Prostate Cancer in the Pre and Post Diagnosis Phase – A Population Based Study on Health Care Costs
Received: 10-Nov-2011 / Accepted Date: 30-Nov-2011 / Published Date: 15-Dec-2011 DOI: 10.4172/2161-1165.S1-001
Abstract
Prostate cancer is associated with significant health care costs and is a major public health concern. The aim of this study was to examine and analyse all direct health care costs among prostate cancer in the pre- and post diagnostic phase of the disease. The aim was also to examine if outcomes of ill health in terms of health care use and health care costs increased among partners of prostate cancer patients. We used population-based data for monitoring health care costs, including in- and outpatient care and pharmaceuticals. Health care costs were monitored in relation to time periods before and after the prostate cancer diagnosis for both patients and their partners. The major part of health care costs for prostate cancer patients occurred during the first year following the diagnosis. A clear difference was seen between costs for survivors and costs for deceased; the first year following the diagnosis costs was about 50% higher for deceased and 2-3 times higher the following years. Health care costs increased with higher Gleason score in the year following the diagnosis. Higher health care costs were seen for patients treated with primary radiotherapy. Lowest costs were seen for patients with expectancy. Health care costs were higher for patients with curative treatments compared to those with palliative treatments. Partners had an increase in health care use both the first and second year following the diagnosis of the prostate cancer patient leading to an increase in health care costs. The cost burden of prostate cancer varies along the different phases of the disease. When planning for care and allocation of resources for care the impact on the partner should also be considered.
Introduction
Prostate cancer is globally the second most common malignancy in men. In Sweden it is the most frequently diagnosed cancer [1,2]. The incidence is increasing, mainly because of an older population and the possibilities for earlier detection of the disease. Furthermore, a great number of patients live for a considerable time following the diagnosis as the disease often progresses slowly. Despite declining mortality rates, costs are thus expected to further raise in the future [3].
Previous studies have shown that the cost burden of prostate cancer is high and varies according to treatment type. Costs are highest for patients treated with external-beam therapy and lowest for patients treated with watchful waiting [4]. However, several aspects concerning the costs of prostate cancer have not yet been fully evaluated. To date, limited information exists regarding health care costs for prostate cancer patients in the pre-diagnostic phase of the disease. Knowledge about costs in the last year of life for prostate cancer patients is also sparse; as such studies usually are conducted at an institutional level [3]. Only one population-based study was found that focused on different phases of the disease. Results showed that costs are highest around two events, the cancer diagnosis and cancer death [5].
Another perspective of prostate cancer related costs not yet fully investigated are the costs for the influence on relatives, for example the partner. In a recent study we found that partners of prostate cancer patients had a significant increase in psychiatric diagnoses and in gastro-intestinal diseases. They also had a significant increase in health care use [6]. Thus, the increase of health care costs for partners should be taken into consideration when assessing the burden of costs for prostate cancer.
The aim of this study was to examine and analyse all direct health care costs among prostate cancer in the pre- and post diagnostic phase of the disease. The aim was also to examine if outcomes of ill health in terms of health care use and health care costs increased among partners of prostate cancer patients.
Materials and Methods
The study presents data for the population in Region Skåne, the southernmost health care region in Sweden. All persons diagnosed with prostate cancer in the period 2000 to 2005 were identified via the Cancer Register of Southern Sweden. Individual data were linked via the ten-digit personal identification number to the Population Register of Sweden, Regional Health Care registries including primary care, and National Health Care registries also including prescribed pharmaceuticals. Data on Gleason score, and treatment types were obtained from the Prostate Cancer Register. The Prostate Cancer Register is a regional as well as national register used for quality followups and quality improvements of the prostate cancer care. Partners to the prostate cancer patients were identified via Population Register of Sweden when living at the same address at the time of the cancer diagnosis.
For each individual, healthcare costs were monitored related to the date of diagnosis. Using this method we calculated the costs for different time periods before and after diagnosis and proximity to death. Costs were obtained for each individual in Region Skåne for all in- and outpatient contacts and pharmaceuticals prescribed for both cancer care and all other care. University hospitals in Region Skåne use advanced models with Activity-Based Costing (ABC) methodology for all the different health-care services provided to individual patients. To decide the costs per patient for health-care in other hospitals in Region Skåne, we used each hospitals own cost per Diagnosis-Related Group (DRG) per clinic matched to the individual patient’s DRG. For primary care we used the average cost per visit to each clinic. Data on health care costs was matched with data on Gleason score and treatment type from the Prostate Cancer Register. Pharmaceutical costs prescribed in outpatient care were monitored for the year following the prostate cancer diagnosis. These costs were based on the part of the study population diagnosed with prostate cancer in the second half of 2005.
Comparisons of health care costs for the whole study period were made with the standard population in the Southern Health Care Region matched for age and gender and with breast cancer patients in Region Skåne. All costs are presented in Euros (rates on 2011-11-01, EUR-SEK 9.0).
Partners’ health care costs were obtained in the same way as described above with in- and outpatients’ costs. They were monitored related to the date of diagnosis of the prostate cancer patient. Health care costs were compared to those of the general population, matched for age, gender and marital status.
This study is part of a larger study of cancer diseases in the Southern Health Care Region. The study was approved by Lund University Committee for Research and Ethics (dnr 80/2007). Handling and storage of data were processed according to Swedish law (Personuppgiftslagen, PUL 1998:2004). All data were coded and thus anonymous in all gathering and handling of data.
Results
Study population
The average yearly incidence of prostate cancer was 218 per 100,000 for the period 2000-2005 in Region Skåne, and was in accordance with national figures for Sweden for the same period [2]. The number of cases stratified by age is shown in Table 1. This gave a study sample of 7 319 prostate cancer patients, of which 66% had a spouse. The study population of partners consisted of 4,860 spouses; 54% of them were older than 65 years and 99.9% were female partners. Distribution of prostate cancer patients according to Gleason score registered in the Prostate Cancer Register is shown in Table 2 (n=7 209).
| Year | Health expenditure as percentage of GDP |
| 2005 | 3.55 |
| 2006 | 3.73 |
| 2007 | 3.75 |
| 2008 | 3.08 |
| 2009 | 4.10 |
| 2010 | 3.01 |
| 2011 | 3.69 |
| 2012 | 3.21 |
| 2013 | 3.10 |
Table 1: Health expenditure in Saudi Arabia as percentage of the GDP.
| Variable | Mean ± SE | Frequency | Percentage |
| Age | 22.06 ±0.07 | ||
| 18-21 | 1307 | 51.9 | |
| 22-25 | 876 | 34.8 | |
| 26-29 | ` | 258 | 10.2 |
| ≥30 | 77 | 3.1 | |
| Residence Region | |||
| Central | 858 | 34.1 | |
| Western | 722 | 28.7 | |
| Southern | 516 | 20.5 | |
| Eastern | 299 | 11.9 | |
| Northern | 123 | 4.9 |
Table 2: Descriptive statistics for the demographical variables (n=2518)
One year survival for all diagnosed with prostate cancer was 93.7%, and the five year survival was 68.2% (Table 3). Prostate cancer patients with a partner had marginal better survival rates, with one year survival 94.6% and five year survival 70.1%.
| Blood Type | Frequency | Percentage | Percentage previous Studies*[24,26] |
| O+ | 1197 | 47.5 | 48 |
| O- | 106 | 4.2 | 4 |
| A+ | 643 | 25.5 | 24 |
| A- | 66 | 2.6 | 2 |
| B+ | 386 | 15.3 | 17 |
| B- | 24 | 1.0 | 1 |
| AB+ | 93 | 3.7 | 4 |
| AB- | 3 | 0.1 | 0.3 |
Table 3: Results of blood type test of the participants.
Health care costs related to prostate cancer
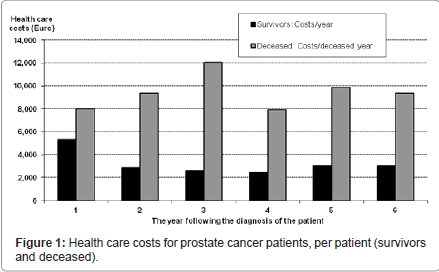
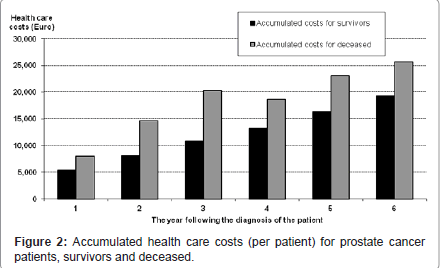
Health care costs per person and year are shown in Table 4, showing that the major part of costs for the prostate cancer patients occur during the first year following the diagnosis. When comparing survivors with those deceased, costs decreased for survivors and increased for deceased with a peak during the third year post diagnosis (Figure 1). Accumulated costs for survivors and deceased are shown in Figure 2, showing higher health care costs per person for deceased.
| Test | Result | Frequency | Percent |
| Right Eye Test | Fit | 2466 | 97.9 |
| Unfit | 52 | 2.1 | |
| Left Eye Test | Fit | 2475 | 98.3 |
| Unfit | 43 | 1.7 | |
| Colour Blindness | Negative | 2437 | 96.8 |
| Positive | 81 | 3.2 | |
| Eyes’ Lids | Fit | 2516 | 99.9 |
| Unfit | 2 | 0.1 | |
| Overall Eyes Assessment | Fit | 2382 | 94.6 |
| Unfit | 136 | 5.4 | |
| Overall E.N.T Assessment | Fit | 2518 | 100 |
| Unfit | 0 | 0 | |
| Overall Dentist Assessment | Fit | 2517 | 100 |
| Unfit | 1 | ≈ 0 | |
| Overall Psychological Assessment | Fit | 2517 | 100 |
| Unfit | 1 | ≈ 0 | |
| Overall Radiology Assessment | Fit | 2517 | 100 |
| Unfit | 1 | ≈ 0 | |
| Overall Surgical Assessment | Fit | 2501 | 99.3 |
| Unfit | 17 | 0.7 | |
| Lung Diseases | Negative | 2517 | 100 |
| Positive | 1 | ≈ 0 | |
| Heart Diseases | Negative | 2517 | 100 |
| Positive | 1 | ≈ 0 | |
| Overall Internist Assessment | Fit | 2517 | 100 |
| Unfit | 1 | ≈ 0 | |
| Sickle Cell Test (Trait and Disease) | Negative | 2400 | 95.3 |
| Positive | 118 | 4.7 | |
| Hepatitis A | Negative | 2518 | 100 |
| Positive | 0 | 0 | |
| Hepatitis B | Negative | 2502 | 99.4 |
| Positive | 16 | 0.6 | |
| Hepatitis C | Negative | 2518 | 100 |
| Positive | 0 | 0 | |
| Hepatitis D | Negative | 2518 | 100 |
| Positive | 0 | 0 | |
| Hepatitis E | Negative | 2518 | 100 |
| Positive | 0 | 0 | |
| Drug Test | Negative | 2448 | 97.2 |
| Positive | 70 | 2.8 |
Table 4: Results of the participants screening process.
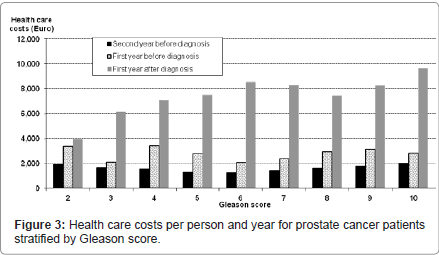
When stratifying health care costs in relation to Gleason score (Figure 3), an increase in health care costs per person and year was seen. No differences were seen for health care costs in the years before the prostate cancer diagnosis. In the year following the diagnosis health care costs increased with higher Gleason score, from Gleason 3 and higher.
Health care costs for prostate cancer patients with different treatment types stratified by accumulated Gleason groups are shown in Table 3. Highest costs were seen for patients treated with external radiotherapy. Lowest costs were seen for patients with expectancy as treatment. Health care costs were higher for patients with curative treatments compared to those with palliative treatments (Table 5).
| Cross Tabulation | P-value* | OR‡ | |||
| Region of Residence | Sickle Cell Test | ||||
| Negative | Positive | ||||
| Centre | 840 | 18 (2.1%) | <0.001 | Reference | |
| West | 710 | 12 (1.6%) | 0.79 (0.38, 1.65) | ||
| South | 460 | 56 (10.9%) | 5.68 (3.30, 9.80)* | ||
| East | 269 | 30 (10%) | 5.20 (2.86, 9.49)* | ||
| North | 121 | 2 (1.6%) | 0.77 (0.18, 3.37) | ||
| Region of Residence | Left-Eye test | ||||
| Normal | Not Normal | ||||
| Centre | 849 | 9 | <0.048 | Reference | |
| West | 712 | 10 | 1.32 (0.54, 3.28) | ||
| South | 500 | 16 | 3.02 (1.32, 6.88)* | ||
| East | 292 | 7 | 2.26 (0.83, 6.13) | ||
| North | 122 | 1 | 0.77 (0.10, 6.15) | ||
| * Statistically significant (p-value <0.05) ‡OR: Odds Ratio | |||||
Table 5: Medical conditions associated with regions of residence.
Pharmaceutical costs prescribed in outpatient care were observed to be 1,405 Euro per person and year (the year following the prostate cancer diagnosis), of which 51% accounted for endocrine therapy (715 Euro).
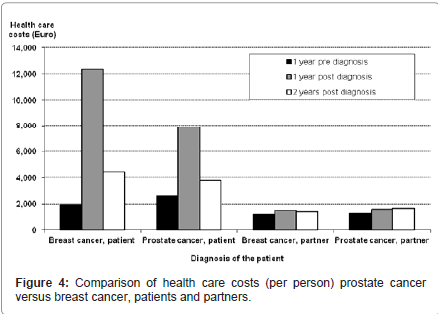
When comparing health care costs for prostate cancer patients with those for breast cancer patients, costs per breast cancer patient were 50% higher during the first year post diagnosis. The following years post diagnosis costs were essentially the same (Figure 4). Differences and similarities between costs for breast and prostate cancer patients were the same for both survivors and deceased.
Health care costs for partners of prostate cancer patients
A significant increase in inpatient care was seen for partners both the first and second year following the diagnosis of the prostate cancer patient. Compared to the year before the diagnosis the number of hospital stays increased with 16%, and days in hospital increased 32% the first year and another 76% the second year after the diagnosis. No increase was seen for outpatient care. The increase in health care use led to increased health care costs for partners both the first and second year post diagnosis compared to costs the year pre diagnosis. In comparison with partners to breast cancer patients, health care costs were essentially the same (Figure 3). Increases were significant compared to costs for the general population, matched for gender, age and marital status. Younger partners (25-64 years old) had a larger increase than older partners (> 65 years).
Discussion
Few studies have used a population-based approach and healthcare consumption, outcome and costs on an individual level have seldom been studied [7]. Findings from this study provide additional information about all direct health care costs related to prostate cancer in different phases of the disease including the pre diagnosis phase and the last year of life for those deceased. Costs related to the prostate cancer diagnosis in the pre diagnosis phase are probably explained by the delay in registration of the diagnosis, which is often done some weeks after the actual time of diagnosis. Findings from this study about costs in different phases of the disease are in accordance with previous research, showing that the two events with highest costs are the time of the diagnosis and the final year [5]. Our data was monitored for a population diagnosed in 2000-2005, giving a picture of costs before the new medical treatment options for prostate cancer was available in full clinical practice. For future studies this might serve as an important base for comparisons. Our data, therefore, provide a baseline for further studies of the effects of the new targeted therapy. One important question for the future is how to prioritize limited resources and how to move resources from treatment to prevention [8-10].
Health care costs for survivors decreased with time from diagnosis, and costs related to the prostate cancer diagnosis also decreased. This is concomitant to previous prevalence based research on health care costs for prostate cancer, showing progressively lower costs the second and third year following the diagnosis [11]. However, future studies need to focus the impact on costs that new treatment options might have had.
When comparing costs for prostate cancer with costs for breast cancer, a clear difference was seen in the first year following the diagnosis with higher costs for breast cancer. As breast cancer treatment is more intense during the first year this was not unexpected. However, the following year’s costs became more equal.
Partners to prostate cancer patients might be affected by their own health with an increased health care use as a consequence. This should be considered when calculating the cost burden of prostate cancer. The partner can be of great importance for the cancer patient in providing both practical and emotional support. Our results also suggest that survival rates are improved for those living with a partner compared to those living alone, which is supported in previous research showing that excess mortality for never married compared to married has increased steadily. This is especially seen for men [12]. Altogether it implies the importance of having a partner or another relative/friend when following a cancer therapy regimen. It also emphasizes the necessity of including the partner in both planning and calculating for prostate cancer care.
Methodological considerations to be made in this study might be the limitation that data does not include costs for municipal care. With the ageing trend in the population and thereby increasing number of elderly with prostate cancer, it is important to also consider those data in future studies. The results give new knowledge about total health care costs related to different treatment types, but do not tell the actual treatment costs. Another limitation might be that we did not adjust for time at risk for the deceased when stratifying health care costs by Gleason score, leading to a probable underestimation of health care costs for patients with higher Gleason score.
Prostate cancer is an important issue in terms of health care decisions. In this study we have elucidated different perspectives of significance when calculating costs for prostate cancer. In future research this also needs to be considered, as costs of prostate cancer are likely to increase.
Acknowledgements
This study was conducted with support from the Southern Regional Care Committee in Sweden.
References
- Ferlay J, Autier P, Boniol M, Heanue M, Colombet M, et al. (2007) Estimates of the cancer incidence and mortality in Europe in 2006. Ann Oncol 18: 581-592.
- The National Board of Health and Welfare (2008) Cancer Incidence in Sweden 2007. Health and diseases 11: 1-117.
- Roehrborn CG, Black LK (2011) The economic burden of prostate cancer. BJU Int 108: 806-813.
- Molinier L, Castelli C, Bauvin E, Rebillard X, Souli M, et al. (2011) Cost study of the clinical management of prostate cancer in France: results on the basis of population-based data. Eur J Health Econ 12: 363-371.
- Krahn MD, Zagorski B, Laporte A, Alibhai SM, Bremner KE, et al. (2010) Healthcare costs associated with prostate cancer: estimates from a population-based study. BJU Int 105: 338-346.
- Sjvall K, Attner B, Lithman T, Noreen D, Gunnars B, et al. (2009) Influence on the health of the partner affected by tumor disease in the wife or husband based on a population-based register study of cancer in Sweden. J Clin Oncol 27: 4781-4786.
- Molinier L, Bauvin E, Combescure C, Castelli C, Rebillard X, et al. (2008) Methodological considerations in cost of prostate cancer studies: a systematic review. Value Health 11:878-885.
- Smith BD, Smith GL, Hurria A, Hortobagyi GN, Buchholz TA (2009) Future of cancer incidence in the United States: burdens upon an aging, changing nation. J Clin Oncol 27: 2758-2765.
- Bray F, Mller B (2006) Predicting the future burden of cancer. Nat Rev Cancer 6: 63-74.
- Bosanquet N, Sikora K (2004) The economics of cancer care in the UK. Lancet Oncol 5: 568-574.
- Norlund A, Alvegrd T, Lithman T, Merlo J, Noreen D (2003) Prostate cancer--prevalence-based healthcare costs. Scand J Urol Nephrol 37: 371-375.
- Kravdal H, Syse A (2011) Changes over time in the effect of marital status on cancer survival. BMC Public Health 11: 804.
Citation: Sjövall K, Attner B, Lithman T, Noreen D, Olsson H (2011) Prostate Cancer in the Pre and Post Diagnosis Phase – A Population Based Study on Health Care Costs. Epidemiol S1:001. DOI: 10.4172/2161-1165.S1-001
Copyright: © 2011 Sjövall K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 14986
- [From(publication date): 11-2011 - Dec 05, 2025]
- Breakdown by view type
- HTML page views: 10243
- PDF downloads: 4743