database, established in 1999 as an ongoing cohort study among people with HIV infection to monitor the patterns of ART uptake and changes to treatment regimens, as well as monitoring HIV disease progression [8,26]. The reported number of people prescribed each treatment was for people treated in community and day services only. Hospital inpatients, and people treated in pharmaceutical company-sponsored clinical trials or expanded access schemes, were not included [8,26]. ART distribution among sub-populations was as follows: 85% MSM; 12% low-risk population; and 3% IDUs [8]. ART data were available from 1996 to 2009, and was projected to 2015.
Independent estimates of HIV epidemic
Due to our concerns with applying EPP and Spectrum to the context of Australia’s HIV epidemic, we independently estimated the outcome measures and indicators projected by EPP and Spectrum.
Back-projection modelling technique to estimate HIV epidemic
Our group had used a modified back-projection modelling technique to estimate the number of HIV infections and diagnoses in Australia over the period 1975-2006 that made maximal use of all available routine surveillance data sources in Australia, namely: newly diagnosed HIV infections; newly acquired HIV infections; and AIDS diagnoses [2]. Briefly, the model was based on a parametric formulation of the time between the acquisition of HIV infection and the earliest diagnosis of HIV infection obtained from enhanced HIV surveillance systems or from laboratory confirmed testing. The HIV incidence curve was then reconstructed by combining two back-projection estimated HIV incidence curves from AIDS diagnostic data (up to 1994, prior to which effective ART was not available) and HIV diagnostic data using the combined progression rate distribution [2].
Results
EPP Australian HIV/AIDS estimates by eligibility for treatment based on CD4+ cell count is summarized in Table 1. It was estimated that in Australia in 2010, there would be 20,900 people living with HIV infection (31% female), 560 new HIV infections, 477 annual number of AIDS-related deaths, and 15,393 people needed for ART if eligibility for treatment remains at CD4+ cell count <200 cells/μl. The estimated HIV prevalence was 0.13% with a range from 0.09% to 0.17%. There was no significant change in the estimates if eligibility for treatment is at CD4+ cell count <350 cells/μl (the new World Health Organization recommendation [27] and typical in Australia).
| EPP estimates | Independent estimates | |||||
|---|---|---|---|---|---|---|
| LB | Best estimate | UB | LB | Best estimate | UB | |
| Eligibility for treatment remains at CD4+ cell count less than 200 | ||||||
| Total number of HIV infections | 15,684 | 20,900 | 25,624 | 18,440 | 20,284 | 22,128 |
| Number of HIV infections: Female | 5,074 | 6,584 | 7,992 | 1,603 | 1,761 | 1,929 |
| HIV prevalence | 0.09% | 0.13% | 0.17% | 0.09% | 0.10% | 0.11% |
| Annual number of AIDS deaths | 303 | 475 | 646 | 15 | 24 | 55 |
| Number needed for ART | 9,713 | 15,393 | 18,334 | 851 | 1,379 | 1,907 |
| Number of new HIV infections | 212 | 560 | 924 | 805 | 1,011 | 1,120 |
| Eligibility for treatment remains at CD4+ cell count less than 350 | ||||||
| Total number of HIV infections | 16,340 | 21,376 | 26,822 | 18,440 | 20,284 | 22,128 |
| Number of HIV infections: Female | 5,077 | 6,563 | 8,239 | 1,603 | 1,761 | 1,929 |
| HIV prevalence | 0.09% | 0.13% | 0.17% | 0.09% | 0.10% | 0.11% |
| Annual number of AIDS deaths | 336 | 477 | 631 | 15 | 24 | 55 |
| Number needed for ART | 12,261 | 17,204 | 21,771 | 1,703 | 2,758 | 3,813 |
| Number of new HIV infections | 213 | 563 | 929 | 805 | 1,011 | 1,120 |
EPP, Estimation and Projection Package; LB, lower bound; UB, upper bound; ART, antiretroviral therapy.
Table 1: Summary Australian HIV/AIDS estimates among adults, 2010.
Independent estimates of indicators of Australia’s HIV epidemic, based on routine surveillance mechanisms, suggest that the number of people living with HIV in Australia is closely aligned with estimates from EPP (20,900, lower and upper bounds: 15,684-25,624) compared with 20,284 (lower and upper bounds: 18,440-22,128) (Table 1). However, there are marked differences between EPP-derived estimates and other Australian estimates for the number of females infected with HIV (median of 6,584 for EPP compared with 1,761), annual number of AIDS-related deaths (median of 475 for EPP compared with 24), annual number of new HIV infections (median of 560 for EPP compared with 1,011), and number in need of ART (median of between 15,393 and 17,204 for EPP compared with 1,379-2,758).
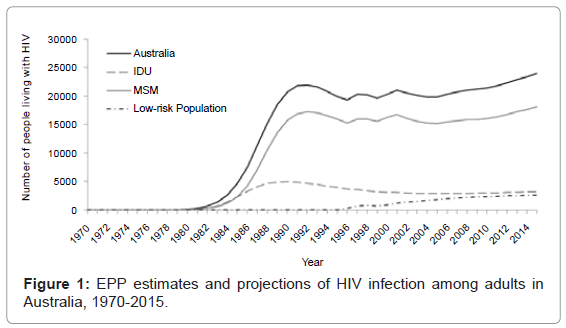
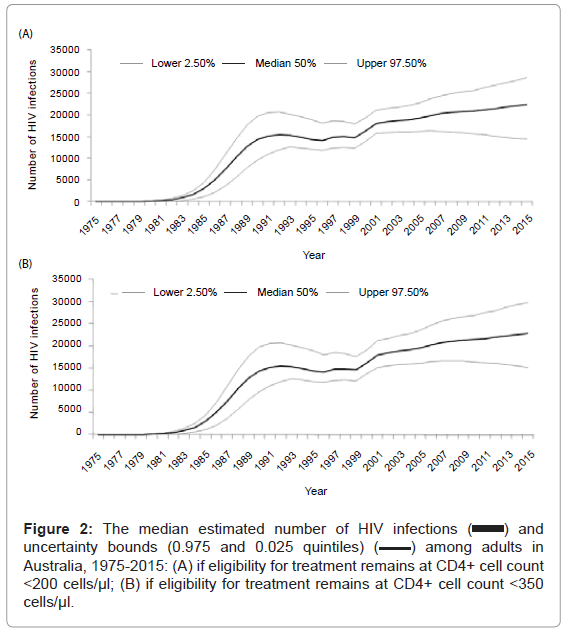
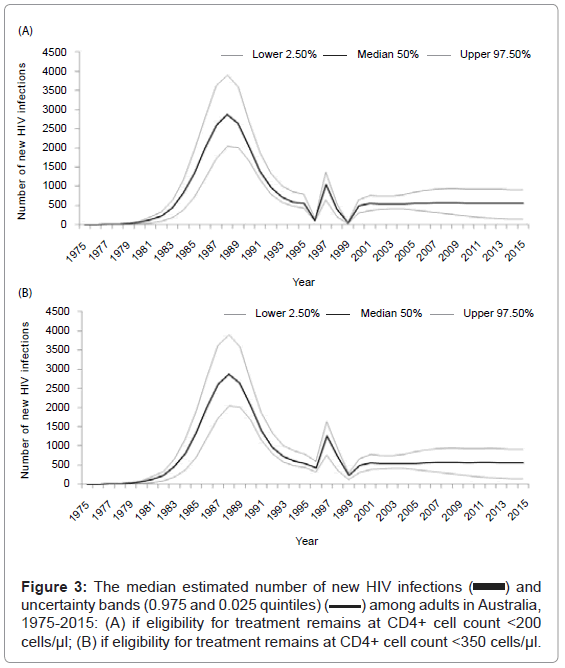
Figure 1 illustrates EPP-derived estimates and projections of the number of adults living with HIV infection for Australia as well as for sub-populations over the period 1970 to 2015. The curve for the Australian population living with HIV plateaued between 1995 and 2006 following a large increase in the early 1990s, and then increased again until 2015. The number of IDUs living with HIV increased from the early 1980s, peaked between 1988 and 1990, then declined until 2000 and remained relatively stable until 2015. The curve for the number of MSM living with HIV is similar to the Australian population. The low-risk population curve increased from 1996 until 2015. Figure 2 and Figure 3 illustrate Spectrum outputs; the median estimated number of adults living with HIV infection and new HIV infections and their uncertainty bounds (0.975 and 0.025 quintiles) among adults in Australia over the period 1975-2015, respectively. EPP-derived number of new HIV infections in Australia increased from the early 1980s, peaked in 1988, then declined sharply until 1996 followed by a smaller peak in 1997-1998 and remained relatively stable until 2015 (Figure 3).
Figure 2: The median estimated number of HIV infections ( ) and uncertainty bounds (0.975 and 0.025 quintiles) (
) and uncertainty bounds (0.975 and 0.025 quintiles) (  ) among adults in Australia, 1975-2015: (A) if eligibility for treatment remains at CD4+ cell count <200 cells/μl; (B) if eligibility for treatment remains at CD4+ cell count <350 cells/μl.
) among adults in Australia, 1975-2015: (A) if eligibility for treatment remains at CD4+ cell count <200 cells/μl; (B) if eligibility for treatment remains at CD4+ cell count <350 cells/μl.
Figure 3: The median estimated number of new HIV infections (  ) and uncertainty bands (0.975 and 0.025 quintiles) (
) and uncertainty bands (0.975 and 0.025 quintiles) ( ) among adults in Australia, 1975-2015: (A) if eligibility for treatment remains at CD4+ cell count <200 cells/μl; (B) if eligibility for treatment remains at CD4+ cell count <350 cells/μl.
) among adults in Australia, 1975-2015: (A) if eligibility for treatment remains at CD4+ cell count <200 cells/μl; (B) if eligibility for treatment remains at CD4+ cell count <350 cells/μl.
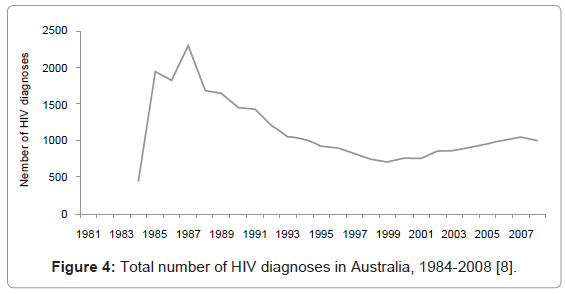
Figure 4 shows independent estimates of the number of new HIV infections (diagnoses) over the period 1981-2008. In comparison with EPP estimates, the annual number of HIV diagnoses peaked in 1987 and declined until 1999 then increased until 2007.
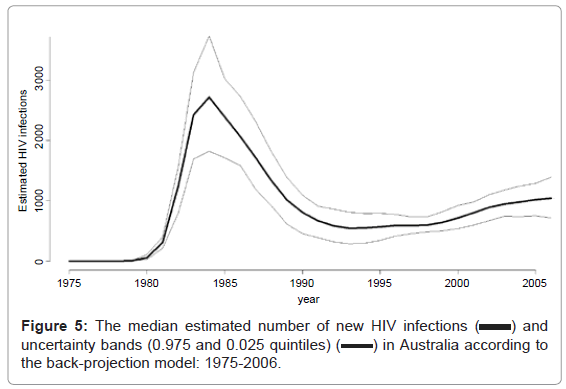
Figure 5 shows the number of new HIV infections over the period 1975-2006 estimated from the back-projection method. In comparison with EPP estimates, the back-projection analyses suggest a peak in the number of new HIV infections in Australia in 1984, followed by a rapid decline until 1994, and then increased in the late 1990s until 2006. Back-projection models estimated that there were a total of 23,350 HIV infections in Australia over the period 1975-2006. Of which, 19,689 (84.3%), 1,050 (4.5%), 1,492 (6.4%), and 1,119 (4.8%) HIV infections were attributed to MSM, IDUs, heterosexual males, and heterosexual females, respectively. It was estimated that there were approximately 6,000 AIDS-related deaths at the end of 2006. Thus, the estimated total number of people living with HIV infection over the period would be approximately 17,350.
Discussion
Our analysis provides a detailed summary of the current state of the Australian HIV epidemic based on a number of evaluation approaches for interpreting our surveillance mechanisms. Overall, the best estimates of EPP represent the extent of HIV in Australia. It represents an average of the sub-populations such as IDU, MSM, and low-risk populations reflecting concentrated HIV epidemic pattern, which shows an increase in the number of HIV infections over the period 1975-2015. The overall pattern of the HIV epidemic is also consistent with independent estimates and back-projection modelling estimates. However, understanding important indicators for informing change in policy or programmatic responses are not well accomplished with EPP. For example, according to EPP, there is approximately 3.7 times the number of HIV-infected females than independent estimates based on our current surveillance system. The annual number of AIDSrelated deaths estimated by EPP is approximately 20 times the number we observe in our surveillance system. AIDS-related deaths have now become rare in Australia with effective combination ART. The EPP estimates may be more appropriate for a resource-constrained country but do not represent the situation in Australia. In Australia, we have consistently been observing an increase in the number of HIV diagnoses, almost certainly reflecting an increase in underlying incidence, and around 1,000 cases per year; EPP estimates are approximately half this number. Lastly, planning for the future care of Australians living with HIV requires understanding of the number in need of life-sustaining ART. There are likely to be around 2,700 people in Australia who have a CD4+ cell count less than 350 cells/μl and in need of ART whereas EPP estimated that 17,000 were in need of ART. These findings suggest that the EPP and Spectrum packages are not precise nor are they ideal for utilizing Australia’s strong HIV surveillance system and data.
HIV in Australia is predominantly confined to populations of MSM and there is not a generalized epidemic like in other countries in our region. Also, due to effective community engagement, the most-atrisk populations test for HIV at a relatively very high frequency. Thus, our HIV surveillance is predominantly based on accurate reporting of the number of HIV diagnoses, which we believe very closely mirrors actual incidence, and not on serial cross-sectional prevalence estimates for informing EPP as in many less-resourced countries. Australia’s national HIV registry has functioned effectively for the last 20 years as a tool for monitoring population patterns and trends. It has been useful for planning and evaluating prevention and treatment programs. Tools to assist in interpreting and gaining further insight into HIV epidemics should be encouraged. But a ‘one size fits all’ approach is unlikely to yield the valuable insight necessary for planning and evaluating effective public health programs. Instead, customized tools that are tailored to the unique epidemiology and surveillance mechanisms in each setting are required. Fortunately, Australia has one of the best surveillance and evaluation mechanisms to enable effective programmatic response and policy. Under this system, Australia has successfully contained the HIV epidemic to a very low prevalence of around 0.1% and avoided the large spread observed in other settings. However, it is highly important that we remain vigilant to effectively monitor the patterns and extent of our epidemic, especially as the profile shifts among specific population groups.
Acknowledgements
This study was funded from the following sources: the Australian Government Department of Health and Ageing; the University of New South Wales; and grant numbers DP1093026 and FT0991990 from the Australian Research Council. The views expressed in this publication do not necessarily represent the position of the Australian Government. The Kirby Institute is affiliated with the Faculty of Medicine, University of New South Wales.
References
- Hallett TB, Zaba B, Todd J, Lopman B, Mwita W, et al. (2008) Estimating incidence from prevalence in generalised HIV epidemics: methods and validation. PLoS Med 5: e80.
- Wand H, Yan P, Wilson D, McDonald A, Middleton M, et al. (2010) Increasing HIV transmission through male homosexual and heterosexual contact in Australia: results from an extended back-projection approach. HIV Med 11: 395-403.
- Lagakos SW, Gable AR (2008) Challenges to HIV prevention--seeking effective measures in the absence of a vaccine. N Engl J Med 358: 1543-1545.
- Mahy M, Warner-Smith M, Stanecki KA, Ghys PD (2009) Measuring the impact of the global response to the AIDS epidemic: challenges and future directions. J Acquir Immune Defic Syndr 52: S152-S159.
- Kaldor J, McDonald A (2003) HIV/AIDS surveillance systems in Australia. J Acquir Immune Defic Syndr 32: S18-S23.
- McDonald AM, Gertig DM, Crofts N, Kaldor JM (1994) A national surveillance system for newly acquired HIV infection in Australia. National HIV Surveillance Committee. Am J Public Health 84: 1923-1928.
- McDonald AM, Crofts N, Blumer CE, Gertig DM, Patten JJ, et al. (1994) The pattern of diagnosed HIV infection in Australia, 1984-1992. AIDS 8: 513-519.
- National Centre in HIV Epidemiology and Clinical Research (2009) HIV/ AIDS, viral hepatitis and sexually transmissible infections in Australia Annual Surveillance Report 2009. National Centre in HIV Epidemiology and Clinical Research, The University of New South Wales.
- Guy RJ, McDonald AM, Bartlett MJ, Murray JC, Giele CM, et al. (2007) HIV diagnoses in Australia: diverging epidemics within a low-prevalence country. Med J Aust 187: 437-440.
- Guy RJ, McDonald AM, Bartlett MJ, Murray JC, Giele CM, et al. (2008) Characteristics of HIV diagnoses in Australia, 1993-2006. Sex Health 5: 91-96.
- Chin J, Sato PA, Mann JM (1990) Projections of HIV infections and AIDS cases to the year 2000. Bull World Health Organ 68: 1-11.
- UNAIDS Reference Group on Estimates, Modelling and Projections (2002) Improved methods and assumptions for estimation of the HIV/AIDS epidemic and its impact: Recommendations of the UNAIDS Reference Group on Estimates, Modelling and Projections. AIDS 16: W1-W14.
- Brown T, Grassly NC, Garnett G, Stanecki K (2006) Improving projections at the country level: the UNAIDS Estimation and Projection Package 2005. Sex Transm Infect 82: iii34-iii40.
- Brown T, Salomon JA, Alkema L, Raftery AE, Gouws E (2008) Progress and challenges in modelling country-level HIV/AIDS epidemics: the UNAIDS Estimation and Projection Package 2007. Sex Transm Infect 84: i5-i10.
- Ghys PD, Brown T, Grassly NC, Garnett G, Stanecki KA, et al. (2004) The UNAIDS Estimation and Projection Package: a software package to estimate and project national HIV epidemics. Sex Transm Infect 80: i5-i9.
- Pisani E, Lazzari S, Walker N, Schwartlander B (2003) HIV surveillance: a global perspective. J Acquir Immune Defic Syndr 32: S3-S11.
- Stover J (2004) Projecting the demographic consequences of adult HIV prevalence trends: the Spectrum Projection Package. Sex Transm Infect 80: i14-i18.
- Prestage G, Ferris J, Grierson J, Thorpe R, Zablotska I, et al. (2008) Homosexual men in Australia: population, distribution and HIV prevalence. Sex Health 5: 97-102.
- Prestage G, Jin F, Zablotska I, Imrie J, Kaldor JM, et al. (2008) Trends in HIV prevalence among homosexual and bisexual men in eastern Australian states. Sex Health 5: 103-107.
- WHO, UNAIDS (2009) Estimating national adult prevalence of HIV-1 in concentrated epidemics.
- Jin F, Prestage GP, McDonald A, Ramacciotti T, Imrie JC, et al. (2008) Trend in HIV incidence in a cohort of homosexual men in Sydney: data from the Health in Men Study. Sex Health 5: 109-112.
- National Centre in HIV Epidemiology and Clinical Research (2009) Australian NSP Survey National Data Report 2004-2008. National Centre in HIV Epidemiology and Clinical Research, The University of New South Wales.
- National Centre in HIV Epidemiology and Clinical Research (2010) Australian NSP Survey National Data Report 2005-2009. National Centre in HIV Epidemiology and Clinical Research, The University of New South Wales.
- National Centre in HIV Epidemiology and Clinical Research (2003) Australian NSP Survey National Data Report 1995-2002. National Centre in HIV Epidemiology and Clinical Research, The University of New South Wales.
- MacDonald M, Wodak AD, Ali R, Crofts N, Cunningham PH, et al. (1997) HIV prevalence and risk behaviour in needle exchange attenders: a national study. The Collaboration of Australian Needle Exchanges. Med J Aust 166: 237-240.
- Petoumenos K, Australian HIV Observational Database (2003) The role of observational data in monitoring trends in antiretroviral treatment and HIV disease stage: results from the Australian HIV observational database. J Clin Virol 26: 209-222.
- World Health Organization (2009) Rapid advice: antiretroviral therapy for HIV infection in adults and adolescents.
- National Centre in HIV Epidemiology and Clinical Research (2009) Return on investment 2: Evaluating the cost-effectiveness of needle and syringe programs in Australia 2009. National Centre in HIV Epidemiology and Clinical Research, The University of New South Wales.
- National Centre in HIV Epidemiology and Clinical Research (2010) Epidemiological and economic impact of potential increased hepatitis C treatment uptake in Australia 2010. National Centre in HIV Epidemiology and Clinical Research, The University of New South Wales.
Citation: Thein HH, Zhang L, Wand H, Wilson DP (2012) Application of Estimation and Projection Package and Spectrum to the Context of Australia’s HIV Epidemic. Epidemiol 2:111. DOI: 10.4172/2161-1165.1000111
Copyright: © 2012 Thein HH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 15568
- [From(publication date): 1-2012 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 10814
- PDF downloads: 4754