Short Communication Open Access
Reconstruction of Lateral Ankle Ligaments Update
Slater GL1*, Walters EE2 and O’Malley M31Sports Foot and Ankle Surgery, Edgecliff Sydney, Australia
2The University of Texas Medical School at Houston, Houston, USA
3Hospital for Special Surgery, Department of Foot and Ankle Surgery, USA
All Authors Contributed Equally
- *Corresponding Author:
- Slater GL
Sports Foot and Ankle Surgery, Australia
Tel: +61-1300388778
Fax: +61-60409555
E-mail: gslater@jakll.com.au
Received date: January 04, 2016; Accepted date: January 25, 2016; Published date: February 27, 2016
Citation: Slater GL, Walters EE, O’Malley M (2016) Reconstruction of Lateral Ankle Ligaments Update. J Ost Arth 1:109. doi: 10.4172/joas.1000109
Copyright: © 2016 Slater GL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Osteoarthritis
Abstract
The emergence of minimally invasive techniques for the reconstruction of lateral ankle ligaments has generated procedures that allow for the restoration of joint anatomy and kinematics while also limiting adverse post-surgical sequelae. Moreover, such advances have paved the way for the use of arthroscopy as a diagnostic tool, allowing for early identification and management of associated lesions and/or underlying pathologies. Our technique, which combines an arthroscopic approach with a direct anatomic reconstruction, has improved the diagnosis and management of intra-articular lesions. Moreover, it has facilitated the use of other minimally invasive techniques in conjunction with ligamentous repair, allowing for quicker post-operative recovery and better surgical outcomes. Both the literature review and our experience suggest that positive and long-lasting outcomes can be achieved through employment of our technique.
Keywords
Chronic ankle instability; Anatomic ligament reconstruction; Lateral ankle ligament; Modified brostrom; Arthroscopy
Introduction
Lateral ligament insufficiency secondary to ankle sprain is one of the most frequently encountered musculoskeletal injuries. Such an insult typically occurs following a combined inversion-plantar flexion injury of the foot, which often leads to disruption of the lateral ligamentous complex [1]. While most fully recover, up to 20% of patients experience long-lasting symptoms following the initial event, such as stiffness, ligament laxity, weakness, and recurrent sprains– all of which pave the way for chronic ankle instability [2-6]. Left unaddressed, lack of joint stability can initiate a cascade of undesirable complications, such as chronic pain, synovitis, chondral damage, and osteoarthritis [7,8]. Treatment with conservative modalities, such as functional rehabilitation, muscle strengthening, and proprioceptive training, is often successful, particularly in cases of functional instability alone (subjective feeling of one’s ankle “giving out”) [9]. For patients that develop chronic instability and fail to achieve satisfactory outcomes with a conservative treatment regimen, surgical intervention is often indicated.
Anatomically, chronic lateral ankle instability is often due to compromise of the anterior joint capsule and the anterior talofibular ligament (ATFL), with additional insufficiency of the calcaneofibular ligament (CFL) in about 15%-30% of patients [4,10-12]. Ligamentous repair of the lateral ankle is typically classified as non-anatomic or anatomic. While non-anatomic procedures usually achieve successful reconstruction outcomes, these techniques have been linked to abundance of undesirable post-surgical complications; as such, anatomic reconstruction, in particular the modified Brostrom-Gould method is considered by many orthopedic surgeons to be the superior reconstructive technique for repair of the aforementioned ligaments. Yet while the modified Brostrom has proven both reliable and highly effective, clinical studies show that anywhere from 13% to 35% of patients experience residual symptoms following successful anatomic reconstruction as a result of unaddressed intra-articular lesions [4,13,14].
This updated review focuses on our technique, which after 20 years of implementation has proven biomechanical equivalency, if not superiority, to the direct Brostrom-Gould procedure [2]. We also outline our surgical technique for additional procedures that are often performed in conjunction with lateral ligament repair, including tibia/ filbula stabilization, Jones fracture repair, and cavus foot correction. Additionally, we discuss our general model of patient assessment as it pertains to diagnostic evaluation and treatment of concomitant pathologies, including osteochondral lesions and soft tissue impingement.
Risk Factors
Recent studies have implicated several factors that may predispose and/or contribute to ankle instability and inversion injuries. Modifiable risk factors include weight/BMI, footwear, muscle strength, and activity level [10,15]. Non-modifiable predispositions include foot/ ankle anatomy, extremity alignment, previous ankle sprain, generalized joint laxity, and underlying intra-articular pathologies. Notably, bony malalignments, such as hindfoot varus, first ray plantarflexion, and midfoot cavus, can predispose to chronic instability [5,10]. While these non-modifiable risk factors remain unchangeable from a patient perspective, it is vital that they are considered when composing surgical strategy. Failure to address the coexistence of additional issues can result in post-surgical complications, including instability, stiffness, and pain, as well as early operative failure despite a successful ligament reconstruction [9,16,17].
Diagnosis and Work-up
It is vital that the initial patient assessment and workup includes a thorough clinical history, detailed physical exam, and imaging studies when appropriate. We respectfully submit that examination of chronic ankle instability should always include an anterior drawer test and an inversion test, as well as evaluation of peroneal tendon integrity/ strength, heel alignment, and ankle range of motion. Diagnosis is made when there is increased laxity on anterior drawer and inversion testing compared to the contralateral ankle [5].
Current opinion regarding imaging for lateral ankle sprain evaluation is a topic of debate. Based on our clinical experience, we recommend always obtaining radiographs (antero-posterior and lateral) and an MRI; weight-bearing images are recommended if possible. Magnetic resonance imaging (MRI) is a useful diagnostic tool for the evaluation of chronic ankle discomfort, especially when attempting to identify associated injuries such as osteochondral lesions or peroneal pathology [5]. Stress radiographs (including talar tilt and anterior drawer tests) may be useful in evaluating ligamentous laxity in patients with chronic ankle instability, but are not recommended in the acute setting [10].
On a case-to-case basis, CT scans may contribute to the clinical picture, particularly when fractures and/or bony mal-alignments are suspected. A thorough clinical history and detailed physical exam play a crucial role in the work up of chronic ankle instability, as early identification and correction of any concurrent/pre-existing intra-articular pathologies will influence patient outcomes.
Surgical Options- Update
As previously discussed, a variety of methods are employed in the operative treatment of lateral ligamentous injuries. While the majority of these methods achieve successful ligament repair, non-anatomic techniques (such as the Watson-Jones and Chrisman Snook procedures) result in altered biomechanics of the subtalar joint, producing disappointing functional results in two-thirds of patients [3,18,19]. Non-anatomic repairs are typically tenodesis procedures, which require rerouting a slip of harvested tendon (usually one of the peroneal tendons) to impart stability [5]. The peroneal tendons serve an important role in normal ankle function, as they are dynamic stabilizers of the hindfoot and help to maintain the longitudinal arch. Their use as a graft destabilizes the ankle and causes alteration in ankle/hindfoot kinematics with resultant loss of subtalar motion [11]. Moreover, non-anatomic techniques are associated with increased pain, limited range of motion, increased need for revision procedure, stiffness, loss of strength due to peroneal tendon sacrifice, and increased incidence of osteoarthritis [10,20].
In our experience, results of such procedures are varied, with 85-95% producing good or excellent reconstructive results. However, due to such undesirable post-surgical sequelae in the long term, use of these techniques should be reserved for patients who demonstrate hypermobility, nerve injuries, or cases of failed anatomic repair [5,21].
Anatomically direct operative techniques repair the ATFL and CFL while simultaneously restoring hindfoot kinematics. “Such repair was initially described by Brostrom and later by Gould and Karlsson et al.” [9]. The Gould modification of the Brostrom method reinforces the ligamentous repair by securing the inferior extensor retinaculum to the distal fibula, providing additional support against inversion load and stabilizing the subtalar joint [10,22]. Unlike tenodesis procedures, direct anatomical techniques have the advantage of smaller incisions, resulting in better cosmetic results and less pain [9]. Although proven to yield good outcomes, anatomic methods only consider the ligamentous structures, failing to address any intra-articular lesions or underlying pathologic abnormalities.
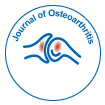
As previously mentioned, our preferred method employs an arthroscopic exam in conjunction with a minimally invasive delayed lateral ligamentous reconstruction. We have successfully employed this minimally invasive method for over 20 years, and find that it provides optimal short- and long-term patient outcomes. Slater et al. reported post-surgical outcomes of 233 patients that underwent lateral ligament repair using our surgical technique between 1998-2008 in the largest single-surgeon study to date, to our knowledge. Inclusion criteria included symptomatic instability that did not improve with conservative treatment, more than three instances of significant instability, and positive clinical exam findings. Those with varus heel alignment or peroneal weakness due to a neurological condition were excluded. The overall patient satisfaction rate was 91%; moreover, the majority of subjects denied continued instability, as 78% returned to activities without recurrence of inversion injuries (Figure 1) [5].
Of the remaining, 13% returned to pre-injury activity levels with some residual instability, while 9% were limited in their ability to return to activity. Of those that did not return to pre-injury function, a large percentage had another surgery performed in addition to the modified Brostrom, such as fracture repair. Post-operatively, 97.75% of patients remained pain free; of the remaining 2.25% of patients who described experiencing an intermittent “achey” pain, two patients had underlying fractures and underwent internal fixation in conjunction with the modified Brostrom procedure. These additional underlying circumstances may have affected the results, contributing to residual instability and post-surgical pain in these individuals [5].
Arthroscopy
In our experience, utilization of arthroscopy prior to ligament reconstruction provides numerous advantages. It enables the surgeon to decide which ligaments are injured and to what extent, visually assess ligament integrity, and determine if there are any associated injuries [15]. In essence, arthroscopy is the best way to detect an unstable syndesmosis. Numerous studies have demonstrated abnormal intra-articular findings upon arthroscopic assessment of the chronically unstable ankle [8,23], Recently, Nery et al. demonstrated that in a group of 38 patients undergoing lateral ankle ligament reconstruction, arthroscopic examination completely confirmed the pre-operative MRI diagnosis in 71% of patients, with only partial confirmation of the initial diagnosis in 29% of patients [4]. White et al. identified that in three of the four cases with an osteochondral lesion (OCL), there was no radiological evidence of it [13]. In other words, the underlying injury likely would have gone undetected had arthroscopy not been performed. Findings of a study conducted by Cha et al. indicate that MRI sensitivity is relatively low for the diagnosis of intra-articular lesions [24]. To ensure that co-existing abnormalities don’t go undetected and untreated, it is imperative that arthroscopic evaluation is performed prior to proceeding with the ligamentous reconstruction.
Commonly Associated Injuries
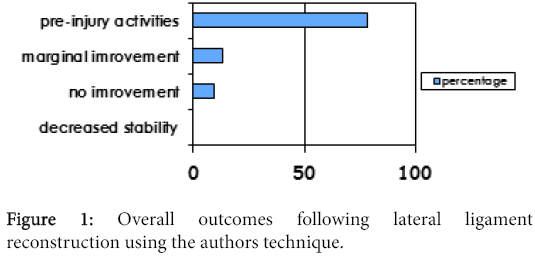
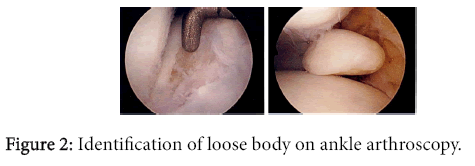
Proper diagnosis and treatment of associated concomitant pathology is integral, and must be addressed in order to achieve satisfactory results for the patient [5]. Hinterman et al. [10] demonstrated that in patients undergoing lateral ligamentous repair, the incidence of co-existing intra-articular synovitis was 32% and chondral lesions was 55% [6,23]. A similar study conducted by Hua et al. revealed that 90.8% of patients undergoing the modified Brostrom procedure were found to have accompanying intra-articular lesions on arthoscopic examination (Figures 2 and 3). Out of 87 ankles, 86.2% had synovitis/soft tissue impingement, 37.9% had a chondral injury, and 6.9% had a distal tibiofibular syndesmosis injury [14]. Neglected distal tibiofibular syndesmosis has been proven to delay rehabilitation and cause prolonged ankle dysfunction [13].
Talar osteochondral lesions have been considered the strongest indicator of poor outcomes following surgery, and are highly associated with chronic post-operative pain [4,16,17]. Up to 50% of lateral ligament sprains may have associated osteochondral lesions (OCLs), particularly after sporting injuries. Van Dijk et al. identified 20 OCLs in 30 ankles that underwent arthoscropy prior to lateral ligament repair [13]. Special attention must be paid to address and correct any associated structural abnormalities that can increase supination forces through the lateral ankle. When uncorrected, such underlying bony malalignments result in a higher stress load being placed on reconstructed ligaments, and may result in laxity recurrence [9].
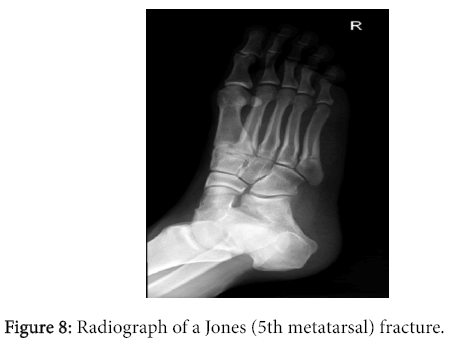
Lastly, a fracture of the fifth metatarsal, known as a Jones fracture, is commonly associated with ankle inversion injuries. This type of fracture is usually the result of ankle plantarflexion and forefoot adduction; consequently, excessive force is placed on the lateral forefoot and metatarsal heads [11,25]. Our preferred repair technique for this injury is discussed below.
Acute vs Delayed Repair
Most orthopedic surgeons recommend a 3-6 month regimen of nonoperative treatment prior to considering surgical intervention [10]. Specifically, we reserve delayed reconstruction of the lateral ligamentous complex for patients who experience significant functional and mechanical instability despite undergoing atleast 3 months of physiotherapy and muscle strengthening.
However, early lateral ligament reconstruction may be warranted in select acute cases demonstrating tibia/fibula instability, ruptured peroneal tendons, and/or large osteochondral lesions. Early reconstruction of acute cases may also be considered in athletes, as residual instability has been shown to be a predictor of repeated injury [13]. In an attempt to reduce the risk of later complications and expedite return to sports, lateral ligament reconstruction may be a time-efficient and effective option for competitive athletes [26].
Our Surgical Technique- Update
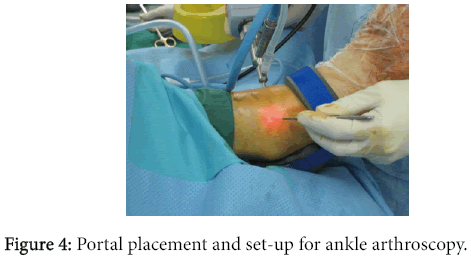
Surgery is carried out under anesthesia with tourniquet control, and arthroscopy is performed prior to the reconstruction (Figure 4). Using a 2.7 mm 30° angle arthroscope, arthroscopic evaluation is used to inspect the ankle joint and syndesmosis, as well as to evaluate for any articular or intra-articular injuries. Any identified intra-articular lesions are assessed and managed accordingly, with tendoscopy and tendon debridement via introduction of a posterolateral portal for peroneal injury; debridement for chondral injuries; or removal of loose bodies.
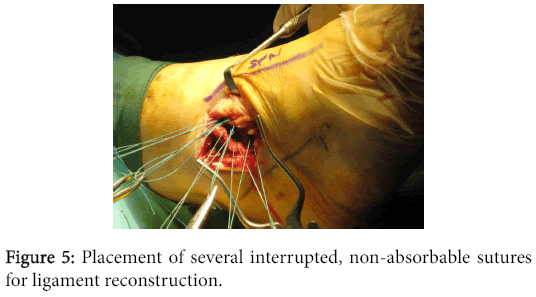
The modified Brostrom is performed following arthroscopy. Incision style (longitudinal, transverse, or oblique) is based on other pathology and ensures exposure of the necessary structures, including the lateral ligamentous complex, inferior retinaculum, and, in some cases, the peroneal tendons. The surgeon should next dissect through the subcutaneous tissue, taking care to avoid branches of the superficial peroneal nerve and the sural nerve. Following identification of the anterior joint capsule, ATFL, and CFL, the inferior retinaculum should be mobilized and retracted, as outlined by the Gould modification. After carefully dissecting at the level of the CFL, the anterior joint capsule should be incised longitudinally, with a portion of the capsule left attached to the fibula for later repair. Reconstruction is initiated using 1/10 ethibond sutures, placing several interrupted, nonabsorbable sutures in the capsule, AFTL, and CFL (Figure 5). Sequential imbrication of the joint capsule is then performed from inferior to superior. Sutures are to be tied with the foot in an everted position. Next, the inferior extensor retinaculum is mobilized and advanced over the imbricated repair. This is secured to the fibula via a continuous 3/0 undyed suture, and the skin is held in place with 4/0 vicryl. Closing technique includes a layered closure, followed by placement of a soft dressing [5].
Post-operative protocol dictates that an air-cast boot is to be placed on the foot and worn until a 10 days post-operative appointment. Following this appointment, the boot should be work for another two to four weeks to allow adequate healing. A physiotherapy regimen should be initiated and will last for 4-6 weeks.
Additional Procedures
When other lesions are identified, additional operative procedures can often be performed in conjunction with the modified Brostrom.
Tibia/Fibula Stabilization
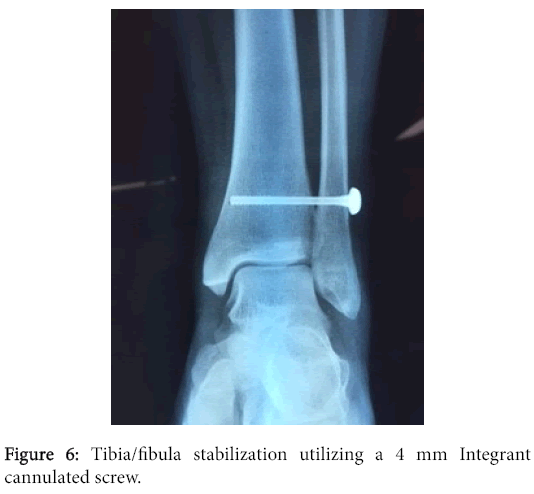
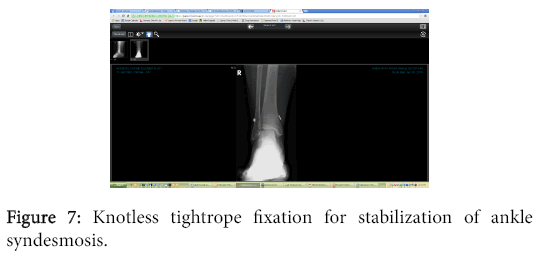
The ankle is placed into neutral position and a wire is introduced from the fibula to the tibia. The tibiofibular joint is initially stabilized using a 50 mm × 4 mm Integrant screw (Figure 6). Fluoroscopy should be used throughout to ensure correct positioning of the screw. After 4 weeks, a knotless tightrope device at 9/5v may be substituted for an Integrated screw to allow for early rehabilitation (Figure 7). The Integrant screw provides compression, which is ideal early on, whereas the tightrope provides long-term stability.
Jones Fracture Repair
The patient should be placed in the lateral decubitis position with tourniquet control. Next, the foot is exsanguinated, followed by standard prepping and draping. IV antibiotics are to be given with induction and a regional block administered.
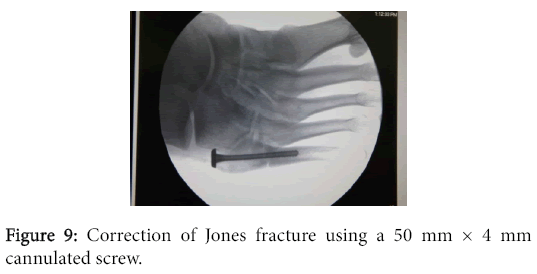
Under Fluoroscan control, a wire is introduced into the styloid of the fifth metatarsal. A percutaneous arthrotomy is performed at the 5th tarsometatarsal joint (Figure 8). A smooth guide wire is then introduced into the metatarsal styloid and passed down the barrel of the fifth metatarsal. The wire should be confirmed to be in the metatarsal on both AP and lateral views on fluoroscopy. A 4 mm incision is made based on the wire entry point. Then, a smooth cannulated drill is inserted and the metatarsal drilled across the fracture site.
Under power, a 50 mm × 4 mm cannulated screw needs to be inserted into the metatarsal and fracture closure with good fixation should be visualized (Figure 9). An injection with local anesthetic and steroid was administered with a 10 ml syringe spinal needle. Closure entails securing the wounds with a single Nylon stitch.
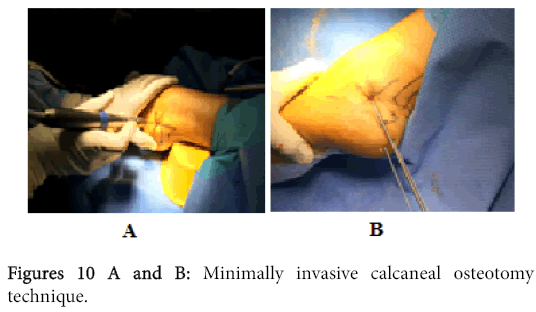
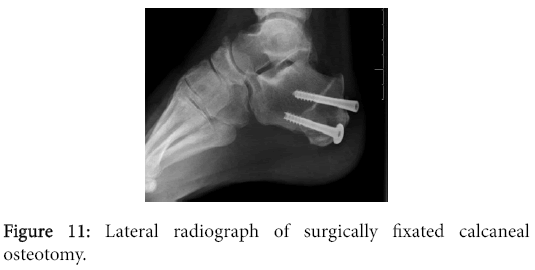
Cavus Foot
Minimally invasive heel shift is our preferred technique for addressing cavus foot (Figure 10A and 10B). This method may also be used in management of posterior tibialis failure. Our technique utilizes a 3 mm Chevron burr with the Surgipro drill system. First, the lateral wall is breached and the heel is divided in sequence beginning in a proximal direction and then in a distal direction. A freer is next introduced through the keyhole incision to ensure complete division at the calcaneus. A Steinmann pin is positioned into the lateral portal and the heel is moved 1 cm in a varus direction. Next, guide wires are introduced into the calcaneus from the posterior aspect of the heel. Fluoroscan is used throughout in order to confirm the positioning of the wires. Large 6.5 mm cannulated screws are inserted over the wires, gaining compression over the osteotomy site. Finally, the wires are removed and the heel shift is screened to ensure stability (Figure 11).
Discussion
Review of current literature suggests that our operative method has gained significant momentum over the last 5 years, and is now considered standard of care. With clinical evidence mounting, it is increasingly clear that adoption of arthroscopy as an adjunct to the modified Brostrom-Gould procedure generates optimal results while simultaneously minimizing post-surgical complications. However, the procedure has a number of limitations which if identified can either lead to modification of the technique or conduction of a different procedure. First, the peroneal tendon cavity is not routinely opened; if suspicious, an MRI scan should be performed. A tendon repair can be performed by changing to an incision, which traces the courses of the tendons. If the peroneal tendons are not working, a peroneal tendonesis procedure may be better to use as the repair will likely stretch out. The procedure did not produce the functional result in patients who had prior fractures of the ankle. Lastly, in returning the athlete back to sport a natural apprehension exists which may predispose to instability and potentially re-injury; this may require referral to a sports psychologist.
We have shown that our patients continue to have a high satisfaction rate at a ten-year follow-up and a low rate of reoccurrence. Recent studies support our hypothesis that implementation of arthroscopy in conjunction with minimally invasive anatomic repair provides excellent long-term outcomes.
References
- Colville MR (1995) Reconstruction of the lateral ankle ligaments. Instr Course Lect 44: 341-348.
- Acevedo JI, Mangone P (2015) Ankle instability and arthroscopic lateral ligament repair. Foot Ankle Clin 20: 59-69.
- Watson-Jones R (1974) The classic: "Fractures and Joint Injuries" by Sir Reginald Watson-Jones, taken from "Fractures and Joint Injuries," by Watson-Jones R (1955), Baltimore, Williams and Wilkins Company (4th edn).Clin Orthop Relat Res 2: 4-10.
- Nery C, Raduan F, Del Buono A, Asaumi ID, Cohen M, et al. (2011) Arthroscopic-assisted Broström-Gould for chronic ankle instability: a long-term follow-up. Am J Sports Med 39: 2381-2388.
- Slater GL, Pino AE, O'Malley M (2011) Delayed reconstruction of lateral complex structures of the ankle. World J Orthop 2: 31-36.
- Odak S, Ahluwalia R, Shivarathre DG, Mahmood A, Blucher N, et al. (2015) Arthroscopic Evaluation of Impingement and Osteochondral Lesions in Chronic Lateral Ankle Instability. Foot Ankle Int 36: 1045-1049.
- Acevedo JI, Ortiz C, Golano P, Nery C (2015) ArthroBroström Lateral Ankle Stabilization Technique: An Anatomic Study. Am J Sports Med 43: 2564-2571.
- Acevedo JI, Mangone P (2015) Arthroscopic brostrom technique. Foot Ankle Int 36: 465-473.
- Giannini S, Ruffilli A, Pagliazzi G, Mazzotti A, Evangelisti G, et al. (2015) Treatment algorithm for chronic lateral ankle instability. Muscles Ligaments Tendons J 4: 455-460.
- McCriskin BJ, Cameron KL, Orr JD, Waterman BR (2015) Management and prevention of acute and chronic lateral ankle instability in athletic patient populations. World J Orthop 6: 161-171.
- Portland G, Kelikian A, Kodros S (2003) Acute surgical management of Jones' fractures. Foot Ankle Int 24: 829-833.
- Broström L (1966) Sprained ankles. VI. Surgical treatment of "chronic" ligament ruptures. ActaChirScand 132: 551-565.
- White WJ, McCollum GA, Calder JD (2015) Return to sport following acute lateral ligament repair of the ankle in professional athletes. KneeSurg Sports TraumatolArthrosc.
- Hua Y, Chen S, Li Y, Chen J, Li H (2010) Combination of modified Brostrom procedure with ankle arthroscopy for chronic ankle instability accompanied by intra-articular symptoms. Arthroscopy: The Journal of Arthro and Rel Surg 26: 524-528.
- Guillo S, Cordier D, Sonnery-Cottet B, Bauer T (2014) Anatomical reconstruction of the anterior talofibular and calcaneofibular ligaments with an all-arthroscopic surgical technique. Orthop Traumatol Surg Res 100: 413-417.
- Lui TH (2015) Modified arthroscopic Brostrom procedure. Foot Ankle Surg 21: 216-219.
- Hsu AR, Ardoin GT2, Davis WH2, Anderson RB2 (2015) Intermediate and Long-Term Outcomes of the Modified Brostrom-Evans Procedure for Lateral Ankle Ligament Reconstruction. Foot Ankle Spec.
- Karlsson J, Bergsten T, Lansinger O, Peterson L (1988) Reconstruction of the lateral ligaments of the ankle for chronic lateral instability. J Bone Joint Surg Am 70: 581-588.
- Snook GA, Chrisman OD, Wilson TC (1985) Long-term results of the Chrisman-Snook operation for reconstruction of the lateral ligaments of the ankle. J Bone Joint Surg Am 67: 1-7.
- Hintermann B, Boss A, Schäfer D (2002) Arthroscopic findings in patients with chronic ankle instability. Am J Sports Med 30: 402-409.
- Liu SH, Baker CL (1994) Comparison of lateral ankle ligamentous reconstruction procedures. Am J Sports Med 22: 313-317.
- Gould N, Seligson D, Gassman J (1980) Early and late repair of lateral ligament of the ankle. Foot Ankle 1: 84-89.
- Hintermann B, Boss A, Schäfer D (2002) Arthroscopic findings in patients with chronic ankle instability. Am J Sports Med 30: 402-409.
- Cha SD, Kim HS, Chung ST, Yoo JH, Park JH,et al. (2012) Intra-articular Lesions in Chronic Lateral Ankle Instability: Comparison of Arthroscopy with Magnetic Resonance Imaging Findings. Clinics in Orthopedic Surgery. 4: 293-299.
- Smith TO, Clark A, Hing CB (2011) Interventions for treating proximal fifth metatarsal fractures in adults: a meta-analysis of the current evidence-base. Foot Ankle Surg 17: 300-307.
- Guillo S, Bauer T, Lee JW, Takao M, Kong SW, et al. (2013) Consensus in chronic ankle instability: Aetiology, assessment, surgical indications and place for arthroscopy. Orthopaedics & Traumatology: Surgery and Research 99: S411-S419.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 13714
- [From(publication date):
March-2016 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 12939
- PDF downloads : 775