Review Article Open Access
Vesicular Stomatitis Virus-Based Vaccines for Prophylaxis and Treatment of Filovirus Infections
Andrea Marzi1*, Heinz Feldmann1, Thomas W. Geisbert2,3 and Darryl Falzarano1
1Laboratory of Virology, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, Montana, USA
2Galveston National Laboratory University of Texas Medical Branch, Galveston, Texas, USA
3Department of Microbiology and Immunology, University of Texas Medical Branch, Galveston, Texas, USA
- *Corresponding Author:
- Dr. Andrea Marzi
Laboratory of Virology
Rocky Mountain Laboratories
903 South 4th Street
Hamilton, MT 59840, USA
Tel: +1-406-375-7421
Fax: +1-406-375-9620
E-mail: marzia@niaid.nih.gov
Received Date: July 28, 2010; Accepted Date: September 07, 2011; Published Date: September 25, 2011
Citation: Marzi A, Feldmann H, Geisbert TW, Falzarano D (2011) Vesicular Stomatitis Virus-Based Vaccines for Prophylaxis and Treatment of Filovirus Infections. J Bioterr Biodef S1:004. doi: 10.4172/2157-2526.S1-004
Copyright: © 2011 Marzi A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Bioterrorism & Biodefense
Abstract
Ebola and Marburg viruses are emerging/re-emerging zoonotic pathogens that cause severe viral hemorrhagic fever with case-fatality rates up to 90% in humans. Over the last three decades numerous outbreaks, of increasing frequency, have been documented in endemic regions. Furthermore, as a result of increased international travel filovirus infections have been imported into South Africa, Europe and North America. Both viruses possess the potential of being used as bioterrorism agents and are classified as category A pathogens. Currently there is neither a licensed vaccine nor effective treatment available, despite substantial efforts being dedicated to understanding filovirus pathogenesis as well as vaccine and drug development. One of the most promising vaccine platforms is based on replication competent recombinant vesicular stomatitis viruses (rVSV) that express a filovirus glycoprotein as the surface antigen. These rVSVs have been extensively studied in rodent and nonhuman primate models of filovirus disease and, in general, have been shown to be 100% protective in pre-exposure prophylaxis. In addition, rVSVs have demonstrated potential for post-exposure treatment, and thus would be particularly useful in the event of intentional release as well as accidental exposures in outbreak and laboratory settings.
Introduction
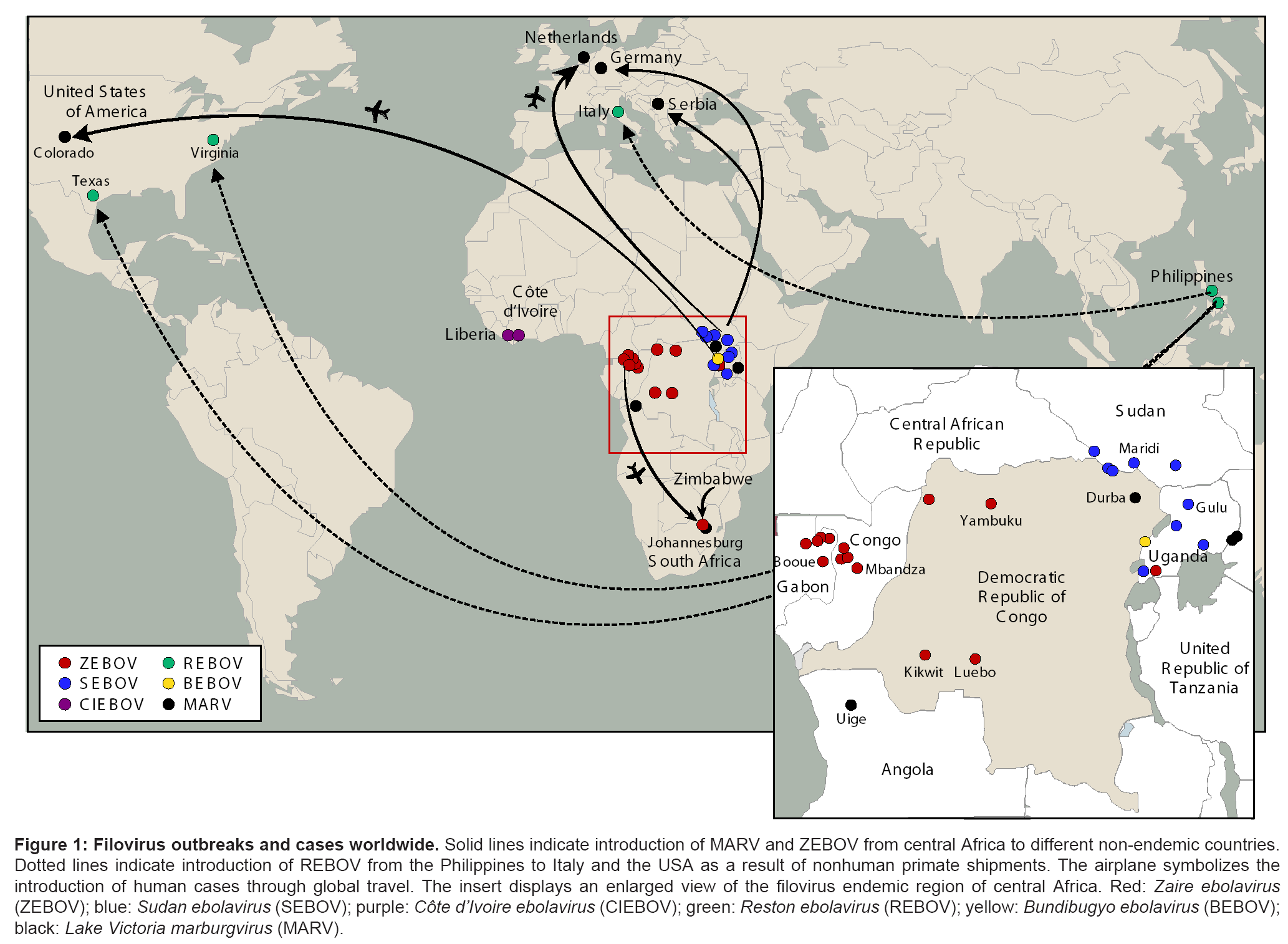
Ebola virus (EBOV) and Marburg virus (MARV), members of the family Filoviridae [1], are the causative agents of severe hemorrhagic fever outbreaks that occur mainly in central Africa [2,3]. More recently, increased worldwide travel has also resulted in imported cases, underlying an increasingly global threat posed by these pathogens (Figure 1). Furthermore, filoviruses are classified as category A agents and thus considered to have the potential to be used for bioterrorism. Together, this has intensified research on filoviruses in a number of maximum containment laboratories worldwide. Both high containment workers and medical personnel in the field are at risk for potential exposures, which have occurred in the past with fatal outcomes [4].
Figure 1: Filovirus outbreaks and cases worldwide. Solid lines indicate introduction of MARV and ZEBOV from central Africa to different non-endemic countries. Dotted lines indicate introduction of REBOV from the Philippines to Italy and the USA as a result of nonhuman primate shipments. The airplane symbolizes the introduction of human cases through global travel. The insert displays an enlarged view of the filovirus endemic region of central Africa. Red: Zaire ebolavirus (ZEBOV); blue: Sudan ebolavirus (SEBOV); purple: Côte d’Ivoire ebolavirus (CIEBOV); green: Reston ebolavirus (REBOV); yellow: Bundibugyo ebolavirus (BEBOV); black: Lake Victoria marburgvirus (MARV).
Filovirus particles are enveloped and contain a nonsegmented, single-stranded, negative-sense RNA genome of approximately 19 kb [5]. EBOV and MARV genomes code for seven structural proteins and in addition EBOV encodes two nonstructural soluble glycoproteins (GP), soluble GP (sGP) and small sGP (ssGP) [5,6]. All known MARV strains belong to the Lake Victoria marburgvirus species, while Ebola virus (EBOV) strains are attributed to four different species: Zaire ebolavirus (ZEBOV), Sudan ebolavirus (SEBOV), Côte d'Ivoire ebolavirus (CIEBOV) and Reston ebolavirus (REBOV) [1]. The recently discovered Bundibugyo ebolavirus (BEBOV) is proposed as a fifth species [7]. The species vary in their apparent pathogenicity in humans with ZEBOV being the most pathogenic (up to 90% case fatality rate), followed by SEBOV (approximately 50% case fatality rate) and BEBOV (approximately 40% case fatality rate) [2]. CIEBOV and REBOV have been shown to be lethal in nonhuman primates, but have not yet been associated with fatal human cases [5,8].
EBOV and MARV replicate systemically resulting in the release of high levels of inflammatory cytokines, coagulation abnormalities and fluid distribution problems. These processes manifest as hemorrhage and vascular leakage, finally leading to multi-organ failure and shock [2,5]. Although EBOV and MARV have been extensively studied in vitro and in various animal models, currently there is neither a licensed vaccine nor approved treatment available. Scientists working in high containment facilities, healthcare workers in Africa and people residing in the endemic regions in Africa remain at risk for potential exposures. In the event of an act of bioterrorism involving filoviruses, the atrisk population could be quite extensive. Thus, countermeasures are considered an important part of any contingency plan for filoviruses.
In the past decade great effort has been made to develop vaccine platforms and treatment strategies against filoviruses. While highly efficacious treatment options are still lacking there are multiple vaccine platforms that have demonstrated efficacy against EBOV and MARV including virus-like-particles (VLPs), Venezuelan equine encephalitis virus replicons (VEEV RP), replication incompetent adenovirus serotype 5 vectors, replication competent recombinant human parainfluenza virus 3 (rHPIV3) and recombinant vesicular stomatitis virus (rVSV) [9]. These platforms have all been tested in the nonhuman primate model and were shown to be protective [10].
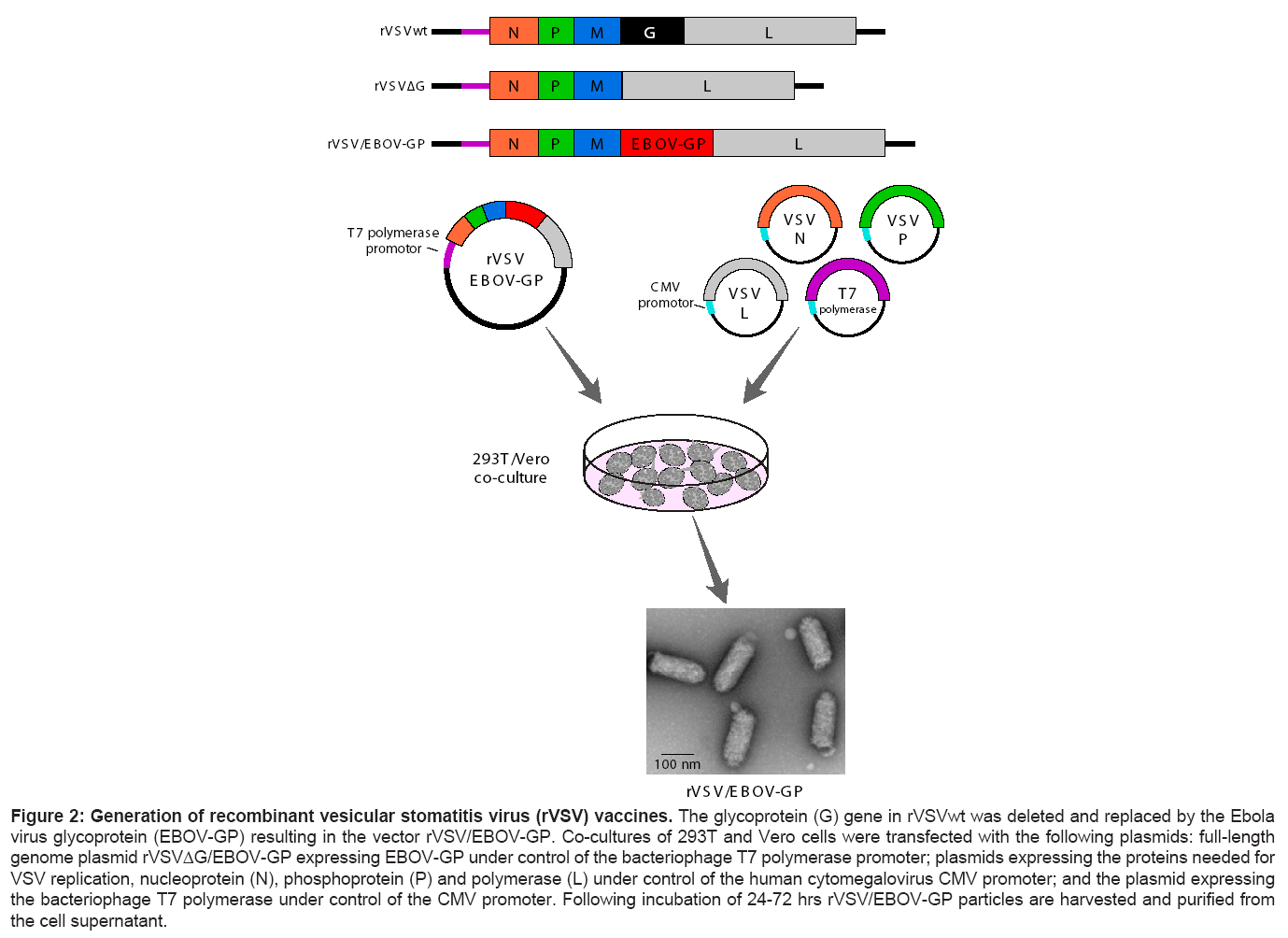
Currently, one of the more promising vaccine approaches against filoviruses is the rVSV platform. VSV is a nonsegmented, negativestranded RNA virus in the family Rhabdoviridae [11]. It is primarily an animal pathogen and is not known to cause severe disease in humans. There are two known serotypes circulating on the American continent, serotypes New Jersey and Indiana [11]. Both VSV serotypes are transmitted by mosquitos, sandflies or blackflies and cause characteristic vesicular lesions on the mouth and teats of livestock [11]. Humans are rarely infected and even in the event of an infection the disease course is generally asymptomatic or mild [11]. VSV is the prototypic rhabdovirus and possesses a number of characteristics that are important for a vaccine vector: replication in almost all known mammalian cell lines, growth to very high titers, and a strong induction of innate and adaptive (humoral as well as cellular) immune responses [12-14]. In addition, there are very low levels of pre-existing immunity to VSV in the general population with the neutralizing immune response primarily directed against the VSV glycoprotein (VSV-G), a viral protein that is not expressed in the filovirus rVSV vaccine vectors (Figure 2) [15,16].
Figure 2: Generation of recombinant vesicular stomatitis virus (rVSV) vaccines. The glycoprotein (G) gene in rVSVwt was deleted and replaced by the Ebola virus glycoprotein (EBOV-GP) resulting in the vector rVSV/EBOV-GP. Co-cultures of 293T and Vero cells were transfected with the following plasmids: full-length genome plasmid rVSVΔG/EBOV-GP expressing EBOV-GP under control of the bacteriophage T7 polymerase promoter; plasmids expressing the proteins needed for VSV replication, nucleoprotein (N), phosphoprotein (P) and polymerase (L) under control of the human cytomegalovirus CMV promoter; and the plasmid expressing the bacteriophage T7 polymerase under control of the CMV promoter. Following incubation of 24-72 hrs rVSV/EBOV-GP particles are harvested and purified from the cell supernatant.
Generation of recombinant vesicular stomatitis virus (rVSV) vaccines
The rVSV vaccine platform is based on the reverse genetics system for an attenuated strain of VSV serotype Indiana and was developed by Rose and colleagues [17]. Briefly, the entire VSV genome was cloned into a plasmid under the control of the bacteriophage T7 polymerase promoter. Subsequently, the open reading frame for the VSV glycoprotein (G) gene was excised and unique restriction enzyme sites for cloning were introduced. The resulting vector can be used to insert foreign virus glycoproteins in place of VSV-G (Figure 2). The deletion of VSV-G has the added benefit of further attenuating the vector virus as VSV-G is one of the major virulence factors [11]. Transfection of the VSV genomic plasmid together with expression plasmids for the viral replication complex [VSV nucleoprotein (N), phosphoprotein (P), and polymerase (L)] and the T7 polymerase into a co-culture of Vero and 293T cells results in viral transcription, protein expression, genome replication and production of recombinant VSV particles that bear the foreign glycoprotein on their surface (Figure 2) [17]. Electron microscopy has shown that these recombinant viral particles possess the same morphology as VSV wild-type (wt) particles (Figure 2) [16]. Initially the rVSV vector was used for HIV vaccine development [15,18], but has since been modified to express the glycoproteins (GP) of other enveloped viruses such as influenza, Lassa, EBOV and MARV [16,19].
To date, two rVSV vaccine vectors have been extensively tested in filovirus animal disease models [20]: rVSV/ZEBOV-GP expressing the GP derived from ZEBOV strain Mayinga, and rVSV/MARV-GP expressing the GP derived from MARV strain Musoke [10,16]. Efficacy testing of rVSV/ZEBOV-GP as either a vaccine or post-exposure therapy has been performed with mouse-adapted (MA-) ZEBOV in mice and hamsters, guinea pig-adapted (GPA-) ZEBOV in guinea pigs, and ZEBOV, SEBOV, CIEBOV and BEBOV in nonhuman primates (NHPs) (Table 1-3). Data on protective efficacy of rVSV/MARV-GP against MARV infection has only been published for macaques (Table 2 and 3).
| antigen | vaccine dose | vaccination route | vaccination | rodent species | challenge doses | challenge virus | viremia/ total | survival/total | reference |
|---|---|---|---|---|---|---|---|---|---|
| ZEBOV-GP | 2x 104 pfu | I.P | day -28 | BALB/c mice | 1x 103 LD50 | MA-ZEBOV | 0/15 | 15/15 | [22] |
| ZEBOV-GP | 2x 104 pfu | I.P | day -28 & -14 | BALB/c mice | 1x 103 LD50 | MA-ZEBOV | N.A | 5/5 | [22] |
| ZEBOV-GP | 2x 104 pfu | I.P | day -28 | BALB/c mice | 1x 104 LD50 | MA-ZEBOV | 0/5 | 5/5 | [22] |
| ZEBOV-GP | 2x 104 pfu | I.P | day -28 | BALB/c mice | 1x 105 LD50 | MA-ZEBOV | 0/5 | 5/5 | [22] |
| ZEBOV-GP | 2x 104 pfu | I.P | day -28 | BALB/c mice | 1x 106 LD50 | MA-ZEBOV | 0/5 | 5/5 | [22] |
| ZEBOV-GP | 2x 103 pfu | I.P | day -28 | BALB/c mice | 1x 103 LD50 | MA-ZEBOV | N.A | 5/5 | [22] |
| ZEBOV-GP | 2x 102 pfu | I.P | day -28 | BALB/c mice | 1x 103 LD50 | MA-ZEBOV | N.A | 5/5 | [22] |
| ZEBOV-GP | 2x 101 pfu | I.P | day -28 | BALB/c mice | 1x 103 LD50 | MA-ZEBOV | N.A | 5/5 | [22] |
| ZEBOV-GP | 2x 100 pfu | I.P | day -28 | BALB/c mice | 1x 103 LD50 | MA-ZEBOV | N.A | 5/5 | [22] |
| ZEBOV-GP | 2x 104 pfu | I.M | day -28 | BALB/c mice | 1x 103 LD50 | MA-ZEBOV | 0/5 | 5/5 | [22] |
| ZEBOV-GP | 2x 104 pfu | I.N | day -28 | BALB/c mice | 1x 103 LD50 | MA-ZEBOV | 0/5 | 5/5 | [22] |
| ZEBOV-GP | 2x 104 pfu | ORAL | day -28 | BALB/c mice | 1x 103 LD50 | MA-ZEBOV | 0/10 | 10/10 | [22] |
| ZEBOV-GP | 2x 104 pfu | I.P | day -21 | BALB/c mice | 1x 103 LD50 | MA-ZEBOV | 0/20 | 20/20 | [23] |
| ZEBOV-GP | 2x 105 pfu | I.P | day -21 | Guinea pig | 1x 103 LD50 | GPA-ZEBOV | N.A | 14/14 | [23] |
| ZEBOV-GP* | 2x 105 pfu | I.P | day -21 | Guinea pig | 1x 103 LD50 | GPA-ZEBOV | N.A | 4/4 | [23] |
| ZEBOV-GP | 1x 105 pfu | I.P | day -28 | Syrian hamster | 1x 102 LD50 | MA-ZEBOV | 0/6 | 6/6 | [24] |
| ZEBOV-GP | 1x 105 pfu | I.P | day -14 | Syrian hamster | 1x 102 LD50 | MA-ZEBOV | N.A | 5/5 | [24] |
| ZEBOV-GP | 1x 105 pfu | I.P | day -7 | Syrian hamster | 1x 102 LD50 | MA-ZEBOV | N.A | 5/5 | [24] |
| ZEBOV-GP | 1x 105 pfu | I.P | day -3 | Syrian hamster | 1x 102 LD50 | MA-ZEBOV | N.A | 5/5 | [24] |
* ZEBOV-GP (strain Kikwit)
N.D. = Not Determined
Table 1: Preventive EBOV rVSV vaccination studies in rodents.
| antigen | vaccine dose | vaccination route | macaque species | challenge virus | challenge route | viremia/ total | disease/ total | survival/ total | reference |
|---|---|---|---|---|---|---|---|---|---|
| ZEBOV-GP | 1x 107 pfu | I.M | cynomolgus | ZEBOV | I.M | 0/4 | 0/4 | 4/4 | [25] |
| MARV-GP | 5x 107 pfu | I.M | cynomolgus | MARV Musoke | I.M | 0/4 | 0/4 | 4/4 | [25] |
| MARV-GP | 2x 107 pfu | I.M | cynomolgus | MARV Angola | I.M | 0/3 | 0/3 | 3/3 | [28] |
| MARV-GP | 2x 107 pfu | I.M | cynomolgus | MARV Ravn | I.M | 0/3 | 0/3 | 3/3 | [28] |
| MARV-GP | 2x 107 pfu | I.M | cynomolgus | MARV Musoke | I.M | 0/1 | 0/1 | 1/1 | [28] |
| ZEBOV-GP | 2x 107 pfu | I.M | cynomolgus | ZEBOV | AEROSOL | 0/3 | 0/3 | 3/3 | [26] |
| MARV-GP | 2x 107 pfu | I.M | cynomolgus | MARV Musoke | AEROSOL | 0/4 | 0/4 | 4/4 | [26] |
| ZEBOV-GP | 2x 107 pfu | I.N | cynomolgus | ZEBOV | I.M | n.a. | 0/4 | 4/4 | [27] |
| ZEBOV-GP | 2x 107 pfu | ORAL | cynomolgus | ZEBOV | I.M | n.a | 0/4 | 4/4 | [27] |
| ZEBOV-GP | 2x 107 pfu | I.M | cynomolgus | ZEBOV | I.M | n.a. | 0/2 | 2/2 | [27] |
| ZEBOV-GP SEBOV-GP MARV-GP | 1x 107 pfu each |
I.M | cynomolgus | ZEBOV | I.M | 0/3 | 0/3 | 3/3 | [29] |
| ZEBOV-GP SEBOV-GP MARV-GP | 1x 107 pfu each |
I.M | cynomolgus | SEBOV | I.M | 0/2 | 0/2 | 2/2 | [29] |
| ZEBOV-GP SEBOV-GP MARV-GP | 1x 107 pfu each |
I.M | cynomolgus | CIEBOV | I.M | 0/3 | 0/3 | 3/3 | [29] |
| ZEBOV-GP SEBOV-GP MARV-GP | 1x 107 pfu each |
I.M | cynomolgus | MARV Musoke | I.M | 0/3 | 0/3 | 3/3 | [29] |
| ZEBOV-GP | 3x 107 pfu | I.M | cynomolgus | SEBOV | I.M | 1/1 | 1/1 | 0/1 | [29] |
| SEBOV-GP ZEBOV-GP MARV-GP | 1x 107 pfu each |
I.M | rhesus | SEBOV | I.M | 0/3 | 0/3 | 3/3 | [29] |
| ZEBOV-GP | 2x 107 pfu | I.M | cynomolgus | BEBOV | I.M | 4/4 | 4/4 | 3/4 | [30] |
| CIEBOV-GP | 2x 107 pfu | I.M | cynomolgus | BEBOV | I.M | 3/3 | 3/3 | 1/3 | [30] |
N.D. = not determined
Table 2: Prseventive filovirus rVSV vaccination studies in NHPs.
| challenge virus | challenge route | time post infection | antigen | rVSV dose | rVSV route | species | viremia/ total | disease/total | survival/ total | reference |
|---|---|---|---|---|---|---|---|---|---|---|
| MA-ZEBOV | I.P | 30 min | ZEBOV-GP | 2x 105 pfu | I.P | BALB/c mice | N.A | 5/5 | 5/5 | [21] |
| MA-ZEBOV | I.P | 24 hrs | ZEBOV-GP | 2x 105 pfu | I.P | BALB/c mice | N.A | 5/5 | 5/5 | [21] |
| GPA-ZEBOV | I.P | 1 hr | ZEBOV-GP | 2x 105 pfu | I.P | Guinea pigs | N.A | 6/6 | 5/6 | [21] |
| GPA-ZEBOV | I.P | 24 hrs | ZEBOV-GP | 2x 105 pfu | I.P | Guinea pigs | N.A | 6/6 | 3/6 | [21] |
| MA-ZEBOV | I.P | 0 min | ZEBOV-GP | 1x 105 pfu | I.P | Syrian hamsters | N.A | 0/5 | 5/5 | [24] |
| MA-ZEBOV | I.P | 24 hrs | ZEBOV-GP | 1x 105 pfu | I.P | Syrian hamsters | N.A | 0/5 | 5/5 | [24] |
| MA-ZEBOV | I.P | 48 hrs | ZEBOV-GP | 1x 105 pfu | I.P | Syrian hamsters | N.A | 5/5 | 0/5 | [24] |
| ZEBOV | I.M | 20-30 min | ZEBOV-GP | 2x 107 pfu | I.M | Rhesus macaques | 8/8 | 8/8 | 4/8 | [21] |
| SEBOV | I.M | 20-30 min | SEBOV-GP | 2x 107 pfu | I.M | Rhesus macaques | 2/4 | 4/4 | 4/4 | [35] |
| MARV Musoke | I.M | 20-30 min | MARV-GP | 1x 107 pfu | I.M | Rhesus macaques | 0/5 | 0/5 | 5/5 | [33] |
| MARV Musoke | I.M | 24 hrs | MARV-GP | 2x 107 pfu | I.M | Rhesus macaques | 3/6 | 4/6 | 5/6 | [34] |
| MARV Musoke | I.M | 48 hrs | MARV-GP | 2x 107 pfu | I.M | Rhesus macaques | 5/6 | 6/6 | 2/6 | [34] |
N.D. = not determined
Table 3: Post-exposure filovirus rVSV treatment in rodents & NHPs.
Preventive vaccine approaches
Rodent models: New EBOV vaccine platforms are commonly tested in rodent models before they undergo efficacy testing in NHPs. For EBOV, the rVSV/ZEBOV-GP vaccine has been extensively tested in BALB/c mice, and to a lesser extent in Syrian golden hamsters and Hartley guinea pigs. BALB/c mice are completely protected following a single intraperitoneal (i.p.) vaccination with 2x104 pfu of rVSV/ ZEBOV-GP per mouse at 28, 21, 14, 7 or even one day prior to lethal challenge with MA-ZEBOV [21-23]. Remarkably, a vaccine dose as low as 2 pfu resulted in complete protection in the ZEBOV mouse model [21]. In addition, it was shown that there is no difference in survival outcome when rVSV/ZEBOV-GP was given 28 days prior to challenge via the i.p., intranasal (i.n.), intramuscular (i.m.), or oral route [22]. The question of long-term immunity provided by the rVSV vaccine was analyzed in the ZEBOV mouse model, and showed that a single i.p. dose of 2x105 pfu rVSV/ZEBOV-GP was still protective 9 months after immunization [22]. As mice appear to be easily protected it was necessary to test rVSV vaccine efficacy in other rodent models. The well-established guinea pig model for ZEBOV was used to confirm the data obtained in the mouse model. Guinea pigs vaccinated with 2x105 pfu rVSV/ZEBOV-GP were challenged with a lethal dose of GPAZEBOV three weeks after vaccination. The vaccinated animals showed no signs of illness, whereas control guinea pigs developed disease and succumbed to infection between day 7 and 9 [23]. Single rVSV vaccines expressing BEBOV-, CIEBOV-, REBOV- or SEBOV-GP did not elicit cross-protective immunity against ZEBOV in the guinea pig model [23], indicating that GP is not sufficient as a cross-species protective immunogen for EBOV. In a more recent study, hamsters were also protected when vaccinated with 1x105 pfu rVSV/ZEBOV-GP 14, 7 or 3 days prior to a lethal challenge with MA-ZEBOV [24]. This study also determined the protective efficacy of a bivalent vaccine vector expressing ZEBOV-GP in addition to the Andes virus glycoprotein (ANDV-GPC), a New World hantavirus, demonstrating that bivalent rVSV vectors are capable of providing complete protection. In summary, the rVSV vaccines have proven to be very potent in ZEBOV rodent models.
Macaque models: Cynomolgus macaques have been established as the "gold standard" model for filovirus infections, thus this model was chosen to test the efficacy of the rVSV/ZEBOV-GP and rVSV/ MARV-GP vaccines. The first study published by Jones et al. showed that a single dose of 1x107 pfu rVSV/ZEBOV-GP provided complete protection of all NHPs against a lethal dose of ZEBOV (1,000 pfu i.m.) 4 weeks following vaccination (Table 2) [25]. Furthermore, all animals were protected from disease and did not show any evidence of ZEBOV viremia. At the time of challenge the NHPs had low to moderate-IgG levels and no neutralizing antibodies, but developed a strong cellular immune response as well as neutralizing antibody titers following ZEBOV infection [25]. Another study demonstrated that 2x107 pfu rVSV/ZEBOV-GP administered i.m. protected NHPs against aerosol infection with 1,000 pfu ZEBOV (Table 2) [26]. The animals developed similar immune responses after vaccination and aerosol challenge as described for i.m. ZEBOV infection and were completely protected. A third study focused on different routes of immunization for the rVSV/ ZEBOV-GP vaccine and no difference in protective efficacy could be observed after i.n., oral or i.m. administration of a single vaccine dose containing 2x107 pfu rVSV administered 28 days prior to homologous challenge (Table 2) [27].
Similar studies have been performed using the rVSV/MARV-GP vaccine and MARV strain Musoke as the challenge virus. A single dose of 2x107 pfu rVSV/MARV-GP given i.m. was protective against a lethal i.m. or aerosol challenge (1,000 pfu) with MARV strain Musoke (Table 2) [25,26]. In contrast to EBOV, there is only one MARV species and the rVSV/MARV-GP vaccine is not only protective against challenge with the homologous strain (MARV strain Musoke), but also against MARV strains Angola and Ravn [28]. The IgG and neutralizing antibody responses induced by the rVSV/MARV-GP vaccine seem to be cross-protective within species [28] suggesting that a single MARV vaccine will be protective against all currently known MARV strains.
EBOV and MARV overlap in their endemic areas in sub-Saharan Africa; therefore, a single vaccine that is protective against both filoviruses is highly desirable. In the first attempt to accomplish this task, equal amounts (1x107 pfu) of rVSV/MARV-, rVSV/ZEBOV- and rVSV/SEBOV-GP were combined and a single blended vaccine was given to cynomolgus macaques [29]. All NHPs survived lethal challenge with either 1,000 pfu ZEBOV, SEBOV or MARV. Interestingly, three animals receiving this blended vaccine were infected with 1,000 pfu CIEBOV and did not develop any signs of disease, despite the lack of CIEBOV-specific antigen in the vaccine [29]. This is the first study indicating that the rVSV vaccines can induce cross-species protective immune responses in nonhuman primates. Falzarano and colleagues used rVSV/ZEBOV-GP and rVSV/CIEBOV-GP to determine whether either of these vaccines alone could induce cross-protection against the newly emerged BEBOV, which is approximately 75% lethal in cynomolgus macaques [30,31]. Only one out of four animals vaccinated with rVSV/ZEBOV-GP succumbed to infection while two out of three animals vaccinated with rVSV/CIEBOV-GP did not survive (Table 2). Animals surviving BEBOV infection developed signs of mild to moderate disease and virus could be isolated from their blood indicating that protection was not complete [30].
The fact that rVSVs are replication-competent vectors raises questions regarding their safety. In addition, potential filovirus vaccine target populations in Africa may be immunocompromised especially as a result of HIV infection, which could increase the risk of adverse effects following vaccination. Geisbert et al. have addressed this issue through vaccination of simian-human immunodeficiency virus (SHIV)-infected, immunocompromised rhesus macaques with rVSV/ZEBOV-GP [32]. Six animals received a single dose of 1x107 pfu VSV/ZEBOV-GP i.m. and three animals received saline as control. None of the animals showed clinical signs of illness indicating that no adverse effects were associated with vaccination. All nine subjects were subsequently challenged with 1,000 pfu ZEBOV (strain Kikwit) on day 31 after immunization. The three control animals succumbed to lethal ZEBOV infection while four of six vaccinated animals survived. Two of the surviving NHPs in the vaccinated group developed mild but characteristic signs of Ebola hemorrhagic fever (EHF), while the other two animals showed no signs of disease. Interestingly, the two non-survivors in the vaccinated group had the lowest CD4+ cells count and highest SHIV viremia, indicating that CD4+ T cell responses may be important for protection [32]. This data suggests that even in immunocompromised individuals, rVSV vectors seem to be safe and efficacious.
In summary, the rVSV vaccine vectors have provided complete and largely sterile protection in filovirus NHP models against homologous challenge when administered prophylactically. Moreover, protective immunity against multiple EBOV and MARV species/strains has been achieved with a blended vaccine approach. The single-shot, blended vaccine currently presents the most feasible vaccine strategy for implementation in endemic regions of Africa while also being suitable for the protection of maximum containment laboratory workers worldwide. In the event of an act of bioterrorism involving filoviruses, these vaccine vectors might also prove useful as time-toprotection appears to be relatively rapid, thus they could be used to limit secondary spread of infections to susceptible populations.
Post-exposure treatment approaches
Rodent models: In the event of an intentional filovirus release, post-exposure vaccination (or treatment) would be highly desirable as there is little to no time for wide-coverage preventative vaccination. It had been demonstrated that a single dose of 2x104 pfu of rVSV/ ZEBOV-GP was completely protective in mice as a preventive vaccine when administered as late as 24 hrs prior to lethal MA-ZEBOV infection (Table 3) [21,22]. This finding suggested that the rVSV vectors could be used for post-exposure treatment. The same rVSV dose was subsequently tested in mice for its protective efficacy when administered either 30 min or 24 hrs post challenge with 1,000 LD50 of MA-ZEBOV [21]. The mice developed mild clinical symptoms including slight weight loss, indicative of virus replication, but all treated animals survived. Encouraged by this outcome, the experiment was repeated in guinea pigs. Groups of six animals were treated with a single dose of 2x105 pfu rVSV/ZEBOV-GP 1 hr or 24 hrs post infection with 1,000 LD50 of GPA-ZEBOV (Table 3) [21]. None of the groups were fully protected; however, 83% of guinea pigs in the 1 hr post challenge group and 50% of guinea pigs in the 24 hr post infection group survived after developing signs of disease [21]. A similar study was performed in hamsters with a single dose of 1x105 pfu rVSV/ZEBOVGP administered immediately following MA-ZEBOV challenge (day 0), or 24 hrs or 48 hrs after challenge [24]. All hamsters treated up to 24 hrs post lethal infection with rVSV/ZEBOV-GP survived, whereas all animals succumbed in the 48 hrs treatment group despite showing delayed time to death. Taken together, rVSV/ZEBOV-GP has the potential to be used for post-exposure treatment and thus was tested in the macaque models.
Macaque models: Three different rVSVs expressing the GP from either MARV (strain Musoke), SEBOV (strain Boniface), and ZEBOV (strain Mayinga) have been tested for post-exposure treatment in the rhesus macaque model of filovirus infections (Table 3). The rhesus macaque model was chosen for these experiments because the mean time to death following lethal filovirus infections is generally longer than with cynomolgus macaques [4,5]. Interestingly, rVSV/MARVGP (strain Musoke) displays the greatest potential for post-exposure treatment. When given 20-30 min following MARV (strain Musoke, 1,000 pfu) infection this vector protected 100% of rhesus macaques from viremia and disease [33]. This experiment was followed up by another study where two groups of six animals were treated with rVSV/MARV-GP 24 or 48 hrs following lethal MARV (strain Musoke) infection [34]. Treatment 24 hrs post-infection resulted in 83% survival, with one out of six animals showing signs of disease and three of the six testing positive for viral RNA in the blood. When treatment was delayed until 48 hrs post infection, the survival rate dropped to 33% and all animals showed moderate to severe signs of disease, and 83% developed viremia [34].
However, the rVSV/SEBOV-GP vector also protected 100% of the animals from lethal outcome when administered 20-30 min post challenge with SEBOV [35]. All four treated animals showed signs of illness and two NHPs developed viremia [35]. By comparison, the rVSV/ZEBOV-GP seems to be the least potent vector for post-exposure treatment as 50% of rhesus macaques infected with ZEBOV (strain Kikwit, 1,000 pfu) and subsequently treated with rVSV/ZEBOV-GP 20-30 min later, succumbed to infection. All survivors developed moderate signs of illness and were viremic. While it appears that this vector is highly effective as a preventive vaccine, it seems less effective as a post-exposure strategy [21]. However, MARV (strain Musoke) and particularly SEBOV infections typically progress slower in NHPs than infections with ZEBOV [4,5], which likely contributes to the greater success of the rVSV/MARV-GP and rVSV/SEBOV-GP in postexposure treatment. It would be interesting to determine post-exposure treatment efficacy against infection with MARV, strain Angola, which shows the fastest disease progression of all known filoviruses [36].
Correlates and mechanisms of protection
The mechanisms of protection of the rVSV vectors in pre-exposure vaccination are not understood. It also appears that there might be differences between the rodent models, in particular the mouse, and the NHP models. The humoral immune response is certainly sufficient to protect mice from lethal challenge as was clearly shown with successful plasma transfer studies [22] as well as treatment studies with neutralizing antibodies [37-39]. For prophylactic vaccination of NHPs, it appears that adaptive immune responses, both cellular and humoral, are required. The MARV rVSV vector seems to elicit stronger non-neutralizing antibody responses whereas the EBOV rVSV vectors induce stronger cellular immune responses. Further studies, such as specific depletion of T and B cells, should better define the mechanism of protection. Nevertheless, a strong non-neutralizing antibody response appears to correlate with protection and could be used as a marker for successful vaccination.
The mechanisms of protection for post-exposure rVSV treatment also remain unknown. VSV is known to act as a very strong inducer of innate immune responses, which might be sufficient to overcome filovirus-driven suppression of these responses [11], thus inhibiting filovirus replication and spread of infection. It has been shown that rVSVs infect the same target cells as filoviruses [16] resulting in a block in EBOV and MARV replication potentially as a result of viral interference. Again, the development of a humoral non-neutralizing immune response is associated with survival but is unlikely to be the mechanism of protection as its development would be too late [21].
Vaccine safety & environmental impact
Since rVSV filovirus vaccines are replication competent, vaccine safety has been a significant concern and as such was taken into account during vector design. Importantly, there has been no indication of potential safety issues using multiple rVSV vectors despite being used in a large number of animal studies. The rVSV vectors are based on an attenuated strain of VSV serotype Indiana and in addition the VSV glycoprotein, a key determinant for VSV pathogenicity [11], has been replaced with a filovirus glycoprotein. This has resulted in replication competent vectors that are attenuated both in vitro [16] and in vivo (Marzi et al., unpublished data). Safety concerns have also been addressed through evaluation of the rVSV filovirus vaccines in two immunocompromised animal models. Non-obese diabetic severe combined immunodeficiency (NOD/SCID) mice and SHIV-infected macaques showed no indication of adverse effects following rVSV vaccination and in fact the vaccines were efficacious against lethal challenge (albeit not completely) [22,32]. Based on efficacy and safety data in animal models, the rVSV/ZEBOV-GP vaccine was recently used for post-exposure treatment of a laboratory exposure with only moderate reactions being reported [40].
While all rVSV animal studies performed so far have only resulted in low level transient rVSV viremia with no detectable shedding of infectious vaccine virus, the potential impact of live attenuated vaccine vectors on the environment should not be underestimated [25-30,32]. Furthermore, this vector is not expected to cause disease in livestock as a result of the lack of VSV-G, however, further safety testing should be performed in animals of interest (cattle, donkeys, mules, horses, swine, etc.). In addition, VSV has a very low transmission rate in nature [26], and there is no evidence that rVSV vectors would accumulate mutations that would result in increased virulence or transmissibility to a broader host range. In this regard, the currently used live measles vaccine that has been widely used for five decades has shown no evidence of acquiring increased virulence [41,42]. Together, the efficacy and safety data strongly support further development of these vaccine vectors for human use.
Conclusion
Most filovirus outbreaks have been reported in sub-Saharan Africa, but with increased global travel EBOV and MARV have the potential to be imported worldwide (Figure 1). Although, larger epidemics in Africa have been prevented as a result of patient isolation, contact tracing and extensive surveillance efforts, the threat of filovirus infection remains ever present particularly with the potential misuse of these viruses as agents of bioterrorism. Significant progress has been made over the last 15 years towards filovirus vaccine development, with multiple potential vaccine candidates that are highly efficacious.
The rVSV vectors have been evaluated in a variety of rodent and NHP models, clearly demonstrating their safety and efficacy as a prophylactic vaccine platform for filoviruses and perhaps other viral hemorrhagic fever pathogens [9,10]. A single shot, blended rVSV approach is currently the best strategy to provide broad coverage for filoviruses in overlapping endemicity zones in Africa (Figure 1). Multi-dose regimens with rVSV vectors seem possible due to the lack of neutralizing antibody responses to the vector backbone (VSVG- deficient) opening the opportunity for continuing vaccination programs. In addition to its efficacy as a preventive vaccine, the rVSV vectors have also shown value in post-exposure treatment. This is an important asset of a vaccine platform in the event of a bioterrorism attack or an accidental laboratory exposure as was shown in 2009 when rVSV/ZEBOV-GP was first used as a post-exposure treatment in a laboratory accident [40]. Thus, the next obvious step for the rVSV filovirus vaccine platform is the move into phase I clinical trials. For this to occur, vaccine stocks need to be produced to GLP/GMP standards and the correlates and mechanisms of protection need to be better defined to allow licensing. Currently, the rVSV filovirus vectors seem to be the most promising choice for a fast-acting preventive and therapeutic vaccine platform.
Acknowledgements
The authors thank Anita Mora and Austin Athman (Visual and Medical Arts Unit, Rocky Mountain Laboratories, National Institute of Allergy and Infectious Diseases, National Institutes of Health) for support with graphics. Filovirus work at the Rocky Mountain Laboratories is funded by the Intramural Research Program, NIAID, NIH. Work on rVSV-based filovirus vaccines at UTMB Galveston is supported in part by the Department of Health and Human Services, NIH grant AI082197.
References
- Feldmann H, TW Jahrling P (2005) Filoviridae In: Fauquet CM MA Maniloff J Desselberger U Ball LA editor Virus Taxonomy: VIIIth Report of the International COmmittee on Taxonomy of Viruses. London: Elsevier/Academic Press.
- Feldmann H, Geisbert TW (2011) Ebola haemorrhagic fever. Lancet 377: 849- 862.
- Hartman AL, Towner JS, Nichol ST (2010) Ebola and marburg hemorrhagic fever. Clin Lab Med 30: 161-177.
- Kuhn J, Calisher C H (2008) Filoviruses - A Compendium of 40 Years of Epidemiological, Clinical, and Laboratory Studies.
- Sanchez A, Geisbert TW, Feldmann H (2006) Filoviridae: Marburg and Ebola viruses In: Knipe DM, Howley PM, editor. Fields Virology. Philadelphia: Lippincott Williams & Wilkins. 1409-1448.
- Mehedi M, Falzarano D, Seebach J, Hu X, Carpenter MS, et al. (2011) A new Ebola virus nonstructural glycoprotein expressed through RNA editing. J Virol 85: 5406-5414.
- Towner JS, Sealy TK, Khristova ML, Albarino CG, Conlan S, et al. (2008) Newly discovered ebola virus associated with hemorrhagic fever outbreak in Uganda. PLoS Pathog 4: e1000212.
- Le Guenno B, Formenty P, Wyers M, Gounon P, Walker F, et al. (1995) Isolation and partial characterisation of a new strain of Ebola virus. Lancet 345: 1271-1274.
- Falzarano D, Geisbert TW, Feldmann H (2011) Progress in filovirus vaccine development: evaluating the potential for clinical use. Expert Rev Vaccines 10: 63-77.
- Geisbert TW, Bausch DG, Feldmann H (2010) Prospects for immunisation against Marburg and Ebola viruses. Rev Med Virol 20: 344-357.
- Lyles DS, Rupprecht CE (2006) Rhabdoviridae. In: Knipe DM, Howley PM editor Fields Virology Philadelphia, USA: Lippincott WIlliams & Wilkins.
- Zinkernagel RM, Adler B, Holland JJ (1978) Cell-mediated immunity to vesicular stomatitis virus infections in mice. Exp Cell Biol 46: 53-70.
- Zinkernagel RM, Althage A, Holland J (1978) Target antigens for H-2-restricted vesicular stomatitis virus-specific cytotoxic T cells. J Immunol 121: 744-748.
- Fehr T, Bachmann MF, Bluethmann H, Kikutani H, Hengartner H, et al. (1996) T-independent activation of B cells by vesicular stomatitis virus: no evidence for the need of a second signal. Cell Immunol 168: 184-192.
- Rose NF, Marx PA, Luckay A, Nixon DF, Moretto WJ, et al. (2001) An effective AIDS vaccine based on live attenuated vesicular stomatitis virus recombinants. Cell 106: 539-549.
- Garbutt M, Liebscher R, Wahl-Jensen V, Jones S, Moller P, et al. (2004) Properties of replication-competent vesicular stomatitis virus vectors expressing glycoproteins of filoviruses and arenaviruses. J Virol 78: 5458-5465.
- Lawson ND, Stillman EA, Whitt MA, Rose JK (1995) Recombinant vesicular stomatitis viruses from DNA. PNAS 92: 4477-4481.
- Rose NF, Roberts A, Buonocore L, Rose JK (2000) Glycoprotein exchange vectors based on vesicular stomatitis virus allow effective boosting and generation of neutralizing antibodies to a primary isolate of human immunodeficiency virus type 1. J Virol 74: 10903-10910.
- Schwartz JA, Buonocore L, Suguitan A Jr., Hunter M, Marx PA, et al. (2011) Vesicular stomatitis virus-based H5N1 avian influenza vaccines induce potent cross-clade neutralizing antibodies in rhesus macaques. J Virol 85: 4602-4605.
- Bente D, Gren J, Strong JE, Feldmann H (2009) Disease modeling for Ebola and Marburg viruses. Dis Model Mech 2: 12-17.
- Feldmann H, Jones SM, Daddario-DiCaprio KM, Geisbert JB, Stroher U, et al. (2007) Effective post-exposure treatment of Ebola infection. PLoS Pathog 3: e2.
- Jones SM, Stroher U, Fernando L, Qiu X, Alimonti J, et al. (2007) Assessment of a vesicular stomatitis virus-based vaccine by use of the mouse model of Ebola virus hemorrhagic fever. J Infect Dis 196 : S404-412.
- Marzi A, Ebihara H, Callison J, Groseth A, Williams KJ, et al. (2011) Vesicular stomatitis virus based Ebola vaccines with improved cross-protective efficacy. J Infect Dis. 3:S1066-74.
- Tsuda Y, Safronetz D, Brown K, LaCasse R, Marzi A, et al. (2011) Protective efficacy of a bivalent recombinant Vesicular Stomatitis Virus vaccine in the Syrian hamster model of lethal Ebola virus infection. J Infect Dis. 3:S1090-7.
- Jones SM, Feldmann H, Stroher U, Geisbert JB, Fernando L, et al. (2005) Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses. Nat Med 11: 786-790.
- Geisbert TW, Daddario-Dicaprio KM, Geisbert JB, Reed DS, Feldmann F, et al. (2008) Vesicular stomatitis virus-based vaccines protect nonhuman primates against aerosol challenge with Ebola and Marburg viruses. Vaccine 26: 6894- 6900.
- Qiu X, Fernando L, Alimonti JB, Melito PL, Feldmann F, et al. (2009) Mucosal immunization of cynomolgus macaques with the VSVDeltaG/ZEBOVGP vaccine stimulates strong ebola GP-specific immune responses. PLoS One 4: e5547.
- Daddario-DiCaprio KM, Geisbert TW, Geisbert JB, Stroher U, Hensley LE, et al. (2006) Cross-protection against Marburg virus strains by using a live, attenuated recombinant vaccine. J Virol 80: 9659-9666.
- Geisbert TW, Geisbert JB, Leung A, Daddario-DiCaprio KM, Hensley LE, et al. (2009) Single-injection vaccine protects nonhuman primates against infection with marburg virus and three species of ebola virus. J Virol 83: 7296-7304.
- Falzarano D, Feldmann F, Grolla A, Leung A, Ebihara H, et al. (2011) Single immunization with a monovalent VSV-based vaccine protects nonhuman primates against heterologous challenge with Bundibugyo ebolavirus. J Infect Dis.3:S1082-9.
- Hensley LE, Mulangu S, Asiedu C, Johnson J, Honko AN, et al. (2010) Demonstration of cross-protective vaccine immunity against an emerging pathogenic Ebolavirus Species. PLoS Pathog 6: e1000904.
- Geisbert TW, Daddario-Dicaprio KM, Lewis MG, Geisbert JB, Grolla A, et al. (2008) Vesicular stomatitis virus-based ebola vaccine is well-tolerated and protects immunocompromised nonhuman primates. PLoS Pathog 4: e1000225.
- Daddario-DiCaprio KM, Geisbert TW, Stroher U, Geisbert JB, Grolla A, et al. (2006) Postexposure protection against Marburg haemorrhagic fever with recombinant vesicular stomatitis virus vectors in non-human primates: an efficacy assessment. Lancet 367: 1399-1404.
- Geisbert TW, Hensley LE, Geisbert JB, Leung A, Johnson JC, et al. (2010) Postexposure treatment of Marburg virus infection. Emerg Infect Dis 16: 1119- 1122.
- Geisbert TW, Daddario-DiCaprio KM, Williams KJ, Geisbert JB, Leung A, et al. (2008) Recombinant vesicular stomatitis virus vector mediates postexposure protection against Sudan Ebola hemorrhagic fever in nonhuman primates. J Virol 82: 5664-5668.
- Geisbert TW, Daddario-DiCaprio KM, Geisbert JB, Young HA, Formenty P, et al. (2007) Marburg virus Angola infection of rhesus macaques: Pathogenesis and treatment with recombinant nematode anticoagulant protein c2. J Infect Dis 196 : S372-381.
- Takada A, Ebihara H, Jones S, Feldmann H, Kawaoka Y (2007) Protective efficacy of neutralizing antibodies against Ebola virus infection. Vaccine 25: 993-999.
- Wilson JA, Hevey M, Bakken R, Guest S, Bray M, et al. (2000) Epitopes involved in antibody-mediated protection from Ebola virus. Science 287: 1664- 1666.
- Parren PW, Geisbert TW, Maruyama T, Jahrling PB, Burton DR (2002) Preand postexposure prophylaxis of Ebola virus infection in an animal model by passive transfer of a neutralizing human antibody. J Virol 76: 6408-6412.
- Tuffs A (2009) Experimental vaccine may have saved Hamburg scientist from Ebola fever. BMJ 338: b1223.
- Griffin DE, Pan CH, Moss WJ (2008) Measles vaccines. Front Biosci 13: 1352- 1370.
- De Vries RD, Stittelaar KJ, Osterhaus AD, de Swart RL (2008) Measles vaccination: new strategies and formulations. Expert Rev Vaccines 7: 1215- 1223.
Relevant Topics
- Anthrax Bioterrorism
- Bio surveilliance
- Biodefense
- Biohazards
- Biological Preparedness
- Biological Warfare
- Biological weapons
- Biorisk
- Bioterrorism
- Bioterrorism Agents
- Biothreat Agents
- Disease surveillance
- Emerging infectious disease
- Epidemiology of Breast Cancer
- Information Security
- Mass Prophylaxis
- Nuclear Terrorism
- Probabilistic risk assessment
- United States biological defense program
- Vaccines
Recommended Journals
Article Tools
Article Usage
- Total views: 18243
- [From(publication date):
specialissue-2011 - Dec 05, 2025] - Breakdown by view type
- HTML page views : 13209
- PDF downloads : 5034