Massachusetts Leads the Nation in Colorectal Cancer Screening: What Lessons can we learn for Implementing Prevention - Translating Epidemiology to Practice?
Received: 07-Feb-2013 / Accepted Date: 08-Feb-2013 / Published Date: 18-Feb-2013 DOI: 10.4172/2161-1165.1000e111
160252No heading
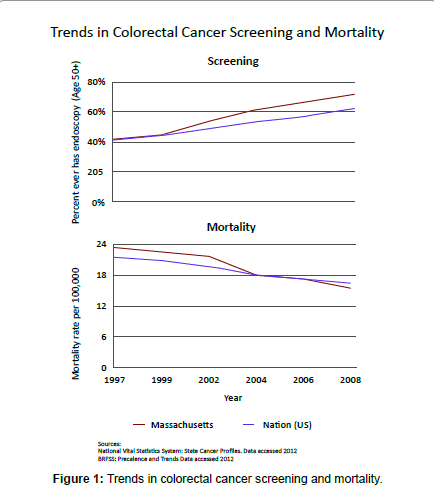
Over the past 15 to 20 years, colorectal cancer screening has gained increasing emphasis as a primary prevention strategy. Yet, the evolving science behind this strategy has been complicated by the range of screening tests available and varied public health approaches that would promote them. The inherent difficulty of building political will for a prevention strategy that, as Hemenway has described, has generally unknown beneficiaries further adds to the complexity of achieving effective and widespread screening [1]. Against this backdrop, Massachusetts has emerged as the state with both the highest rate of screening and the most dramatic decrease in colorectal cancer mortality over the past 15 years. Are there lessons we can draw from the Massachusetts experience and apply more broadly? The evidence on screening as an effective strategy to reduce colorectal cancer mortality has its roots in studies of Fecal Occult Blood Testing (FOBT) that showed a reduction in colorectal cancer mortality [2]. Initially, trials of fecal occult blood testing were published and prospective data from the Kaiser Permanente Health Plan confirmed benefits of screening, showing a reduction in colorectal cancer mortality. In 1997, the combined efforts of gastroenterologists and others led to the seminal paper by Winawer et al. recommending routine colorectal cancer screening [3]. The American Cancer Society followed suit with similar guidelines, and the U.S. Congress subsequently approved screening for colorectal cancer to be covered under Medicare. In Massachusetts, the move from evidence and recommendations to action hinged on a sustained social strategy, described best by the “collective impact approach,” which includes a common agenda, shared measurement system, mutually reinforcing activities, continuous communication and a backbone support organization [4]. Created in 1997, the efforts of the Massachusetts Colorectal Cancer Work Group met most of these criteria. The Work Group consisted of our interdisciplinary Harvard Center for Cancer Prevention along with the Massachusetts Department of Public Health, American Cancer Society, Massachusetts Medical Society, health insurers, medical centers, and other medical and public health schools – all with a common goal of increasing screening for colorectal cancer in Massachusetts. Coordinated efforts of the Work Group members spread across a range of opinion leaders and gatekeepers. Working closely with the American Cancer Society New England Division, which promoted screening throughout New England, the Harvard Center for Cancer Prevention worked to promote screening through educational and outreach activities to providers and communities. We also worked to present the case for colorectal screening to legislators and policy leaders from across New England emphasizing the potential for colorectal cancer screening to reduce mortality. In line with an initial plan summarized by Evjy, then President-elect of the Massachusetts Medical Society, the Work Group’s other coordinated efforts included systems level interventions in HMOs, and building public awareness of the benefits of screening and prevention of colorectal cancer [5]. As these efforts were developed and sustained, colorectal cancer has significantly declined as a cause of death in Massachusetts (Figure 1 and Table 1). The incidence dropped from an age-standardized rate of 27 deaths/100,000 in 1994 to 15.4 deaths/100,000 in 2008. This significant and substantial 35 percent reduction in mortality is a testament to the impact of widespread screening. Over the same timeframe, the proportion of the population screened in Massachusetts rose from 41 percent in 1997 to 61 percent in 2004 and has continued to increase up to 75 percent in 2010. This was the highest prevalence of colorectal screening in the nation [6]. Promoting population health through reduction in colorectal cancer mortality requires successfully moving from knowledge through translation to implementation in widespread practice. Preventive action usually lags behind the science. In the setting of colorectal cancer – the second leading cause of cancer mortality – screening within the United States has substantial variation in the rate of uptake and the corresponding decline in mortality. For example, rates of screening by 2010 varied from 54 percent to 59 percent in the bottom quartile of states to 70 percent to 75 percent in New England, Maryland, and Washington State [6]. The overall national average of 64 percent exceeds the American Cancer Society challenge goals of 55 percent by 2010. National changes in access through Medicare coverage and in professional awareness through publication of prevention guidelines recommending screening alone do not speed translation to practice. Implementation research must be active and support movement of evidence-based effective health care and prevention strategies or programs from the clinical or public health knowledge base into routine use. While research components building the knowledge base focus more on advancing the scientific evidence and adjusting programs to meet needs of specific populations, the overall implementation in Massachusetts proceeded as a combined effort engaging resources of the state department of public health, American Cancer Society, academics, and many other related groups. While numerous components of implementation may occur within health systems, the promotion of colorectal cancer prevention and screening spans far beyond provider systems and insurance providers. Other successful primary prevention programs such as in Australia to reduce sun exposure, increase awareness among providers, and reduce melanoma mortality and also illustrate the need for public health prevention efforts to embrace providers, community awareness, and regulatory changes. The melanoma prevention program there has evolved over time, yet core elements remain unchanged after more than 30 years. Can we sustain a program in colorectal cancer screening for this duration? A question that, perhaps, highlights one of the biggest barriers to broadly implementing programs similar to those in Massachusetts: the variable funding for state public health community education and annual funding cycles for CDC funds to support promotion of colorectal screening. To this day, CDC still only funds about half of all states to promote colorectal cancer screening. Public health programs often do not communicate the successes of prevention, largely due to the nature of their benefits. Lowered rates of disease take time to document and often lack emotional appeal – at least to the population at large. This contrasts with treatment, where patient advocates, often as survivors, voice their own demand for services. Thus, resource allocation has greater pull for treatment and access to treatment than may be sustained for prevention programs. Yet, we have seen a national reduction in colorectal cancer mortality of over 27% in the period 1994 to 2007, with the leading states having a 37% decrease in mortality. Comprehensive prevention programs clearly work. As a nation we are on track and may already have exceeded the American Cancer Society goal of 22 to 33% mortality reduction by 2015. This is consistent with estimates that screening and lifestyle changes provide far greater population health benefits than advances in treatment of colorectal cancer [7]. Future programs might benefit from greater resource allocation to better quantify those components that are most effective and to relate intermediate measures of progress in the implementation to the disease outcome pathway. Improved strategies to quantify success and synthesize evidence of success in prevention may help sustain political will for cancer prevention. Implementing a broad range of strategies already known to be effective can further speed reduction in colorectal cancer mortality. The Massachusetts colorectal screening experience suggests success of a broadly supported and widespread effort of multiple organizations and disciplines [4]. It is a coordinated approach involving substantial effort but is one that could, if adopted more often, bring greater success and greater awareness to other important public health issues of our day.
| Year | 1997 | 1999 | 2002 | 2004 | 2006 | 2008 |
| Screening Mass | 0.413 | 0.44 | 0.534 | 0.612 | 0.663 | 0.714 |
| Screening Nat | 0.41 | 0.439 | 0.486 | 0.535 | 0.571 | 0.622 |
| Mort Mass | 23.4 | 22.5 | 21.6 | 18 | 17.1 | 15.4 |
| Mort Nat | 21.5 | 20.9 | 19.7 | 18 | 17.2 | 16.4 |
Table 1: Trends in colorectal cancer screening and mortality.
References
- Hemenway D (2010) Why we don't spend enough on public health. N Engl J Med 362: 1657-1658.
- Mandel JS, Bond JH, Church TR, Snover DC, Bradley GM, et al. (1993) Reducing mortality from colorectal cancer by screening for fecal occult blood. Minnesota Colon Cancer Control Study. N Engl J Med 328: 1365-1371.
- Winawer SJ, Fletcher RH, Miller L, Godlee F, Stolar MH, et al. (1997) Colorectal cancer screening: clinical guidelines and rationale. Gastroenterology 112: 594-642.
- Kania J, Kramer M (2011) Collective Impact. In: Stanford Social Innovation Review. Winter 2011.
- Joseph DA, King JB, Miller JW, Richardson LC (2012) Prevalence of colorectal cancer screening among adults--behavioural risk factor surveillance system, United States, 2010. MMWR Morb Mortal Wkly Rep 61: 51-56.
- Edwards BK, Ward E, Kohler BA, Eheman C, Zauber AG, et al. (2010) Annual report to the nation on the status of cancer, 1975-2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer 116: 544-573.
Citation: Colditz GA, Hank Dart SM (2013) Massachusetts Leads the Nation in Colorectal Cancer Screening: What Lessons can we learn for Implementing Prevention - Translating Epidemiology to Practice? Epidemiol 3:e111. DOI: 10.4172/2161-1165.1000e111
Copyright: © 2013 Colditz GA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 14427
- [From(publication date): 4-2013 - Dec 23, 2024]
- Breakdown by view type
- HTML page views: 9858
- PDF downloads: 4569